Abstract
Purpose
Sinus elevation procedures have become a routine and reliable way to gain bone volume in the edentulous maxilla for dental implant placement. Presence of bony septations and pathology in the maxillary sinus often cause complications leading to graft or implant failure or both. The aim of this study was to retrospectively evaluate the prevalence of pathology, direction of the septa, and sinus width measured at 2 mm, 5 mm, and 10 mm from the sinus floor in maxillary sinuses using cone-beam computed tomography (CBCT).
Materials and Methods
Seventy-two sinuses from 36 random preoperative CBCT scans referred for implant therapy were retrospectively evaluated for the number, prevalence, and direction of bony septations and presence of pathology. Width of the sinus was also measured at 2 mm, 5 mm, and 10 mm from the sinus floor to account for the amount of bone available for implant placement.
Results
Maxillary sinus septa were found in 59.7%. Presence of a single septum was noted in 20 sinuses (27.7%), followed by two septa in 17 sinuses. The most common direction of the septum was the transverse direction. Retention pseudocyst and mucosal thickening were the most commonly seen abnormality/pathology.
Implant-supported restorations are increasingly becoming the option of choice for restoring missing teeth due to their high rate of documented success.1 However, implant placement can be challenging, especially in the posterior maxilla, due to poor bone quality and the dual-pattern resorption of maxillary alveolar bone.2 According to Wolff's law, tooth loss leads to disuse atrophy and trabecular bone adaptation resulting in marked alveolar bone resorption.3 In addition to alveolar bone resorption, bone volume is further compromised due to the continuous pneumatization of the maxillary sinus.4
The edentulous posterior maxilla with extensive bone resorption and sinus pneumatization requires prior augmentation of bone volume to facilitate dental implant placement and to increase the chances of long term success. This has been reported to be achievable with sinus elevation procedures to create bone for implants using the crestal osteotome approach or lateral window approach with or without the use of biomaterials.5678910 The newly gained bone provides sufficient primary stability, and it has been shown that osseo-integration can predictably be achieved with a high implant survival rate ranging between 61.7% and 100%, with the average survival rate of all interventions being 92.6%.11 The clinical success and or survival (≤3 years) of implants placed with an osteotome sinus floor elevation technique have been reported to be similar to that of implants conventionally placed in the partially edentulous maxilla, making it a very reliable option to gain bone volume.12
However, sinus augmentation procedures are not only technique sensitive but are also prone to complications if a thorough preoperative evaluation is not performed.1314151617 In developing any treatment plan for rehabilitation of the edentulous posterior maxilla with implant-supported prostheses, sound knowledge of the anatomy and common variations, patency, and health of the maxillary sinus must be carefully considered. Diagnostic imaging with traditional two-dimensional (2D) radiographic methods using panoramic radiographs and intraoral radiographs plays a crucial role but does not yield three-dimensional (3D) information of the area of interest. The introduction of CBCT has changed the imaging paradigm in preoperative treatment planning for implants. Several studies have shown that CBCT can play a vital role in providing reliable information like available bone height, presence of pathology, and number and location of bony septations when present, and can also aid in preoperative implant planning.45678181920212223 Encountering unexpected complications during sinus elevation surgery can often jeopardize the final outcome of the bone graft and implant placement itself, also at times leading to serious sino-nasal complications. Sinus membrane perforation has been reported to be the most common (7-44% occurrence) of the intraoperative complications. Other post-operative complications like nasal bleeding, sinus infection, and barrier membrane or graft exposure are less common.2223242526
Factors that can increase the risk of the chance of Schneiderian membrane perforation include anatomical variations, presence of septa, previous sinus infection or surgery, and surgeon's experience.182122 Anatomical factors consist of residual alveolar height, bone density, maxillary sinus septa, and morphology of the sinus floor.2310161718 Maxillary sinus septa have been reported to occur in 13%-35% of maxillary sinuses.20 The presence of septa has been implicated as a potential cause for perforation during sinus elevation surgery.21222324252627 Thus the information on the prevalence, location, and direction of the septa as well as the presence of pathology at the base of the sinus would help patients and their doctors better appreciate the risks associated with surgery in that region. Careful preoperative assessment of the presence of anatomical variations, pathology, and 3D evaluation, especially at the base of the maxillary sinus with CBCT can help in better planning the procedure and aid the clinician in mitigating the chances of surgical complications.
The aim of this study was to retrospectively determine the prevalence of pathology, prevalence, and direction of bony septae in the maxillary sinus and to correlate these measures with age and gender by using CBCT. The dimensions of the maxillary sinus were evaluated at 2 mm, 5 mm, and 10 mm from the sinus floor. The clinical significance of this study and its measurements should help the clinician in understanding the width of the sinus at the most commonly augmented heights, which will suggest the amount of bone graft material and membrane needed for the procedure. Understanding the prevalence of septations will help in anticipating this potential complication and establishing a treatment plan that accounts for the presence of the septa and the increased time necessary to manage this complication if it were in the area of interest for augmentation.
This retrospective study evaluated a randomly selected sample of 36 CBCT volumes acquired at the University of Connecticut Health Center's Oral and Maxillofacial Radiology Clinic between January 2008 and June 2013. Patients who were referred for dental implant therapy were imaged with a CBCT scan that did not show any patient motion or metallic artifacts that rendered the scans non-diagnostic were included. CBCT scans that did not have the entire sino-nasal complex in the field of view, CBCT scans that had patient movement. CBCT scans that had metallic artifacts from dental restorations that would make it challenging to evaluate the maxillary sinus for the presence of pathology when present and make height/width measurements were excluded from the study. The study was approved by the Institutional Review Board (IRB) and the local ethics committee (IRB number: 13-174-1).
The exams were performed using a CBCT unit (CB MercuRay, Hitachi Medical Systems, Kyoto, Japan). The acquisition specifications were a 6-inch field-of-view (FOV) scan covering the maxillary region including the maxillary sinuses, with a voxel size of 0.2 mm and a scan time of 10 seconds. Operating parameters were set at 120 kVp and 15 mA. The images were visualized using a 22 inch HP Compaq LA2205wg screen (HP Corporation, Palo Alto, CA, USA) with a resolution of 1680×1050; 1.8 MP. A CB Works version 3.0 (Cybermed, Seoul, Korea), a DICOM viewing software program, was used to analyze the images. The images were reconstructed with a slice thickness of 0.5 mm and a slice interval of 1.5 mm.
The CBCT images were evaluated by a radiology resident and a periodontology resident under the guidance of a board certified oral and maxillofacial radiologist. There was a calibration session prior to initiation of image evaluation to understand the purpose of the study and a training session was conducted to understand the various functions of the reconstruction software. The prevalence, number, and direction of the septum were measured on the coronal, sagittal, and axial planes (Fig. 1). The presence of any pathological/abnormal landmarks was also investigated. In addition, the presence or absence of the posterior teeth (first and second premolars, and molars) was evaluated. The maximum anterio-posterior dimension at the levels of 2 mm, 5 mm, and 10 mm and the height cranial to the floor of the sinus were measured on the coronal, sagittal, and axial images (Fig. 2). The maximum disto-medial dimension at the 2-mm, 5-mm, and 10-mm levels were measured. Based on the direction of the septa with reference to the floor of the sinus, the septa were marked in the transverse sagittal and horizontal directions. Although all septa did not exactly follow these specific directions, they were judged and marked based the closest direction to their orientation. Descriptive statistical analysis was used, including mean, range, and standard deviation.
This cross-sectional study consisted of 36 patients (72 bilateral maxillary sinuses) with a mean age of 53.2 years (range of 31 to 85 years). The male to female ratio was 19 to 17 with males accounting for 52.8% and females 47.2%. The posterior teeth in this study were defined as premolars and molars, with the exception of the third molars. The mean percentage of the presence of erupted premolars and molars at the time of evaluation was 57.0% (±0.5) distributed on both sides as follows: 56.0% (±0.4) on the right and 58.0% (±0.4) on the left side.
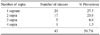
Maxillary sinus septa were found in 59.7% of the 72 sinuses; that is, 20 sinuses (27.7%) showed a single septum, followed by 2 septa in 17 sinuses (23.6%), and 3 septa in 5 sinuses (6.9%), and in one particular sinus in the sample, 4 septations were recognized (1.3%) (Table 1). In total, 73 septa were found from 72 maxillary sinuses.
The most common direction of the septum in the sinus was found to be the transverse direction, which existed in 51 septa (70.8%), followed by the sagittal direction in 17 septa (23.6%), and the least common was the horizontally oriented septa, which are found in 5 septa (6.9%).
Abnormalities were found in 23 sinuses (31.9%), 9 of which were in the right sinus (25.0% of the patients) and 14 in the left sinus (39.0% of the patients). The most common abnormality was mucus retention pseudocyst, which accounted for 17 cases, which was 74% of the abnormalities, followed by mucosal thickening, which accounted for 3 cases (13%). Other abnormalities were recognized less commonly, and those included 1 metastatic lesion, 1 keratocystic odontogenic tumor, and 1 antrochoanal polyp (Table 2).
At the level of 2 mm cranial to the floor of the sinus, the mean anterio-posterior dimension was found to be 15.3±5.6 mm, with a range of 5.1 mm to 29.4 mm. On the other hand, the disto-medial dimension at this level was found to be 10.2±3.9 mm with a range of 5.4 mm to 30.8 mm. While at the level of 5 mm cranial to the floor of the sinus, the mean anterio-posterior dimension was found to be 24.1±6.1 mm with a range of 10 mm to 39 mm and the disto-medial dimension was found to be 14.5±4.1 mm, with a range of 2.2 mm to 31.6 mm. In addition, at the level of 10 mm cranial to the floor of the sinus, the mean anterio-posterior dimension was found to be 31.8±4.1 mm, with a range of 18.7 mm to 47.5 mm, and the disto-medial dimension at the same level was found to be 19.5±4.1 mm, with a range of 11.9 mm to 36.3 mm (Table 3)
The maximum dimensions of the sinuses were measured in three dimensions, including the antero-posterior, disto-medial (medio-lateral), and cranio-caudal dimensions. In the antero-posterior dimension, the mean distance was found to be 38.2±3.5 mm, with a range of 28.3 mm to 48.5 mm. While in the disto-medial dimension, the mean distance was found to be 27.3±4.4 mm with a range of 18.1 mm to 44.2 mm. Finally, the cranio-caudal dimension was measured to be 36.3±4.7 mm, with a range of 23.1 mm to 45 mm (Table 4).
There was no significant difference between the prevalence of the septa between the right and left sides, according to the age and sex of the patient, or by average sinus dimensions.
Various studies have reported on the prevalence, direction, and location of septa with a range of percentages. The clinical prevalence of septa reported in various studies accounts for up to 57.6% of maxillary sinuses based on clinical and radiological examination.20 Gosau et al.28 stated that most septa are present in the posterior region. Ulm et al.29 claimed conversely that most are in the anterior, while Velasquez-Plata et al.30 and Gonzalez-Santana et al.31 described them to be prevalent in the middle region. Since no consensus has emerged on the location and prevalence, we tailored this study to address this question with a reasonably large sample size.
The total prevalence of radiographically detected septa described in this study appears to be the highest reported in the literature so far. The maxillary sinus septa were found in 59.7% (50.0% of right sinuses; 69.4% of left sinuses) (Table 1). A single septum was most frequently recognized in 20 sinuses (27.7%), followed by two septa in 17 sinuses (23.6%), and three septa in 5 sinuses (6.9%), and in a single sinus there was 4 septa (1.3%).
The most common direction of the septum in the sinus was found to be the transverse direction, and this orientation occurred in 51 septa (70.0%), followed by the sagittal direction in 17 septa (23.3%), and least common was the horizontally oriented septa, which are found in 5 septa (6.9%). The lower rate of prevalence reported in previous studies might be a result of diagnosis of the sinus septa using 2D panoramic radiographs. Sinus septa showing a sagittal orientation might not have been diagnosable at all using panoramic radiographs and thus led to the false assumption of narrow internal sinus anatomy and subsequent non-augmentation of the medial portion of the sinus cavity.203032
The high correlation of the values between the reported clinical prevalence and radiological prevalence of septa obtained in this study highlighted the ability of high spatial resolution CBCT in evaluating anatomy or septa.20 Furthermore, 31.9% of the sinuses showed the presence of abnormalities, with mucus retention cyst (17 cases in 74.0% of the abnormalities) being the most common abnormality to be found, followed by periosteal thickening (3 cases in 13.0% of the abnormalities). Other less commonly recognized abnormalities were metastatic lesion, keratocystic odontogenic tumor, and antrochoanal polyp.
The dimensions of the maxillary sinus in anterio-posterior, disto-medial, and cranio-caudal planes were evaluated at the levels 2 mm, 5 mm, and 10 mm cranial to the sinus floor. This was predominantly the area of interest during sinus elevation in most clinical situations, and elevation was obtained ranging from a minimum of 2 mm to a maximum of 10 mm, with 5 mm routinely. Thus, the presence or absence of septa and pathology in this region would be of particular interest to the clinician. This might dictate a different approach in case of sinus floor augmentation ranging from modification in the surgical access strategy (or window design) to a change in implant positions or total avoidance of bone augmentation procedures. During the lateral window approach, the direct visualization of the sinus membrane within the sinus would be limited or compromised due to the nature of the surgical site and challenges of the surgery. The pre-operative three-dimensional radiographic analyses would help the clinician estimate the amount of elevation needed in the medio-lateral dimension, thus minimizing or even preventing augmentation of the medial portion of the sinus and its effect on implant placement. There was no significant difference between the prevalence of septa between the right and left sides, or by the age and sex of the patient.
Different radiographic techniques for evaluation of the maxillary sinus septa include standard oral radiography, panoramic radiography, and CBCT scans. Panoramic radiography may lead to a misdiagnosis of sinus septa about 12-44% of the time because it is difficult to identify the overlapping anatomic structures due to superimposition. 2032 In contrast, CBCT allows high-resolution images of delicate bony structures. CBCT does not have the inherent problem of superimposition and magnification, and it helps in visualizing the craniofacial structures with more precision than the 2D conventional methods. Therefore, CBCT may be considered the 3D method of choice for visualization of the antral septa. Perpendicular to the orientation of the maxillary septa, an axial image can be considered the optimal sectional plane for revelation of bony variation.1518 For accurate diagnosis and treatment planning, CBCT scans may be a very useful diagnostic tool to avoid or at least minimize complications.
Further studies may be necessary in the future to evaluate the correlation between the orientation of the septa and rate of complications in the outcome of a sinus augmentation surgical procedure for implant placement. Based on the results of this study, it can be concluded that the prevalence of bony septa and presence of sinus pathology in the maxillary sinus is very high in the population we studied, and preoperative imaging of the maxillary sinus using CBCT can be a very useful aid in planning sinus augmentation procedures for dental implant therapy.
Figures and Tables
Fig. 2
A. Maximum disto-medial dimension is measured at 10 mm cranial to the floor of the sinus in coronal section. B. Maximum antero-posterior dimensions at 10 mm cranial to the floor of the sinus is measured on the sagittal section. C. Maximum width at 10 mm cranial to the floor of the sinus is measured in axial section.

References
1. Tadinada A, Fung K, Thacker S, Mahdian M, Jadhav A, Schincaglia GP. Radiographic evaluation of the maxillary sinus prior to dental implant therapy: a comparison between two-dimensional and three-dimensional radiographic imaging. Imaging Sci Dent. 2015; 45:169–174.

2. Balshi TJ, Wolfinger GJ. Management of the posterior maxilla in the compromised patient: historical, current, and future perspectives. Periodontol 2000. 2003; 33:67–81.

3. Chappard D, Baslé MF, Legrand E, Audran M. Trabecular bone microarchitecture: a review. Morphologie. 2008; 92:162–170.

4. Sharan A, Madjar D. Maxillary sinus pneumatization following extractions: a radiographic study. Int J Oral Maxillofac Implants. 2008; 23:48–56.
5. Raghoebar GM, Timmenga NM, Reintsema H, Stegenga B, Vissink A. Maxillary bone grafting for the insertion of endosseous implants: results after 12-124 months. Clin Oral Implants Res. 2001; 12:279–286.
6. Peleg M, Garg AK, Mazor Z. Predictability of simultaneous implant placement in the severely atrophic posterior maxilla: a 9-year longitudinal experience study of 2132 implants placed into 731 human sinus grafts. Int J Oral Maxillofac Implants. 2006; 21:94–102.

7. Nedir R, Nurdin N, Vazquez L, Szmukler-Moncler S, Bischof M, Bernard JP. Osteotome sinus floor elevation technique without grafting: a 5-year prospective study. J Clin Periodontol. 2010; 37:1023–1028.

8. Blus C, Szmukler-Moncler S, Salama M, Salama H, Garber D. Sinus bone grafting procedures using ultrasonic bone surgery: 5-year experience. Int J Periodontics Restorative Dent. 2008; 28:221–229.
9. Pjetursson BE, Tan WC, Zwahlen M, Lang NP. A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevation. J Clin Periodontol. 2008; 35:8 Suppl. 216–240.

10. Bornstein MM, Chappuis V, von Arx T, Buser D. Performance of dental implants after staged sinus floor elevation procedures: 5-year results of a prospective study in partially edentulous patients. Clin Oral Implants Res. 2008; 19:1034–1043.

11. Wallace SS, Froum SJ. Effect of maxillary sinus augmentation on the survival of endosseous dental implants. A systematic review. Ann Periodontol. 2003; 8:328–343.

12. Emmerich D, Att W, Stappert C. Sinus floor elevation using osteotomes: a systematic review and meta-analysis. J Periodontol. 2005; 76:1237–1251.

13. Galindo-Moreno P, Avila G, Fernández-Barbero JE, Aguilar M, Sánchez-Fernández E, Cutando A, et al. Evaluation of sinus floor elevation using a composite bone graft mixture. Clin Oral Implants Res. 2007; 18:376–382.

14. Marino MJ, Weinstein JE, Riley CA, Levy JM, Emerson NA, McCoul ED. Assessment of pneumatization of the paranasal sinuses: a comprehensive and validated metric. Int Forum Allergy Rhinol. 2016; 6:429–436.

15. Yoo JY, Pi SH, Kim YS, Jeong SN, You HK. Healing pattern of the mucous membrane after tooth extraction in the maxillary sinus. J Periodontal Implant Sci. 2011; 41:23–29.

16. Tiwana PS, Kushner GM, Haug RH. Maxillary sinus augmentation. Dent Clin North Am. 2006; 50:409–424.

17. Testori T, Weinstein RL, Taschieri S, Del Fabbro M. Risk factor analysis following maxillary sinus augmentation: a retrospective multicenter study. Int J Oral Maxillofac Implants. 2012; 27:1170–1176.
18. Kennedy DW, Zinreich SJ, Rosenbaum AE, Johns ME. Functional endoscopic sinus surgery. Theory and diagnostic evaluation. Arch Otolaryngol. 1985; 111:576–582.

19. Mafee MF, Chow JM, Meyers R. Functional endoscopic sinus surgery: anatomy, CT screening, indications, and complications. AJR Am J Roentgenol. 1993; 160:735–744.

20. Maestre-Ferrín L, Galán-Gil S, Rubio-Serrano M, Peñarrocha-Diago M, Peñarrocha-Oltra D. Maxillary sinus septa: a systematic review. Med Oral Patol Oral Cir Bucal. 2010; 15:e383–e386.
21. Wen SC, Chan HL, Wang HL. Classification and management of antral septa for maxillary sinus augmentation. Int J Periodontics Restorative Dent. 2013; 33:509–517.

22. Călin C, Petre A, Drafta S. Osteotome-mediated sinus floor elevation: a systematic review and meta-analysis. Int J Oral Maxillofac Implants. 2014; 29:558–576.

23. Benavides E, Rios HF, Ganz SD, An CH, Resnik R, Reardon GT, et al. Use of cone beam computed tomography in implant dentistry: the International Congress of Oral Implantologists consensus report. Implant Dent. 2012; 21:78–86.
24. Schwartz-Arad D, Herzberg R, Dolev E. The prevalence of surgical complications of the sinus graft procedure and their impact on implant survival. J Periodontol. 2004; 75:511–516.

25. Barone A, Santini S, Sbordone L, Crespi R, Covani U. A clinical study of the outcomes and complications associated with maxillary sinus augmentation. Int J Oral Maxillofac Implants. 2006; 21:81–85.
26. Ziccardi VB, Betts NJ. Complications of maxillary sinus augmentation. In : Jensen OT, editor. The sinus bone graft. Chicago, IL: Quintessence;1999. p. 201–208.
27. Regev E, Smith RA, Perrott DH, Pogrel MA. Maxillary sinus complications related to endosseous implants. Int J Oral Maxillofac Implants. 1995; 10:451–461.
28. Gosau M, Rink D, Driemel O, Draenert FG. Maxillary sinus anatomy: a cadaveric study with clinical implications. Anat Rec (Hoboken). 2009; 292:352–354.

29. Ulm CW, Solar P, Krennmair G, Matejka M, Watzek G. Incidence and suggested surgical management of septa in sinus-lift procedures. Int J Oral Maxillofac Implants. 1995; 10:462–465.
30. Velásquez-Plata D, Hovey LR, Peach CC, Alder ME. Maxillary sinus septa: a 3-dimensional computerized tomographic scan analysis. Int J Oral Maxillofac Implants. 2002; 17:854–860.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download