Abstract
Purpose
This study was performed to evaluate the relationship between pterygoid plate asymmetry and temporomandibular joint disorders.
Materials and Methods
Cone-beam computed tomography (CBCT) images of 60 patients with temporomandibular disorders (TMD) involving pain were analyzed and compared with images of 60 age- and gender-matched controls. Three observers performed linear measurements of the lateral pterygoid plates.
Results
Statistically significant differences were found between measurements of the lateral pterygoid plates on the site that had pain and the contralateral site (p<0.05). The average length of the lateral pterygoid plates (LPPs) in patients with TMD was 17.01±3.64 mm on the right side and 16.21±3.51 mm on the left side, and in patients without TMD, it was 11.86±1.97 mm on the right side and 11.98±1.85 mm on the left side. Statistically significant differences in the LPP length, measured on CBCT, were found between patients with and without TMD (p<0.05). The inter-examiner reliability obtained in this study was very high for all the examiners (0.99, 95% confidence interval: 0.98-0.99).
Temporomandibular disorder (TMD) is a clinical term used to describe musculoskeletal disorders affecting the temporomandibular joints (TMJs) and their associated musculature.1 Pain in the TMJ and/or jaw muscles is one of the defining features of TMD and the primary reason for seeking care.
The lateral pterygoid plate (LPP) is thought to play an important role in the control of jaw movement2 because of the presence of abnormal patterns of lateral pterygoid muscle activity in some TMD patients.34 If the LPP is involved in the etiology of some of the signs and symptoms of TMD, then visualizing the direct action of the muscle on bony attachments with cone-beam computed tomography (CBCT) imaging might be of interest.
Jaw muscles are versatile entities capable of changing their size, cross-sectional area, and fiber properties to adapt to changing functional demands.5 The lateral pterygoid muscle consists of a superior head and a lower or inferior head. Classically, the inferior head is said to be active during jaw opening, jaw protrusion, and contralateral jaw movements and arises from the lateral surface of the LPP. Its fibers pass horizontally backward and laterally, to be inserted into a depression in front of the neck of the condyle of the mandible, and into the front margin of the articular disk.6
Even if there are reports on an association between TMJ pain and the lateral pterygoid muscles, to the best of our knowledge, the relationship between LPP asymmetry and jaw muscle pain has not been described as yet. Therefore, the overall aim was to evaluate a potential relationship between pterygoid plate asymmetry and the occurrence of TMD by comparing LPP measurements.
This study was approved by the Ethics Committee of Cayetano Heredia Peruvian University under the number SIDISI 57819. This was a case-control study comparing dual independent data and match-paired data. It was conducted from October 2010 to November 2013. TMD diagnoses were performed by a TMD specialist on the basis of the Research Diagnostic Criteria (RDC/TMD).7 The RDC/TMD guidelines provide standardized criteria for a two-axis diagnosis.
Sample size calculation considering the mean differences was applied; the sampling was not probabilistic and consisted of 60 patients with TMD on the right or the left side and referred by a TMD specialist and 60 age- and gender-matched controls referred by the Imagenes Cone Beam CT Diagnostic Center, Lima, Peru. All patients were divided into five age groups according their ages at onset: (1) young group (<20 years), (2) young adult group (21-30 years), (3) adult group (31-40 years), (4) pre-elderly group (41-50 years), and (5) elderly group (>51 years).
Patients were informed about the project, and they consented to participate in the study. The control group was obtained from the Imagenes Cone Beam CT Diagnostic Center database, taking into consideration factors such as age, sex, and images with a similar scanned area for the analysis of the pterygoid plate for sample homogenization.
CBCT was performed using i-CAT® (Imaging Sciences International, Hatfield, PA, USA). The operating parameters were obtained at 120 kV and 23.87 mAs with a typical voxel size of 0.25 mm. Images were viewed on a Dell Precision® Display (1920×1200 pixels) (Dell Inc., Round Rock, TX, USA). Two training sessions were organized prior to the final observations for the calibration of the observers. To ensure that the analyses were performed as usual by the specialists, the observers were blinded to the fact that the analyses were part of a study.
For visualizing the cases, the ICAT Vision™ i-CAT software was used (Imaging Sciences International, Hatfield, PA, USA). Measurement tools were used for assessing the length of the LPP. The slice thickness was 0.4 mm. Further, the multiplanar reformation display was explored. Three observers evaluated all images independently and made linear measurements of the pterygoid plates in an axial view, referring to the coronal and sagittal view. First, the midsagittal plane and the nasal cavity floor plane were selected on the coronal view (Fig. 1). Second, the midsagittal plane and the long axis of the palatal plane were selected on the sagittal view in order to obtain a proper axial view of the outer wings of the bilateral pterygoid tubercle (Fig. 2). Measurements were made from the distal point of the lateral pterygoid plate to the medial and lateral pterygoid plate junction (Fig. 3).
The collected data were statistically analyzed using IBM SPSS for Windows version 19 (IBM Corp., Armonk, NY, USA). Descriptive statistics were used to summarize all measurements that were considered to have a normal distribution (Kolmogorov-Smirnoff test p>0.05). The results of the measurements of the LPP on the site that had TMD and a contralateral site were compared using a paired t-test, and the measurements of the LPP on the site that had TMD and in the control group were compared by an independent t-test. The p values of less than 0.05 were considered statistically significant. The intra-class correlation coefficient (ICC) was also calculated for determining the inter- and intra-observer agreement. The results of the three examiners were compared by means of two-way mixed-effect ICCs. ICC values ranged from 0 to 1. ICCs were interpreted as follows: 0.00 to 0.25=little, if any, correlation; 0.26 to 0.49=low correlation; 0.50 to 0.69 =moderate correlation; 0.70 to 0.89=high correlation; and 0.90 to 1=very high correlation. An average of the three measurements was used for further analysis.
One hundred twenty CBCT scans were analyzed. The 60 patients without TMD constituted an age- and gender-matched control group. This produced a homogeneous sample. The mean age of the patients with TMD was 40.10±15.43 years (age range: 15-74 years), while the mean age of the patients without TMD was 40.02±15.38 years (age range: 15-74 years).
The average length of LPP in patients with TMD was 17.01±3.64 mm on the right side and 16.21±3.51 mm on the left side, and in patients without TMD, it was 11.86±1.97 mm on the right side and 11.98±1.85 mm on the left side. There were statistically significant differences between measurements of the LPP on the site that had TMD and the contralateral site on both the right side (p<0.05) and the left side (p<0.05) (Table 1).
The average length of LPP in the group of patients under 20 years with TMD was 16.35±4.53 mm on the right side and 15.78±3.07 mm on the left side, and in patients without TMD, it was 12.39±2.55 mm on the right side and 12.28±2.29 mm on the left side. When comparing the LPP length between patients with and without TMD under 20 years of age (14 patients), no statistically significant differences were found on the right side (p>0.05); however, on the left side, there were statistically significant differences (p<0.05).
Another group of patients considered for the analysis were young adults (22 patients). The average length of LPP in this group with TMD was 16.27±3.68 mm on the right side and 16.44±2.97 mm on the left side, and in patients without TMD was 12.70±2.13 mm on the right side and 12.84±2.30 mm on the left side (Fig. 4). Statistically significant differences were found on the right side (p<0.05) and the left side (p<0.05) between measurements of the LPP on the site that had TMD and the contralateral site.
The same statistically significant difference was seen on the right side (p<0.05) and the left side (p<0.05) in the adult group (30 patients). An average LPP length of 16.12±2.36 mm on the right side and 16.63±4.06 mm on the left side was found in the group with TMD, and of 11.72±2.04 mm on the right side and 11.84±1.77 mm on the left side in patients without TMD. Moreover, statistically significant differences were found in the pre-elderly (26 patients) and elderly (28 patients) groups (Table 2).
The mean length of the LPP in patients with TMD and pain on the right side was 18.58±3.32 mm and that for patients with TMD and pain on the left side was 14.65±3.28 mm. A statistically significant relationship was found between the length of the right LPP and pain on the same side (p<0.05). Furthermore, a statistically significant relationship was also found for the same variables on the left side. A length of 18.3±3.38 mm on this side and 15.14±3.21 mm on the right side was found.
Inter-examiner reliability showed a very high ICC for all the examiners (0.99, 95% confidence interval (CI): 0.98-0.99). An average of the three measurements was used for further analysis.
It has been widely accepted that TMDs are a set of disorders affecting the stomatognathic system; this has led to new explanatory etiologic models, such as multifactorial and biopsychosocial models. Since these etiologic models have tremendous flexibility in determining appropriate etiologic agents, the associated therapeutic methods selected are also highly variable. Greene8 reviewed the etiology of TMDs, proving that a specific agent or even a combination of etiologic agents that can be differentiated from other possible agents does not exist. There is no proof that individual anti-etiologic therapies can actually stop or reduce the etiologic agent they are supposed to affect.
Schwartz9 was one of the first investigators to propose the importance of muscle spasm as a primary etiological factor in initiating pain and dysfunction in the temporomandibular region. He also proposed the importance of the psychological characteristics of the patient. These observations preceded what is now known as the "psychophysiological theory."
Some treatments (e.g., botulinum toxin (Botox®) injections) are carried out at least partly on the basis that there is something wrong with the activity of the lateral pterygoid muscle.1011 Signs of tenderness to palpation of the purported lower border of the muscle are common in TMD patients, and some clinicians consider that the lateral pterygoid muscle is involved in the etiology of clicking, which, when severe, can be painful.12
Our hypothesis is that the hyperactivity of lateral pterygoid muscles can cause asymmetry on the LPP. This can explain the presence of pain and TMD in patients. There are several studies that demonstrate changes in the growth of the mandible or maxillae that can be compatible with hyperplasia or hypoplasia.13 However, no syndrome or disorder of the sphenoid bone itself has been reported that might alter only its pterygoid process.1415 Only unilateral fibrous dysplasia of the sphenoid bone has been reported to cause a full enlargement of the affected side.16
In the present study, the average length of LPP in patients without TMD was 11.86±1.97 mm on the right side and 11.98±1.85 mm on the left side. These results are comparable with those reported by Ueki et al. in 2009. Ueki et al. evaluated 82 Japanese patients with mandibular prognathism and facial asymmetry and found that the average length of LPP in patients without TMD was 11.3±3.2 mm on the right side and 12.6±3.9 mm on the left side.17 This reinforces the difference between the two groups found in our study since patients studied in the latter study had no reported TMD.
When a TMJ dysfunction occurs, there is an internal degeneration, which usually begins with a displacement of the articular disc. This displacement may be caused by trauma or a permanent mild injury that can lead a long spasm in the lateral pterygoid muscle, predominantly to the superior fascicle that inserts mainly on the outer wing of the pterygoid tubercle and on the antero-medial pole of the articular disc.18
The empirical observation that led to this study has been confirmed with the results and may explain why patients with TMD have a chronic spasm of the lateral pterygoid muscle. This excessive muscle tension produces a gradual remodeling on the outer wing of the pterygoid tubercle, which can condition its elongation over an undetermined period of time.
Statistically significant differences were found in almost all patient age groups when we compared patients with and without TMD. Only the group of patients under 20 years of age demonstrated no statistically significant differences (p=0.067) on the right side, which could be attributed to the fact that they have not yet concluded their growth.
No statistically significant differences were found when the gender was compared between groups with and without TMD (P>0.05). This agreed with the results of Peck (2007), who demonstrated that bone remodeling is not dependent on patients' gender but on their muscular activity.19
It is not possible to be sure that the pain reported by the patient corresponds to the lateral pterygoid muscle, as many other muscles can cause pain in the area. Patients who had pain on the right side were compared in terms of the length of the LPP, revealing a statistically significant relation with increased lengths on the same side (p<0.001). The same occurred when patients with TMD and increased length on the left side and pain on the same side were compared (p=0.002). To the best of our knowledge, these results on the LPP length and pain relationship have not been reported in the literature thus far.
Kannan evaluated the efficacy of pterygoid dysfunction for surgical management of the temporomandibular joint (TMJ) pain and dysfunction, and found that after surgery, most patients were free from pain, while in the remaining patients, the intensity of pain was reduced.15 The surgical procedure that was examined resulted in the shortening of the lateral and medial pterygoid muscles. This was expected to result in the decompression of the joint indirectly because of the reduction in the anterior and upward vectors of force on the condyle from the pterygoid muscles. Finally, the authors hypothesized a reduced pressure on the bilaminar zone, which is wedged between the anterior surface of the condyle and the articular eminence (in anterior disk displacement) during movement. This reduction of pressure may alleviate the pain.
Information regarding the LPP lengths can also be useful for clarifying evidence that suggests that etiology is unequivocally linked to symptomatology, since all care provided must be evidence-based and appropriately sequenced. Within the limits of the present study, CBCT LPP measurements on the side with TMD were found to be significantly different from those on the side without TMD.
Figures and Tables
 | Fig. 1Coronal cone-beam computed tomography (CT) image shows the intersection of the midsagittal plane with the nasal cavity floor plane. |
 | Fig. 2Sagittal cone-beam CT image shows the midsagittal plane and the long axis of the palatal plane selected in order to obtain a proper axial view of the outer wings of the bilateral pterygoid tubercle. |
 | Fig. 3Axial cone-beam CT image shows the measurement in the lateral pterygoid plate (LPP), medial pterygoid plate (MPP), and maxillary sinus (MS). |
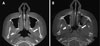 | Fig. 4A. Axial cone-beam CT image shows the differences between the left and the right pterygoid plates of a 22-year-old man with temporomandibular disorder (TMD) B. Axial cone-beam CT image shows no differences between the left and the right pterygoid plates on a matched control. |
References
1. Okeson JP. Current terminology and diagnostic classification schemes. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997; 83:61–64.

2. Murray GM, Bhutada M, Peck CC, Phanachet I, Sae-Lee D, Whittle T. The human lateral pterygoid muscle. Arch Oral Biol. 2007; 52:377–380.

3. Fujita S, Iizuka T, Dauber W. Variation of heads of lateral pterygoid muscle and morphology of articular disc of human temporomandibular joint - anatomical and histological analysis. J Oral Rehabil. 2001; 28:560–571.

4. Liu ZJ, Wang HY, Pu WY. A comparative electromyographic study of the lateral pterygoid muscle and arthrography in patients with temporomandibular joint disturbance syndrome sounds. J Prosthet Dent. 1989; 62:229–233.
5. Grunheid T, Langenbach GE, Korfage JA, Zentner A, van Eijden TM. The adaptive response of jaw muscles to varying functional demands. Eur J Orthod. 2009; 31:596–612.

6. Osborn AG. Radiology of the pterygoid plates and pterygopalatine fossa. AJR Am J Roentgenol. 1979; 132:389–394.

7. List T, Dworkin SF. Comparing TMD diagnoses and clinical findings at Swedish and US TMD centers using research diagnostic criteria for temporomandibular disorders. J Orofac Pain. 1996; 10:240–253.
8. Greene CS. The etiology of temporomandibular disorders: implications for treatment. J Orofac Pain. 2001; 15:93–116.
9. Schwartz LL. Pain associated with the temporomandibular joint. J Am Dent Assoc. 1955; 51:394–397.

10. Schwartz M, Freund B. Treatment of temporomandibular disorders with botulinum toxin. Clin J Pain. 2002; 18:S198–S203.

11. Freund B, Schwartz M, Symington JM. Botulinum toxin: new treatment for temporomandibular disorders. Br J Oral Maxillofac Surg. 2000; 38:466–471.

12. Bakke M, Moller E, Werdelin LM, Dalager T, Kitai N, Kreiborg S. Treatment of severe temporomandibular joint clicking with botulinum toxin in the lateral pterygoid muscle in two cases of anterior disc displacement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005; 100:693–700.

13. Bakathir AA, Margasahayam MV, Al-Ismaily MI. Maxillary hyperplasia and hyperostosis cranialis: a rare manifestation of renal osteodystrophy in a patient with hyperparathyroidism secondary to chronic renal failure. Saudi Med J. 2008; 29:1815–1818.
14. Sharma R. Pterygoid disjunction for internal derangement of temporomandibular joint. J Maxillofac Oral Surg. 2011; 10:142–147.

15. Kannan SV. Pterygoid dysjunction: new minimally invasive technique for the treatment of painful temporomandibular joint dysfunction. J Craniofac Surg. 2010; 21:1264–1269.
17. Ueki K, Hashiba Y, Marukawa K, Nakagawa K, Okabe K, Yamamoto E. Determining the anatomy of the descending palatine artery and pterygoid plates with computed tomography in Class III patients. J Craniomaxillofac Surg. 2009; 37:469–473.

18. Sato S, Kawamura H, Motegi K, Takahashi K. Morphology of the mandibular fossa and the articular eminence in temporomandibular joints with anterior disc displacement. Int J Oral Maxillofac Surg. 1996; 25:236–238.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download