Abstract
Glandular odontogenic cysts (GOCs) are rare intrabony solitary or multiloculated cysts of odontogenic origin. The importance of GOCs lies in the fact that they exhibit a propensity for recurrence similar to keratocystic odontogenic tumors and that they may be confused microscopically with central mucoepidermoid carcinoma. Thus, the oral and maxillofacial radiologists play an important role in definitive diagnosis of GOC based on distinctive cases; though they are rare. In large part, this is due to the GOC's complex and frequently non-specific histopathology. This report describes a case of GOC occurrence in the posterior mandibular ramus region in a 17-year-old female, which is a rare combination of site, age, and gender for occurrence.
Glandular odontogenic cysts (GOCs) are rare intrabony solitary or multiloculated cysts of odontogenic origin. In 1987, Padayachee and Van Wyk1 first reported two cases that shared the features of both botryoid odontogenic cysts and central mucoepidermoid tumors and suggested that the term "sialo-odontogenic cyst" be adopted for such lesions to avoid confusion and mismanagement. One year later, Gardner et al2 reported eight other cases and favored the name "glandular odontogenic cyst"; they regarded it as a distinct entity due to its unusual histopathological features. In addition, this term was included in the revised edition of a World Health Organization report3 in 1992 as "developmental odontogenic epithelial cyst." It has also been termed "mucoepidermoid cyst" by Sadeghi et al4 and "polymorphous odontogenic cyst" by High et al.5 In the 20 years since it was first described, 111 cases of this type of cyst have been reported, an incidence of 0.2% among odontogenic cysts.6
Hence, although rare, this cyst is a well-known clinical entity and is important to recognize and diagnose due to its aggressive behavior and tendency to recur. This cyst reports a slight male predilection with a male : female ratio of 1.3 : 1,6 and the most-commonly affected site is the anterior mandible. It tends to occur over a wide age range of 10-90 years, with a mean age of 49.5 years. The mandible seems to be affected more commonly (87.2%) than the maxilla.7
Radiographic examination reveals a well-defined cystlike unilocular or multilocular radiolucency, often with scalloped margins and sclerotic borders.8 In addition, there may be root resorption and tooth displacement with cortical perforation, leading to extension of the cyst into the adjacent soft tissues.
Histologically, GOC is characterized by a cyst wall lining of non-keratinized epithelium with papillary projections, nodular thickenings, mucous-filled clefts, and "mucous lakes." In addition, it includes cuboidal basal cells, which are sometimes vacuolated.9,10
GOC treatment includes curettage and enucleation, although some authors believe marginal resection to be a more reliable treatment due to the tendency of the cyst to recur after curettage and enucleation.10
The aim of this report is to present a case of GOC in a young female patient in the posterior mandibular region, which was quite rare and unusual.
A 17-year-old female patient was referred to the Outpatient Department of Oral Medicine and Radiology at Nair Hospital Dental College, Mumbai, by a local orthodontist after discovering a well-defined radiolucent pathology in the right ramal region of the mandible on a routine panoramic view.
The patient reported mild dull pain over the right posterior mandibular region for a period of 15 days with no aggravating or relieving factors. An extraoral examination revealed no significant clinical findings. Intraorally, there was mild obliteration of the buccal vestibule in the right lower second molar region with no other relevant clinical finding. The patient's medical history revealed that she had suffered from allergic asthma since childhood, she was not on any medication for the condition.
A panoramic radiograph was obtained using a Planmeca Proline CC machine (Planmeca OY, Helsinki, Finland) with exposure parameters of 73 kVp, 10 mA, and 15 s exposure time. A well-defined multiloculated radiolucent lesion was observed extending from the distal border and apex of the lower right second molar into the ramus to approximately 3 mm away from the sigmoid notch enclosing the developing tooth bud of the right lower third molar (Fig. 1). There was no expansion of the posterior or inferior borders of the ramus, as seen on the panoramic radiograph.
A cone-beam computed tomographic (CBCT) scan was obtained using a Kodak 9000 3D machine (Carestream Health Inc., Rochester, NY, USA), with a field-of-view (FOV) of 50 mm×37 mm, voxel size of 76.5 µm×76.5 µm×76.5 µm, and exposure time of 10.8 s. The captured images were reconstructed using a high-spatial-frequency reconstruction algorithm, and these images revealed a well-defined multiloculated radiolucent lesion in the right mandibular ramal region (Figs. 2A and B). This lesion extended from the right lower second molar to the upper third of the ramus, with resorption of the apex of the right mandibular second molar having well-defined, sharp right-angled septa (Fig. 2C). The radiolucency had scalloped borders and surrounded the developing third molar tooth bud (Figs. 2B and C). There was perforation of the lingual cortical plate and thinning of the buccal cortical plate, as seen on the CBCT coronal section of the lesion (Fig. 2D).
Based on the clinical and radiographic findings, a provisional diagnosis of keratocystic odontogenic tumor due to minimal expansion with considerable bony involvement was proposed with a differential diagnosis of odontogenic myxoma due to the presence of right-angled straight septa, as seen on the reconstructed panoramic section in the CBCT image.
Thereafter, an incisional biopsy of the lesion along with enucleation of the third molar tooth bud was performed under antibiotic coverage and local anesthesia. The specimen was submitted for histopathological evaluation, which revealed a pseudo-stratified, ciliated columnar epithelial cystic lining covering mature fibrous connective tissue. Thus, the overall histopathological findings were suggestive of a GOC. Following these investigations, surgical exploration with curettage of the GOC of the hemimandible was performed under general anesthesia, and the specimen was sent for histopathological confirmation. The hematoxylin and eosin stained section showed cystic lumen lined by pseudo-stratified columnar epithelium with filiform extensions of the cytoplasm and mucous-secreting cells with intra-epithelial spherule formation, which is characteristic of GOCs, thus confirming the previous histopathological diagnosis of GOC (Fig. 3).
After a 3-month follow-up of the patient, no complication or recurrence was reported (Fig. 4).
As stated previously in the Introduction section, a case of GOC, an unusual odontogenic developmental cyst of the jaws, is presented herein. In accordance with previous studies and cases, our case demonstrated significant mandibular involvement.7 In addition, the radiological features showed similarities with previous reports, including a well-defined radiolucency with distinct borders along with loss of cortical integrity and root resorption.
The histopathological features were also suggestive of a cystic cavity lined with pseudo-stratified, ciliated columnar epithelial lining, and fibrous vascular connective tissue.8,9,10,11,12 The disagreement was related to gender predilection, age, and site prevalence: the literature showed a predilection toward males and a mean age of 49.5 years with the anterior mandible being the most-commonly affected site,6,7,13,14 whereas the present case was reported in a young teenage girl with the involvement of the posterior mandible and the ramus region.
GOC recognition based on physical and radiological examinations alone is practically impossible, a fact that the authors of all previous studies harmoniously stress upon. Only histopathological examinations allow for a certain diagnosis of the cyst.15
The GOC does not differ from other jawbone cysts in typical radiological projections. Thus, diagnoses of dentigerous cysts, and botryoid, radicular, and keratocystic odontogenic tumors should be made on the basis of X-ray examinations. Furthermore, in the case of multilocular cysts, the differential diagnosis may shift toward ameloblastoma, myxoma, central giant cell granuloma, and fibrous dysplasia.16 However, the most important diagnosis outcome worthy of consideration is central mucoepidermoid carcinoma due to the significant histopathological similarities.
Kaplan et al6,16 and Brannon et al12 proposed a list of major and minor microscopic criteria for GOC on the basis of the frequency of each feature in the reported cases from the literature. On the basis of their analysis, it was suggested that at least the focal presence of each of the following major criteria must be present for diagnosis: 1) squamous epithelial lining with a flat interface with the connective tissue wall, lacking basal palisading; 2) epithelium exhibiting variations in thickness along the cystic lining with or without epithelial "spheres," "whorls," or focal luminal proliferation; 3) cuboidal eosinophilic cells or "hobnail" cells; 4) mucous (goblet) cells with intraepithelial mucous pools, with or without crypts lined by mucous-producing cells; and 5) intraepithelial glandular, microcystic, or ductlike structures.
In addition, they listed the following minor criteria that supported the diagnosis but were not mandatory: 1) papillary proliferation of the lining epithelium, 2) ciliated cells, 3) multicystic or multiluminal architecture, and 4) clear or vacuolated cells in the basal or spinous layers.
The distinction between low-grade central mucoepidermoid carcinoma and GOC is difficult, if not impossible. The only feature that has not been reported in low-grade central mucoepidermoid carcinoma and that may justify the existence of GOC as a separate entity is the occasional presence of epithelial plaques, similar to those seen in lateral periodontal cysts.17 However, unlike lateral periodontal and botryoid odontogenic cysts, which are more innocuous, GOC is regarded as considerably aggressive.
Our case was considered to be GOC because it fulfilled all criteria specified by Gardner et al,2 and unlike mucoepidermoid carcinoma, cellular atypia and solid and microcystic epithelial proliferation were not seen.
The reported treatment of GOC ranges from a conservative approach (enucleation, marsupialization, curettage with or without peripheral ostectomy, curettage with adjuvant Carnoy's solution, or cryotherapy) to marginal resection and segmental resection. A few authors preferred marginal and segmental resection due to the cyst's tendency to recur after conservative treatment.14
However, it is unlikely that all cases and reports published thus far have used such strict histopathological criteria for GOC recognition. From this recommendation, it can be readily concluded that in a few cases, GOC histopathology can be non-specific to the extent that it is insufficient as the sole test for every suspected case of GOC.18 Therefore, its criteria and clinical features should be identified and used to further refine the diagnosis of cases for which histopathological diagnosis is ambiguous, as well as the differential diagnosis of this cyst (Table 1).18
In conclusion, GOC is a rare and aggressive lesion with a relatively high recurrence rate. Hence, a careful clinical and radiological evaluation along with a meticulous and precise histopathological examination must be carried out. CT or CBCT scans are recommended for diagnosing GOC because they provide accurate information about lesion locularity, cortical integrity, expansion and extent of the lesion, and involvement of the contiguous soft tissue.
Figures and Tables
Fig. 1
A panoramic radiograph shows a well-defined multiloculated radiolucent lesion extending from the distal border and apex of lower right second molar into the ramus till approximately 3 mm away from the sigmoid notch enclosing the developing tooth bud of right lower third molar.

Fig. 2
A. An axial CBCT image shows multiple curved bony septae (black arrows). B. A sagittal CBCT image shows scalloped borders of the cystic lesion (black arrows). C. A reconstructed panoramic CBCT image shows a well-defined radiolucent lesion in the right mandibular ramal region extending from the right lower second molar to the upper third of the ramus with resorption of the apex of the second molar (black arrow) and with well-defined sharp right angle septa (black arrow head). D. A coronal CBCT image shows perforation of the right lingual cortical plate (black arrow head) and thinning of the right buccal cortical plate (white arrow head).

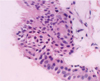
Fig. 3
Histopathologic examination shows cystic lumen lined by pseudo-stratified columnar epithelium with filiform extensions of the cytoplasm and mucous-secreting cells with intra-epithelial spherule formation, characteristic of glandular odontogenic cyst (H&E stain, 400×).
References
1. Padayachee A, Van Wyk CW. Two cystic lesions with features of both the botryoid odontogenic cyst and the central mucoepidermoid tumour: sialo-odontogenic cyst? J Oral Pathol. 1987; 16:499–504.

2. Gardner DG, Kessler HP, Morency R, Schaffner DL. The glandular odontogenic cyst: an apparent entity. J Oral Pathol. 1988; 17:359–366.

3. Kramer IR, Pindborg JJ, Shear M. The WHO histological typing of odontogenic tumours: a commentary on the second edition. Cancer. 1992; 70:2988–2994.
4. Sadeghi EM, Weldon LL, Kwon PH, Sampson E. Mucoepidermoid odontogenic cyst. Int J Oral Maxillofac Surg. 1991; 20:142–143.

5. High AS, Main DM, Khoo SP, Pedlar J, Hume WJ. The polymorphous odontogenic cyst. J Oral Pathol Med. 1996; 25:25–31.

6. Kaplan I, Anavi Y, Hirshberg A. Glandular odontogenic cyst: a challenge in diagnosis and treatment. Oral Dis. 2008; 14:575–581.

8. Nair RG, Varghese IV, Shameena PM, Sudha S. Glandular odontogenic cyst: report of a case and review of literature. J Oral Maxillofac Pathol. 2006; 10:20–23.

9. Gardner DG, Morency R. The glandular odontogenic cyst, a rare lesion that tends to recur. J Can Dent Assoc. 1993; 59:929–930.
10. Krishnamurthy A, Sherlin HJ, Ramalingam K, Natesan A, Premkumar P, Ramani P, et al. Glandular odontogenic cyst: report of two cases and review of literature. Head Neck Pathol. 2009; 3:153–158.

11. Manor R, Anavi Y, Kaplan I, Calderon S. Radiological features of glandular odontogenic cyst. Dentomaxillofac Radiol. 2003; 32:73–79.

12. Brannon RB, Kessler HP, Castle JT, Kahn MA. Glandular odontogenic cyst: analysis of 46 cases with special emphasis on microscopic criteria for diagnosis. Head Neck Pathol. 2011; 5:364–375.
13. Prabhu S, Rekha K, Kumar G. Glandular odontogenic cyst mimicking central mucoepidermoid carcinoma. J Oral Maxillofac Pathol. 2010; 14:12–15.

14. Salehinejad J, Saghafi S, Zare-Mahmoodabadi R, Ghazi N, Kermani H. Glandular odontogenic cyst of the posterior maxilla. Arch Iran Med. 2011; 14:416–418.
15. Łuczak K, Nowak R, Rzeszutko M. Glandular odontogenic cyst of the mandible associated with impacted tooth: report of a case and review of literature. Dent Med Probl. 2007; 44:403–406.
16. Kaplan I, Anavi Y, Manor R, Sulkes J, Calderon S. The use of molecular markers as an aid in the diagnosis of glandular odontogenic cyst. Oral Oncol. 2005; 41:895–902.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download