Abstract
Bony fusion between the mandibular condyle and skull base involves temporomandibular joint (TMJ) bony ankylosis. This condition might originate from trauma, infection, or systemic disease. TMJ adhesion can develop after synovial damage. Both TMJ ankylosis and adhesion lead to functional impairment and pain. Here, we present a case of a 50-year-old female who had bony ankylosis of the right TMJ and adhesion of the left TMJ. She had otitis media in the right ear. A large mass in the right TMJ was observed on computed tomograph. Magnetic resonance image showed a large fused bone mass with normal bone marrow in the right TMJ and flattening of the condyle with a thin disk in the left TMJ. Gap arthroplasty with temporal fascia was performed on the right TMJ, and discectomy, high condylectomy, and coronoidectomy were performed on the left TMJ. During a 2-year follow-up after surgery, the patient had no recurrence.
Bony ankylosis of the temporomandibular joint (TMJ) is a fusion between the condyle and the temporal bone, which partially or completely obliterates the articular space and causes joint deformity. The fused bony fragment or a large bone mass may involve the condyle of the mandible, the temporal bone, and the zygomatic process. Thus, bony ankylosis can be easily diagnosed with conventional radiological tools such as panoramic view and computed tomography (CT).1234 In 2002, El-Hakim and Metwalli4 reported a new classification of bony ankylosis including surrounding vital structures (Table 1). This classification provides more information to surgeons during the pre-surgical period and during surgery.4 The common causes of ankylosis are trauma (31%-98%), infection (10%-49%), and systemic diseases. TMJ ankylosis negatively affects the patient's quality of life. Because the mouth opening is impaired, mastication and speech are difficult. Generalized caries, poor oral hygiene, facial asymmetry, and obstructive sleep apnea may also occur.567 The pathogenesis of TMJ adhesion is not yet fully understood.8910 Kaminishi and Davis8 suggested two mechanisms for TMJ adhesion. In the first mechanism, synovitis induces a fibrin layer on the articular surface; this layer becomes the fibrous tissue. In the second mechanism, joint space hematomas become scar-like fibrous tissue during healing. This may eventually develop into fibrous adhesion. Since TMJ adhesion limits anterior and posterior TMJ movements, the mouth opening becomes impaired and is frequently associated with pain.91011 To the best of our knowledge, only a few cases of TMJ ankylosis on one side and TMJ adhesion on the other side have been reported. In this paper, we report a rare case of TMJ ankylosis on one side and severe TMJ adhesion on the opposite side and discuss the radiological diagnosis and treatment of the same.
A 50-year-old female was referred to the Department of Oral and Maxillofacial Surgery for treatment of TMJ ankylosis. Ankylosis began when the patient was 12 years old. The patient had experienced a fall, but she could not remember the time and the specifics of the associated trauma accurately. She had experienced otitis media in her right ear more than 20 years previously. Clinical examination revealed facial asymmetry and limitation of the mouth opening (2 mm). On a panoramic radiograph, bony fusion of the right TMJ, a prominent right antegonial notch, and severe deviation of the mandible to the right were noted, along with multiple dental caries, retained roots, and generalized severe alveolar bone loss. A well-defined outline of the condyle was noted in the left TMJ (Fig. 1). CT images revealed bony ankylosis with a large mass in the right TMJ area, the loss of air cells in the temporal squama and mastoid area, and a thickened right zygomatic arch. The normal relationship of the articular fossa and the condyle with the articular space was revealed in the left TMJ (Fig. 2). Magnetic resonance imaging (MRI) showed a large fused bone mass with normal bone marrow in the right TMJ (Fig. 3) and flattening of the condyle with a thin disk in the left TMJ. Irregularities of the cortical bone of the articular fossa and the condyle were also detected in the left TMJ (Fig. 4).
A three-dimensional (3D) rapid prototyping (RP) model was fabricated using the CT images. The right condyle was fused with the posterior portion of the zygomatic arch. Abnormal bone formation was detected in and around the TMJ. Anatomical structures of the TMJ were not found (Fig. 5A). A narrowed articular space between the condylar head and the articular fossa was detected in the left TMJ (Fig. 5B).
Radiographically, the differential diagnoses for the right TMJ included benign bone tumors such as osteochondroma, ostoma, chondroma, chondroblastoma, benign osteoblastoma, fibro-osteoma, fibrous dysplasia, myxoma, and giant cell tumor. However, careful history taking and radiological and histological examination for this patient would be useful for the differential diagnosis.12 On the basis of the clinical and radiological examinations, the patient was diagnosed with bony ankylosis in the right TMJ and suspected adhesion in the left TMJ.
Surgery was performed under general anesthesia using laryngoscopy with nasotracheal intubation. A preauricular incision with a temporal extension on the right side was made. In order to create an approximately 15 mm wide gap, excision of the bony mass was carried out. Then, the mandible was mobilized manually, but it did not move. An intraoral incision was made on the left side, and the left coronoid process was removed. Another preauricular incision without a temporal extension was made on the left side. Surgical opening of the joint, discectomy, and high condylectomy were performed on the left TMJ. The right temporalis fascia was used as the interpositional graft material. An occlusal stop (height: 30 mm) was inserted between the dental arches and maxillomandibular fixation (MMF) and was maintained for 5 days. The maximum mouth opening (MMO) was 35 mm after surgery. Postoperative pain medications were administered, and vigorous postoperative physiotherapy was performed to preserve the range of motion and to prevent postoperative hypomobility due to recurrence.513
After the 3-month follow-up, the MMO was 25 mm. All teeth were extracted because of the severe dental problems. One month after extraction, the patient underwent dental implant surgery (Fig. 6). Four months after dental implant surgery, she had full mouth rehabilitation (Fig. 7). Two years after surgery, the MMO was approximately 20 mm, and the masticatory function was normal (Fig. 8).
In the past, conventional radiographies such as panoramic, lateral and posteroanterior skull, submentovertex, and transcranial radiography were frequently used for the diagnosis of TMJ pathologies. These radiographies had a limitation with respect to the analysis of anatomical structures because of the superimposition of these structures.3 Nowadays, CT imaging provides more detailed information to radiologists and surgeons, such as the shape of the mandibular condyle and pathological changes in the joint outline. The osseous changes in the condyle such as erosion, osteophyte, and sclerosis are easily detected on the coronal and sagittal views of CT images. Moreover, 3D CT and RP models are useful to radiologists and surgeons in the pre-operative period. They show an accurate, realistic structure of the patient's joint, which is very useful for diagnosis and surgical planning.314 MRI has good tissue contrast resolution and performs better in the differentiation of soft tissue structures than CT images. Adhesion of the TMJ is easily detected by MRI and arthroscopy. Fibrous adhesion is the most common form of an anteriorly displaced disc.9
In our case, radiological findings revealed that the right TMJ definitely had bony ankylosis with a loss of air cells in the temporal squama and mastoid area. Moreover, the zygomatic arch was also thickened abnormally. MRI showed flattening of the condyle and a thin disk in the left TMJ in this case. Adhesion of the TMJ is usually diagnosed on the basis of an immobile disk during mouth opening as revealed by MRI.8915 Because our patient had severe bony ankylosis of the right TMJ, the left TMJ also did not move. Therefore, the diagnosis of the left TMJ was difficult. During surgery, the mandible did not move after right gap arthroplasty; therefore, the left TMJ could be diagnosed with severe adhesion. Further, a patient with unilateral severe bony ankylosis of the TMJ might have adhesion at the opposite side, which would limit mouth opening. Therefore, surgeons should use a more careful approach during surgery.
Roychoudhury et al.16 recommended at least a 15 mm gap between the recontoured glenoid fossa and the mandible for preventing reankylosis. In our case, we obtained a 15 mm gap; this gap was well maintained after surgery. In order to prevent reankylosis, it is important to place an interpositional graft in the surgically formed gap.17 To achieve MMO, ipsilateral and/or contralateral coronoidectomy is necessary.18 In our case, the temporal fascia was used for preventing recurrence, and coronoidectomy of the left mandible was also performed. Because the TMJ area is a complex region, the risk of complications after TMJ surgery is high; complications include facial scars, facial nerve palsy, gustatory sweating, perforation of the middle cranial fossa, and damage of the maxillary artery. 1619 Our patient had pain and a facial scar immediately after surgery, but no other complications. The vertical dimension was newly established during the full-mouth rehabilitation period. Two years after surgery, although the MMO decreased from 35 mm to 20 mm, ankylosis did not recur, the patient was satisfied with surgery, and her body weight increased due to proper nutrition.
In conclusion, a patient with severe bony ankylosis of the TMJ on one side might have adhesion on the opposite side, which would limit mouth opening. This adhesion could not be detected in a radiological examination. Therefore, radiologists and surgeons should use a more careful approach for diagnosis and treatment.
Figures and Tables
Fig. 1
Panoramic radiograph shows bony ankylosis of the right temporomandibular joint (TMJ) and normal outline of the left TMJ.

Fig. 2
Axial (A) and coronal (B) computed tomographic (CT) images show bony ankylosis of the right TMJ and articular space of the left TMJ clearly revealed by CT.

Fig. 3
T1-weighted sagittal (A) and coronal (B) magnetic resonance (MR) images reveal a large fused bone mass in the right TMJ.
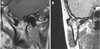
Fig. 4
T1-weighted sagittal (A) and coronal (B) MR images show the flattening of the condyle with a thin disk in the left TMJ.

Fig. 5
Photographs of three-dimensional rapid prototyping model. A. The right condyle is fused with the posterior portion of the zygomatic arch. Abnormal bone formation is also detected in and around the TMJ. B. Narrowed articular space is detected in the left TMJ.

Fig. 6
Panoramic radiograph shows that the patient underwent dental implant surgery 3 months after the surgery.

Table 1
New classification of bony ankylosis of temporomandibular joint (TMJ) by El-Hakim and Metwalli4

References
1. McFadden LR, Rishiraj B. Treatment of temporomandibular joint ankylosis: a case report. J Can Dent Assoc. 2001; 67:659–663.
2. Li JM, An JG, Wang X, Yan YB, Xiao E, He Y, et al. Imaging and histologic features of traumatic temporomandibular joint ankylosis. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014; 118:330–337.

3. Casanova MS, Tuji FM, Ortega AI, Yoo HJ, Haiter-Neto F. Computed tomography of the TMJ in diagnosis of ankylosis: two case reports. Med Oral Patol Oral Cir Bucal. 2006; 11:E413–E416.
4. El-Hakim IE, Metwalli SA. Imaging of temporomandibular joint ankylosis. A new radiographic classification. Dentomaxillofac Radiol. 2002; 31:19–23.

5. Manganello-Souza LC, Mariani PB. Temporomandibular joint ankylosis: report of 14 cases. Int J Oral Maxillofac Surg. 2003; 32:24–29.

6. Chidzonga MM. Temporomandibular joint ankylosis: review of thirty-two cases. Br J Oral Maxillofac Surg. 1999; 37:123–126.

7. Bhatt K, Roychoudhury A, Balakrishnan P. Temporomandibular joint ankylosis: is hypercoagulable state of blood a predisposing factor? Med Hypotheses. 2013; 81:561–563.

8. Kaminishi RM, Davis CL. Temporomandibular joint arthroscopic observations of superior space adhesions. Oral Maxillofac Surg Clin North Am. 1989; 1:103–109.
9. Sanromán JF. Closed lock (MRI fixed disc): a comparison of arthrocentesis and arthroscopy. Int J Oral Maxillofac Surg. 2004; 33:344–348.

10. Shinohara Y, Okamoto K, Goh Y, Kiga N, Tojyo I, Fujita S. Inhibition of fibrous adhesion formation in the temporomandibular joint of tenascin-C knockout mice. Eur J Histochem. 2014; 58:2337.

11. Sheets DW Jr, Okamoto T, Dijkgraaf LC, Milam SB, Schmitz JP, Zardeneta G. Free radical damage in facsimile synovium: correlation with adhesion formation in osteoarthritic TMJs. J Prosthodont. 2006; 15:9–19.

12. More CB, Gupta S. Osteochondroma of mandibular condyle: a clinic-radiographic correlation. J Nat Sci Biol Med. 2013; 4:465–468.

13. Sporniak-Tutak K, Janiszewska-Olszowska J, Kowalczyk R. Management of temporomandibular ankylosis - compromise or individualization - a literature review. Med Sci Monit. 2011; 17:RA111–RA116.

14. Sales MA, Oliveira JX, Cavalcanti MG. Computed tomography imaging findings of simultaneous bifid mandibular condyle and temporomandibular joint ankylosis: case report. Braz Dent J. 2007; 18:74–77.

15. Zhang S, Liu X, Yang C, Cai X, Chen M, Haddad MS, et al. Intra-articular adhesions of the temporomandibular joint: relation between arthroscopic findings and clinical symptoms. BMC Musculoskelet Disord. 2009; 10:70.

16. Roychoudhury A, Parkash H, Trikha A. Functional restoration by gap arthroplasty in temporomandibular joint ankylosis: a report of 50 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999; 87:166–169.
17. Vasconcelos BC, Bessa-Nogueira RV, Cypriano RV. Treatment of temporomandibular joint ankylosis by gap arthroplasty. Med Oral Patol Oral Cir Bucal. 2006; 11:E66–E69.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download