Abstract
Purpose
The purpose of this study was to evaluate and compare the efficacy of cone-beam computed tomography (CBCT) and digital intraoral radiography in diagnosing simulated small external root resorption cavities.
Materials and Methods
Cavities were drilled in 159 roots using a small spherical bur at different root levels and on all surfaces. The teeth were imaged both with intraoral digital radiography using image plates and with CBCT. Two sets of intraoral images were acquired per tooth: orthogonal (PA) which was the conventional periapical radiograph and mesioangulated (SET). Four readers were asked to rate their confidence level in detecting and locating the lesions. Receiver operating characteristic (ROC) analysis was performed to assess the accuracy of each modality in detecting the presence of lesions, the affected surface, and the affected level. Analysis of variation was used to compare the results and kappa analysis was used to evaluate interobserver agreement.
Results
A significant difference in the area under the ROC curves was found among the three modalities (P=0.0002), with CBCT (0.81) having a significantly higher value than PA (0.71) or SET (0.71). PA was slightly more accurate than SET, but the difference was not statistically significant. CBCT was also superior in locating the affected surface and level.
External root resorption (ERR) is defined as the loss of mineralized dental tissue, such as cementum, dentin, and even alveolar bone, as the result of various factors leading to alterations in osteoclastic activity. It occurs physiologically during the normal exfoliation of the primary dentition. When pathology is involved, various factors may play a role, such as inflammation or infection and pressure caused by impacted teeth, masses (tumors or cysts), or orthodontic movement. Fuss et al.1 suggested a simple yet comprehensive classification system that can best describe the etiologies involved: pulpal infections, periodontal infections, orthodontic treatments, impacted tooth or tumors, and ankylosis.
The current technique of choice for diagnosing ERR is conventional or digital intraoral radiography. Most frequently, ERR is discovered accidentally during routine oral examinations and is usually found in its late stages; thus, unfortunately, if the lesion is advanced, the only viable solution is tooth extraction. Therefore, the accurate diagnosis of an incipient ERR lesion is very important, as it may lead to appropriate treatment planning. The interpretation of periapical films may not result in accurate information for many reasons, such as the projection of the lingual and buccal cortices, the projection of multiple roots, and also adjacent anatomical structures that might mimic external root resorption.23 Conventional transmission radiography projects three-dimensional (3D) structures onto a two-dimensional medium; therefore, the topography and extent of ERR cannot be evaluated with certainty.4 Advanced imaging modalities, such as conebeam computed tomography (CBCT), offer a 3D presentation of 3D structures. Some of the advantages of CBCT that make it a desirable tool for detecting such subtle changes are that it provides 3D full volumetric reconstruction by processing two-dimensional cone-beam projections, it offers multidirectional presentation so the viewer can assess the target area in all planes, it involves relative low levels of radiation, and, finally, it can eliminate the need to take multiple angulated projections as well as the retakes that are sometimes necessary.4 Computed tomography is no longer a new technology in diagnosing dental diseases; it has been successfully used in dentomaxillofacial imaging for the diagnosis and treatment planning of malformations, impacted teeth, implants, and many other conditions.
The main purpose of this study was to assess the accuracy of CBCT in detecting incipient ERR lesions and to compare it to the more commonly used technique of intraoral periapical radiography.
Eight dry human mandibles, containing 120 teeth with a total of 159 roots (single and multi-rooted teeth), were acquired from the Forensic Odontology Division of the Comprehensive Dentistry Department, UTHSCSA. Only fully developed and intact roots were accepted; therefore, we excluded four developing third molars and one molar with completely missing roots.
The teeth were extracted by hand. This operation was easily accomplished for the majority of the teeth, since they had been previously used in another study and had been fixed back into their sockets using dental wax. The teeth we considered difficult to extract were left untouched and used as negative controls. Small lesions were simulated by drilling superficial holes with a #1 spherical bur (1 mm Φ and 0.5 mm deep) on the buccal (B), lingual (L), mesial (M), and distal (D) root surfaces and at the superior, middle, and apical levels. Each root received only one lesion. The teeth were then placed back in their sockets and fixed with dental wax. Approximately 10 lesions were drilled per mandible, resulting in a total of 81 lesions (positives), as well as 78 controls. Of these, 35 lesions were placed in an interproximal (mesial or distal) area, and 46 were placed in the buccolingual area.
For the digital intraoral radiography, periapical projections were acquired for each tooth group (molar, premolar, canine, and incisors): one regular (orthoradial or orthogonal), and one mesioangulated view (15°) per group of teeth. Seven orthoradial and seven mesioangulated periapical radiographs were acquired for each mandible, resulting in a total of 112 periapical radiographs. In order to simulate soft tissue, a soft tissue-equivalent plastic device 1 cm in thickness was placed between the tube head and the radiographed teeth (Fig. 1). The intraoral images were acquired on #1 and #2 image plates (ScanX, AirTechniques, Melville, NY, USA) using a Prostyle Intra machine (Planmeca Oy 00880, Helsinki, Finland). The exposure parameters were set at 60-63 kVp, 8 mA, and 0.16-0.4 seconds. The exposure parameters varied because we followed the recommended parameters for each tooth group. The image plates were then scanned with a ScanX scanner (Air Techniques, Melville, NY, USA).
For advanced 3D imaging, one CBCT scan was acquired per mandible, using a Planmeca Promax 3D scanner (Planmeca Oy 00880, Helsinki, Finland). The mandibles were embedded in water to simulate soft tissue. The exposure parameters were set as 84 kVp, 14 mA, and 12 seconds, 401×401×401 pixels matrix, a voxel size of 200 µm, and a slice thickness of 1 mm.
The periapical radiographs were exported as TIFF files to avoid any loss of data through compression and were presented for viewing in a folder containing one orthogonal (PA, Fig. 2) image and a combination of that orthogonal image and its corresponding mesioangulated view (SET, Fig. 3). The CBCT scans (Fig. 4) were exported as 15-bit images using integrated viewer software (Planmeca Romexis Viewer®, Helsinki, Finland).
Four readers, all oral radiology residents, independently evaluated the images in one viewing session. The readers were asked to ignore any other pathology and rate their confidence in detecting the presence of a lesion using a five-point rating scale: 1, lesion definitely absent; 2, lesion probably absent; 3, unsure; 4, lesion probably present; and 5, lesion definitely present. The readers were also asked to locate the surface and the level of the lesions they identified. A training session was held prior to their viewing sessions, and it was explained that the simulated lesions were small hemispherical root defects, not irregular as one might expect in practice.
All statistical analyses were performed using IBM SPSS for Windows version 20.0 (IBM Corp., Armonk, NY, USA). The area under the receiver operating characteristic (ROC) curve was used to assess the diagnostic accuracy of the three modalities (detection on PA, SET, and CBCT). Sensitivity and specificity values were calculated, with a score of 3, 4, or 5 by a reviewer considered positive. The ROC areas, sensitivity, and specificity were analyzed using analysis of variance. For surface and level indications, the percentages of correct evaluations were used. The kappa statistic was used to assess interobserver agreement. Intraobserver agreement was not evaluated due to time restrictions.
Before the study was initiated, a power analysis was conducted. The original plan called for 88 positive roots and 28 negative roots. These numbers would have resulted in a power of 0.80 for detecting a difference in area under the ROC curve of 0.10 (0.80 for conventional vs. 0.90 for CBCT) in a two-tailed test with a significance level of 0.05, using only one reader. The participation of four readers increased the power to 0.85. Since we were unable to extract some teeth, only 81 positive roots were obtained. We increased the number of negative roots to the 78 roots that were available. This increased the power for a single reader to 0.82. In our study, we observed areas under the curve of approximately 0.71 for conventional imaging and 0.81 for CBCT, which was somewhat different than the anticipated results. Even in this situation, the power of the study was still adequate, at approximately 0.74 for a single reader and 0.80 with the participation of four readers.
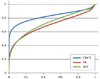
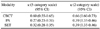
A significant difference was found in the areas under the ROC curves among the three modalities (P=0.0002), with CBCT having significantly higher values than PA or SET, as shown in Figure 5 and Table 1.
A significant difference in sensitivity was found among the three modalities, with CBCT being significantly more sensitive than PA or SET (Table 1). No significant differences in specificity were observed among the imaging modalities.
Table 3 shows the kappa statistics for agreement among the four readers in assessing the presence of a lesion using the original five-category scale and a two-category scale in which scores of 3, 4, and 5 were considered positive.
For each lesion, the percentage of observations in which the reader identified the correct surface was calculated. The percentage of correct observations for L lesions was significantly higher than for D or M lesions (Table 3).
For each lesion, the percentage of observations in which the reader identified the correct level was calculated. Table 4 shows the percentage of correct responses by level. The percentage of correct scores was significantly lower for apical lesions than for middle or superior lesions, and no significant difference was observed between middle and superior lesions.
Our results indicated that CBCT was superior in detecting incipient ERR lesions (Fig. 5, Table 1). This was essentially in accordance with previous studies.35678 Our study did not show a 100% rate of true positives with CBCT because it was a dynamic analysis, involving constant scrolling through the volume of the acquired images, such that a fatigued and/or untrained eye might easily miss small lesions. Moreover, our sample size was much larger than other studies, we used multiple tooth types with varying root shapes and morphologies, and we also included more observers. No special radiographic training session on viewer software manipulation was performed prior to the radiographic evaluations.
We expected that having a different, angulated projection (SET) would lead to better results than were obtained in the orthogonal intraoral radiography (PA) assessment. However, the results proved otherwise (Fig. 5, Table 1), with PA demonstrating slightly better results than SET, although no significant difference was observed. All previous studies that compared intraoral radiography with CBCT have considered all three projections (orthogonal, mesioangulated, and distoangulated) as a single imaging modality, making it difficult to contextualize our results.567
CBCT proved to be significantly more sensitive than the other two modalities (Table 1). However, although it was more sensitive than the other modalities, the sensitivity of CBCT was 69%, meaning that false negatives were observed in 31% of cases where a lesion actually was present.
All three modalities analyzed showed specificity values higher than 79% (Table 1). Although not significantly higher than that of the other modalities, the specificity of CBCT was 91%. Thus, CBCT gave a false positive result in less than 10% of cases where no lesion was present.
Instances of buccolingual ERR were correctly identified slightly more frequently than interproximal instances of ERR (Table 3). We observed that, with the exception of three readings that completely confused B with L, all missed surfaces were interproximal cases of ERR that were diagnosed as either B or L. This could be explained by a technical problem that we did not take into consideration. When the teeth were extracted, the lesions were placed on the chosen anatomical surface (i.e., B). When placed back in their sockets, the teeth rotated slightly along their axes, shifting the lesions mesially or distally. The percentage of lesions correctly identified as L was significantly higher than that of D or M lesions and also higher than that of B lesions, although the difference was not significant. The study conducted by Kumar et al.9 also showed a high percentage of detection for lingual lesions. Table 3 shows the percentage of lesions correctly identified on each surface. For each lesion, we computed the percentage of observations in which the reader identified the correct surface, regardless of the imaging modality that was used. This was mainly because the readers correctly identified the surface and level only after viewing the CBCT images. Even if they could correctly detect the presence of ERR using all three modalities, they were most confident in locating them on CBCT. This observation was confirmed in the agreement analysis (Table 2), in which poor agreement was found between readers when only PA and SET images were analyzed.
Apical lesions were missed most frequently (Table 4), most likely due to variations in apical morphology, their small size, and different orientations.
The most frequent limitations from previous studies were addressed in the present study. The most important limitations of previous studies were small sample sizes and the use of one type of tooth.567 We decided to use all mandibular teeth groups. Some of the previous studies cited by Kumar et al.9 suggested that the maxillary incisors are most frequently affected by root resorption following orthodontic treatment. This generalization, nevertheless, does not rule out the possibility of ERR occurring in any type of root (e.g., the distal root of a mandibular second molar adjacent to an impacted third molar), and the diagnostic and therapeutic choices are correspondingly challenging. We also decided to use all root surfaces and three different root levels. Our purpose was to address all the possibilities that one might encounter in dental practice. We decided not to use any artificial material, and used dried mandibles to better simulate a normal, almost clinical situation, where roots are surrounded by trabecular bone, with a peripheral cortical outline, and imaged and visualized in their anatomical positions.
We opted to only assess lesions of one size, since the previous studies cited by Patel et al.2 showed that intraoral radiography performed poorly in the detection of small lesions. In contrast, all imaging modalities have been shown to be capable of detecting large cavities, such that severe ERR does not present a significant diagnostic challenge.
For the anterior teeth used in previous studies, all three intraoral PA projections are valuable and could be reproduced in common practice. In light of our goal of simulating clinical situations, we decided against using a distoangulated projection, since we used molars, making the clinical applicability of that projection less compelling.
Some of the limitations of our study are the fact that it was in vitro study using dried mandibles, it incorporated artificially created lesions that do not exactly reproduce the clinical features of ERR, it included teeth previously used for a different study on the detection of root fractures, it did not include any clinical information and patient dental history that could help contextualize the observations, and the use of a single interpretation session may have led to fatigue among the readers.
The use of CBCT results in slightly higher values of radiation exposure than digital intraoral radiography, but the radiation exposure is much lower than that of medical computed tomography. Nonetheless, proper preparations should be considered when prescribing advanced imaging modalities. Accurate selection criteria should be employed, and adjustment of the exposure parameters and the field of view should be a constant concern during 3D imaging, as well as always weighing the benefits and possible risks to the patient.101112
Keeping in mind that "all radiographic examinations must be justified on an individual needs basis whereby the benefits to the patient... must outweigh the risks," if CBCT is used wisely (not on a routine basis and not without a previous through clinical examination), it could become an excellent alternative to conventional intraoral radiography, as it has been shown to be a powerful and accurate diagnostic tool.10
In conclusion, the superimposition of anatomic structures as well as root thickness may obscure many anatomical and pathological details in traditional radiographs. In our study, it was shown that CBCT was capable of eliminating the effect of those factors, resulting in images with the high level of detail needed to detect external root resorption, even in its early stages.
Figures and Tables
Fig. 3
A set of orthogonal (PA, left) and corresponding mesioangulated projection (SET, right) are taken.
Fig. 4
Planmeca Romexis Viewer Software shows axial, coronal, sagittal, and three-dimensional CBCT images of simulated external root resorption (arrows).
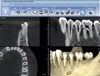
Fig. 5
Receiver operating characteristic (ROC) curves for all modalities of PA, SET, and CBCT images.
References
1. Fuss Z, Tsesis I, Lin S. Root resorption - diagnosis, classification and treatment choices based on stimulation factors. Dent Traumatol. 2003; 19:175–182.

2. Patel S, Dawood A, Wilson R, Horner K, Mannocci F. The detection and management of root resorption lesions using intraoral radiography and cone beam computed tomography - an in vivo investigation. Int Endod J. 2009; 42:831–838.
3. Patel S, Dawood A, Ford TP, Whaites E. The potential applications of cone beam computed tomography in the management of endodontic problems. Int Endod J. 2007; 40:818–830.

4. Noujeim M, Prihoda T, Langlais R, Nummikoski P. Evaluation of high-resolution cone beam computed tomography in the detection of simulated interradicular bone lesions. Dentomaxillofac Radiol. 2009; 38:156–162.

5. Durack C, Patel S, Davies J, Wilson R, Mannocci F. Diagnostic accuracy of small volume cone beam computed tomography and intraoral periapical radiography for the detection of simulated external inflammatory root resorption. Int Endod J. 2011; 44:136–147.

6. Bernardes RA, de Paulo RS, Pereira LO, Duarte MA, Ordinola-Zapata R, de Azevedo JR. Comparative study of cone beam computed tomography and intraoral periapical radiographs in diagnosis of lingual-simulated external root resorptions. Dent Traumatol. 2012; 28:268–272.

7. Kamburoğlu K, Kurşun S, Yüksel S, Oztaş B. Observer ability to detect ex vivo simulated internal or external cervical root resorption. J Endod. 2011; 37:168–175.

8. D'Addazio PS, Campos CN, Özcan M, Teixeira HG, Passoni RM, Carvalho AC. A comparative study between cone-beam computed tomography and periapical radiographs in the diagnosis of simulated endodontic complications. Int Endod J. 2011; 44:218–224.
9. Kumar V, Gossett L, Blattner A, Iwasaki LR, Williams K, Nickel JC. Comparison between cone-beam computed tomography and intraoral digital radiography for assessment of tooth root lesions. Am J Orthod Dentofacial Orthop. 2011; 139:e533–e541.

10. American Association of Endodontists. American Academy of Oral and Maxillofacial Radiography. AAE and AAOMR joint position statement. Use of cone-beam-computed tomography in endodontics. Pa Dent J (Harrisb). 2011; 78:37–39.
11. Ludlow JB, Davies-Ludlow LE, White SC. Patient risk related to common dental radiographic examinations: the impact of 2007 International Commission on Radiological Protection recommendations regarding dose calculation. J Am Dent Assoc. 2008; 139:1237–1243.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download