Abstract
Central odontogenic fibroma (COF) is a rare benign tumor that accounts for 0.1% of all odontogenic tumors. A case of COF (simple type) of the mandible in a four-year-old boy is described in this report. The patient showed asymptomatic swelling in the right inferior border of the lower jaw for one week. A panoramic radiograph showed a poorly-defined destructive unilocular radiolucent area. Cone-beam computed tomography showed expansion and perforation of the adjacent cortical bone plates. A periosteal reaction with the Codman triangle pattern was clearly visible in the buccal cortex. Since the tumor had destroyed a considerable amount of bone, surgical resection was performed. No recurrence was noted.
Central odontogenic fibroma (COF) is an extremely rare benign ectomesenchymal neoplasm that accounts for 0.1% of all odontogenic tumors.1234 It has two major types: (1) the simple type and (2) the World Health Organization (WHO) type.356
This tumor appears in both the mandible and maxilla (55 % and 45%, respectively). It has been reported to occur in a wide age group with a strong female predilection.678
Radiographically, COF is usually radiolucent and sometimes can have a mixed radiolucent-radiopaque appearance. Most COFs are well-defined unilocular lesions, but they can be multilocular or have poorly-defined borders in rare cases.1239
Periosteal reaction occurs when cortical bone reacts to one of a range of possible stimulants.10 A Codman triangle develops when a portion of the periosteum is lifted off of the cortex by a tumor, pus, or hemorrhage at a leading edge. This aggressive form of periosteal reaction is commonly seen in osteosarcomas and occasionally in infection and metastases.11 The current literature contains no report of periosteal reaction accompanying COF.
The aim of this report is to present a case of COF in the mandibular right molar region of a four-year-old boy that had a very rare unusual radiographic and cone-beam computed tomography (CBCT) appearance with periosteal reaction.
A four-year-old boy was referred to the Oral and Maxillofacial Radiology Department at the School of Dentistry of the University of Mashhad. His chief complaint was a swelling in the right inferior border of the lower jaw, which had been present for one week and exhibited slow growth. He reported no pain or other symptoms. His parents had incidentally noticed the swelling. He had visited a general dentist, the lesion was initially diagnosed as a dentoalveolar abscess, and the patient was referred to the Oral and Maxillofacial Radiology Department for further investigation. His medical and familial history was unremarkable.
On the extraoral and intraoral examinations, no trismus, lymphadenopathy, paresthesia, or mucosal changes were observed. No dental caries were present in the right mandibular quadrant. The expansion involved an area measuring approximately 3 cm×2 cm in the right inferior border of the lower jaw anterior to the mandibular angle. It had a non-ulcerated smooth surface. On palpation, the swelling was firm in consistency and non-tender.
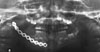
A panoramic radiograph showed a poorly-defined destructive expansive radiolucent area in the posterior body of the mandible near the angle region. The internal pattern was unilocular. The lesion had perforated the inferior cortical border of the mandible. Thinning of the cortical outlines of the follicles of the first and second permanent molars was observed (Fig. 1).
CBCT was performed for further evaluation. On the axial view, lingual expansion and perforation of buccal and lingual cortical plates with some faint septae were seen. A periosteal reaction (Codman triangle) was clearly visible in the buccal cortex (Fig. 2).
The panoramic and cross-sectional reformatted CBCT images also confirmed the previous findings. They showed a poorly-defined multilocular radiolucent lesion with some wispy septae. Periosteal new bone formation was seen in the buccal aspect of the lesion. The buccal, lingual, and inferior cortical plates of the mandible were perforated. No tooth displacement was observed, but the cortical outlines of the follicles of the first and second permanent molars were eroded and perforated. The cortical border of the inferior alveolar nerve canal could not be seen throughout the lesion and seemed to be destructed (Fig. 3).
An incisional biopsy was performed through an extraoral approach. Since the patient was uncooperative, the biopsy was performed under general anesthesia. Gross examination of the biopsy specimen showed several soft tissue pieces that jointly measured approximately 25 mm×15 mm×8 mm, whitish in color and elastic in consistency.
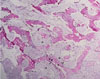
Histopathological examination of the incisional biopsy specimen of the lesion revealed a non-encapsulated tumor consisting of a benign neoplastic proliferation of odontogenic ectomesenchymal tissue. The biopsy showed fibrous connective tissue stroma with plump fibroblastic cells alongside collagen bundles. No odontogenic epithelial cells were found in the sections. Some myxoid changes in the stroma and normal bone trabecules containing osteocyte lacunae and osteoblastic margins were seen (Figs. 4 and 5). A diagnosis of COF (simple type) was established.
Since the tumor had destroyed a considerable amount of bone, surgical resection and bone grafting were performed (Fig. 6). The surgical procedure consisted of segmental resection of the mandible with immediate bone grafting reconstruction via the intraoral route. The autogenous bone was harvested from the iliac crest. The histopathology of the postoperative tissue was consistent with the incisional biopsy diagnosis. Following the resection, the patient was maintained on systemic antibiotics but this failed to prevent infection. The graft site was infected after one month and the infected bone graft was removed (Fig. 7). Graft failure was most likely due to wound dehiscence and bone exposure. A six-month follow-up panoramic radiograph showed that the patient's condition was stable, with no recurrence (Fig. 8).
COF is classified as a rare benign tumor that originates from ectomesenchymal tissues such as the dental papillae, periodontal ligament, or dental follicle.31213 It is most often found in females, and the ratio of incidence in the maxilla and mandible is approximately 1 : 1, with a slight tendency to favor the mandible. It involves the anterior part of the maxilla, whereas mandibular lesions affect the premolar and molar areas.614151617
COF can be subclassified according to histological features. The simple type (the epithelium-poor type) is composed of collagen bundles interspersed with plump fibroblasts. Small nests or islands of inactive odontogenic epithelium may or may not be present. Foci of dystrophic calcification may be seen. Some believe that this lesion belongs to the spectrum of odontogenic myxoma and should be classified as a myxofibroma. The WHO type (the epithelium-rich type) has a more complex pattern and contains long strands or isolated nests of odontogenic epithelial rests. It may have dysplastic dentin, osteoid, or cementum-like calcifications.3561415161819 Our case resembled the simple type.
COF is usually asymptomatic, involving slow expansion of the cortical bones.6142021 Our case occurred in the mandible of a four-year-old boy and manifested as an asymptomatic firm swelling.
Radiographically, COF is mostly unilocular with well-defined borders. Larger lesions show multilocular radiolucency, with radiopaque areas sometimes seen in the interior of the tumor. In rare cases, COF can be poorly defined. Aggressive types can cause root resorption or displace teeth.123914 On CT and CBCT scans, COF usually presents as an expansile homogenous mass that can erode and perforate the adjacent cortical boundaries. Thin and straight septae can also be noted in some lesions.922232425 Less common CT findings include calcified materials within the lesion, a diffuse sclerotic border, and peripheral osteosclerosis.2627 The present case demonstrated a very unique malignancy-like radiographic appearance of COF with periosteal reaction.
Periosteal reaction occurs when cortical bone reacts to one of several possible underlying insults.10 In the jaws, periosteal reaction can occur in patients with inflammatory lesions, osteomyelitis, and malignant tumors, but periosteal reactions rarely occur in cases of benign lesions, such as eosinophilic granuloma and osteoid osteoma. Periosteal reaction is more common in younger people and in patients with sarcomas compared to carcinomas. Usually, a single-layer or multi-layered (lamellated or onion-skin) pattern appears in osteomyelitis and benign lesions, whereas an spiculated, sunray, or Codman triangle appearance is mostly seen in malignant tumors.2829
The imaging presentation of periosteal reaction is characterized by the intensity, aggressiveness, and duration of the underlying etiologic factor. With slow-growing lesions, the periosteum has enough time to respond to the pathological process, resulting in a solid, continuous periosteal reaction. In rapidly growing bone lesions, the periosteum is unable to produce new bone as fast as the growing pathology. Consequently, a discontinuous pattern of periosteal reaction is seen.11
If the periosteum is significantly elevated, it can break, forming an acute angle (Codman triangle). This is usually seen in malignant bone tumors such as osteosarcoma, Ewing's sarcoma, fibrosarcoma, juxtacortical chondrosarcoma, malignant fibrous histiocytoma, metastatic tumors, and in some other rapidly growing lesions such as aneurysmal bone cyst, giant cell tumor, or in reactive processes (osteomyelitis and subperiosteal hematoma).1011303132 To the best of our knowledge, periosteal reaction accompanying COF has not been previously reported. In the present case, the young age of the patient and rapid tumor growth led to a periosteal reaction. It seems that periosteal reaction is more closely related to the age of the patient and duration of the lesion than to the etiology of the tumor.
The radiographic differential diagnosis includes malignant tumors, such as osteosarcoma and Ewing's sarcoma. Osteosarcoma can exhibit a Codman triangle appearance and can be radiolucent with some initial ossification changes, resembling the septae seen in our case. Ewing's sarcoma occurs in young patients and can induce a periosteal reaction. Aggressive benign lesions, such as aneurysmal bone cyst and central giant cell granuloma, can also be included in the differential diagnosis list. In the jaws, aneurysmal bone cyst can cause expansion, and it frequently occurs in the same region as our patient's lesion. Furthermore, both aneurysmal bone cyst and central giant cell granuloma can have a multilocular appearance with some wispy septae.30
The treatment of COF is enucleation and efficient curettage. Recurrence is not common.614 Since the tumor in our case showed aggressive behavior, resection of the lesion and installation of a bone graft were performed.
In conclusion, the purpose of presenting this case was to describe an extremely rare manifestation of central odontogenic fibroma (simple type) in a four-year-old boy. Periosteal reaction with a Codman triangle pattern is very rare in benign tumors, and the present case is the first case of COF reported to occur with a periosteal reaction. It can be concluded that aggressive benign lesions are capable of inducing periosteal reaction in children.
Figures and Tables
Fig. 1
A panoramic radiograph shows a poorly-defined radiolucent lesion in the posterior mandibular region, perforating the inferior mandibular cortex.

Fig. 2
Axial cone-beam computed tomography images show lingual expansion and perforation of the buccal and lingual cortical plates. Note the periosteal reaction (Codman triangle) in the buccal cortex (arrows).

Fig. 3
Panoramic (A) and cross-sectional (B) reformatted cone-beam computed tomography images show a multilocular lesion with some faint septae. The lesion has perforated the lingual, buccal, and inferior mandibular cortical plates, the cortical outlines of the follicles of the molars, and the inferior alveolar nerve canal. Periosteal new bone formation is seen in the buccal cortical plate (arrows).

Fig. 4
Plump fibroblasts (arrow) within a collagenous background. No epithelial remnants are found (H&E stain, 100×)
References
1. Daniels JS. Central odontogenic fibroma of mandible: a case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004; 98:295–300.

2. Kaffe I, Buchner A. Radiologic features of central odontogenic fibroma. Oral Surg Oral Med Oral Pathol. 1994; 78:811–818.

3. Covani U, Crespi R, Perrini N, Barone A. Central odontogenic fibroma: a case report. Med Oral Patol Oral Cir Bucal. 2005; 10:Suppl 2. E154–E157.
4. Cicconetti A, Bartoli A, Tallarico M, Maggiani F, Santaniello S. Central odontogenic fibroma interesting the maxillary sinus. A case report and literature survey. Minerva Stomatol. 2006; 55:229–239.
5. Barnes L, Eveson JW, Reichart P, Sidransky D. World Health Organization classification of tumours. Pathology and genetics: head and neck tumours. Lyon: IARC Press;2005.
6. Waldron CA. Odontogenic cysts and tumots. In : Neville BW, Damm DD, Allen CM, Bouquot J, editors. Oral and maxillofacial pathology. 3rd ed. St. Louis: Saunders Elsevier;2009. p. 726–727.
7. Daskala I, Kalyvas D, Kolokoudias M, Vlachodimitropoulos D, Alexandridis C. Central odontogenic fibroma of the mandible: a case report. J Oral Sci. 2009; 51:457–461.

8. Balaji P, Gupta A, Govindraju P, Vasan V, Jambunath U. Central odontogenic fibroma of maxilla: a rare case. Int J Sci Stud. 2015; 2:189–192.
9. Salgado H, Mesquita P. Central odontogenic fibroma of the maxilla - a case report. Rev Port Estomatol Med Dent Cir Maxilofac. 2014; 55:49–54.

10. Wenaden AE, Szyszko TA, Saifuddin A. Imaging of periosteal reactions associated with focal lesions of bone. Clin Radiol. 2005; 60:439–456.

12. Bodner L. Central odontogenic fibroma. A case report. Int J Oral Maxillofac Surg. 1993; 22:166–167.

13. Venugopal S, Radhakrishna S, Raj A, Sawhney A. Central odontogenic fibroma. J Indian Soc Periodontol. 2014; 18:240–243.

14. Thankappan P, Chundru NS, Amudala R, Yanadi P, Rahamthullah SA, Botu M. Central odontogenic fibroma of simple type. Case Rep Dent. 2014; 2014:642905.

15. Gaikwad PT, Kulkarni MM, Saluja H, Nikam A, Yemle S, Sabnis SL. Central odontogenic fibroma: a case report and review of literature. Int J Oral Maxillofac Pathol. 2013; 4:29–32.
16. Veeravarmal V, Madhavan RN, Nassar MM, Amsaveni R. Central odontogenic fibroma of the maxilla. J Oral Maxillofac Pathol. 2013; 17:319.

17. Ramer M, Buonocore P, Krost B. Central odontogenic fibroma-report of a case and review of the literature. Periodontal Clin Investig. 2002; 24:27–30.
19. Brazao-Silva MT, Fernandes AV, Durighetto-Junior AF, Cardoso SV, Loyola AM. Central odontogenic fibroma: a case report with long-term follow-up. Head Face Med. 2010; 6:20.

20. Schussel JL, Gallottini MH, Braz-Silva PH. Odontogenic fibroma WHO-type simulating periodontal disease: report of a case. J Indian Soc Periodontol. 2014; 18:85–87.

21. de Matos FR, de Moraes M, Neto AC, Miguel MC, da Silveira EJ. Central odontogenic fibroma. Ann Diagn Pathol. 2011; 15:481–484.

22. Talukder S, Agarwal R, Gupta P, Santosh BS, Misra D. Central odontogenic fibroma (WHO Type): a case report and review of literature. J Indian Acad Oral Med Radiol. 2011; 23:259–262.

24. Hwang EH, Lee SR. Central odontogenic fibroma of the simple type. Korean J Oral Maxillofac Radiol. 2002; 32:227–230.
25. Eversole LR. Odontogenic fibroma, including amyloid and ossifying variants. Head Neck Pathol. 2011; 5:335–343.

26. Ikeshima A, Utsunomiya T. Case report of intra-osseous fibroma: a study on odontogenic and desmoplastic fibromas with a review of the literature. J Oral Sci. 2005; 47:149–157.

27. Araki M, Nishimura S, Matsumoto N, Ohnishi M, Ohki H, Komiyama K. Central odontogenic fibroma with osteoid formation showing atypical radiographic appearance. Dentomaxillofac Radiol. 2009; 38:426–430.

28. Ida M, Tetsumura A, Kurabayashi T, Sasaki T. Periosteal new bone formation in the jaws. A computed tomographic study. Dentomaxillofac Radiol. 1997; 26:169–176.

29. An SY, Shin HI, Choi KS, Park JW, Kim YG, Benavides E, et al. Unusual osteoid osteoma of the mandible: report of case and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013; 116:e134–e140.

30. White SC, Pharoah MJ. Oral radiology: principles and interpretation. 7th ed. St. Louis: Elsevier;2014.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download