Abstract
Purpose
This study was performed to investigate the course of the mandibular canal on panoramic radiography and the visibility of this canal on both panoramic radiography and cone-beam computed tomography (CBCT).
Materials and Methods
The study consisted of panoramic radiographs and CBCT images from 262 patients. The course of the mandibular canal, as seen in panoramic radiographs, was classified into four types: linear, elliptical, spoon-shaped, and turning curves. The visibility of this canal from the first to the third molar region was evaluated by visually determining whether the mandibular canal was clearly visible, probably visible, or invisible. The visibihlity of the canal on panoramic radiographs was compared with that on CBCT images.
Results
Elliptical curves were most frequently observed along the course of the mandibular canal. The percentage of clearly visible mandibular canals was the highest among the spoon-shaped curves and the lowest among the linear curves. On panoramic radiographs, invisible mandibular canals were found in 22.7% of the examined sites in the first molar region, 11.8% in the second molar region, and 1.3% in the third molar region. On CBCT cross-sectional images, the mandibular canal was invisible in 8.2% of the examined sites in the first molar region, 5.7% in the second molar region, and 0.2% in the third molar region.
The mandibular canal is an important landmark that should be considered before any surgery in the posterior mandible.1,2,3 Preoperative radiological diagnosis can provide the exact location of the mandibular canal and thus prevent complications during any surgical procedures.4 The course of the mandibular canal has been investigated in several studies, and frequent anatomic variations have been found in the intrabony course of the inferior alveolar nerve.5,6,7 Further, the radiographic appearance of the mandibular canal can be variable.8
The visibility of the mandibular canal may vary significantly, even within the same individual.9,10,11 Wadu et al11 found that in a reasonable number of cases, the radiopaque border is disrupted in radiographic images, and it is invisible in some other cases. The mandibular canal is usually formed by a thin trabecular bone with many circumferentially located voids, and there is a thin layer of cortical bone in only a few mandibles.12,13 Radiological analyses have suggested a correlation between alveolar bone quality and the presence of the mandibular canal wall.14
Previous studies have investigated the visibility of the mandibular canal using panoramic radiography, computed tomography, or cone-beam computed tomography (CBCT).1,15,16,17,18,19,20 On panoramic images, the mandibular canal is typically seen as a well-defined radiolucent zone, lined by radiopaque superior and inferior borders.4 Several researchers have found it difficult at times to identify the mandibular canal on panoramic images.15,16,17,18,19 Computed tomography4,15,16,17 and CBCT1,20 have been superior to conventional imaging modalities for the depiction of the mandibular canal. As a general rule, if the inferior alveolar is poorly depicted on panoramic radiographs, the canal will be difficult to localize using other imaging modalities.21
The understanding of the anatomic variability of the course and visibility of the mandibular canal will be helpful in treatment planning for procedures involving the posterior mandible.22 The aim of this study was to investigate the course of the mandibular canal on panoramic radiographs and to assess the visibility of this canal on panoramic radiographs and CBCT cross-sectional images.
In this retrospective study, the samples were chosen randomly from patients who visited Pusan National University Dental Hospital and underwent panoramic radiography as well as CBCT in 2013. The CBCT scans had been taken as part of a clinical diagnostic procedure for various reasons, such as implant placement, extraction of the third molar, or orthodontic treatment planning. The patients were 140 males and 122 females with a mean age of 29.4 years (age range: 20-60 years). Subjects with mandibular pathology were excluded from the study.
All panoramic radiographs were taken using a Proline XC (Planmeca Co., Helsinki, Finland). CBCT scans were acquired using a PaX-Zenith 3D (Vatech Co., Hwasung, Korea). The scanning parameters were 100-105 kVp, 24 s, 5.0-5.6 mA, voxel size of 0.2 mm, and field of view of 16 cm×14 cm. CBCT images were processed and observed with Ez3D Plus Professional K software (Vatech Co., Hwasung, Korea). Cross-sections were perpendicular to the dental arch, and the occlusal plane served as the reference for cross-sections. The observer carefully examined these images, scrolling through consecutive cross-sectional images.
The course of the mandibular canal, as seen in the panoramic radiographs, was classified into four types: linear, elliptic, spoon-shaped, and turning curves (Fig. 1).23 The visibility of the mandibular canal was evaluated by visually determining whether the mandibular canal was clearly visible, probably visible, or invisible on panoramic radiographs and CBCT cross-sectional images (Fig. 2). It was assessed in three mandibular regions: the first molar, second molar, and third molar regions. The visibility of this canal on panoramic radiographs was compared with that on CBCT images.
Descriptive statistical analysis was applied to the data. The Wilcoxon signed-rank test was used to detect statistically significant differences in the visibility of the mandibular canal between the right and the left sides, and between panoramic radiography and CBCT. The Kruskal-Wallis test was used to examine the difference in the visibility of this canal according to the course of the canal and the difference in visibility in the three mandibular regions. A p value of less than 0.05 was considered to indicate a statistically significant difference. Statistical analyses were performed using IBM SPSS Statistics 21.0 (IBM, Armonk, NY, USA).
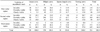
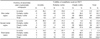
There was no statistically significant difference between the right and the left sides, and the results of both sides were averaged. Elliptic curves were most frequently observed along the course of the mandibular canal (p<0.05) (Table 1). The percentage of clearly visible mandibular canals was highest in spoon-shaped curves and the lowest in linear curves (Tables 2 and 3).
On panoramic radiographs, the percentage of invisible mandibular canals was 22.7% in the first molar region, 11.8% in the second molar region, and 1.3% in the third molar region. On CBCT cross-sectional images, the percentage of invisible mandibular canals was 8.2% in the first molar region, 5.7% in the second molar region, and 0.2% in the third molar region. In the first molar region, the percentage of clearly visible mandibular canals was 13.0% and 50.4% on panoramic radiographs and CBCT, respectively. The CBCT cross-sectional images were significantly better than the panoramic radiographs in assessing the visibility of the mandibular canal (p<0.05). The visibility of this canal in distal regions was significantly better than in the first molar region (p<0.05) (Table 4).
In this study, the course of the mandibular canal was investigated on panoramic radiographs, and the visibility of the canal was assessed on both panoramic images and cross-sectional CBCT images. Our results showed the variation in the course and visualization of this canal.
Several researchers have classified the course of the mandibular canal according to the vertical locations within the mandible, such as high, low, and intermediate locations. 6,7,24 In a study using 96 plain films of dried mandibles, Heasman showed that a majority (68%) of inferior canals passed along an intermediate course between the root apices and the inferior border of the mandible.24 Ozturk et al22 confined classification to the canal's course in the mandibular body: straight projection (12.2%), catenary-like configuration (51.1%), and progressive descent from posterior to anterior (36.7%). This study classified the course of the mandibular canal into linear, spoon-shaped, elliptic, and turning curve types, as in the study conducted by Liu et al.23 A linear curve (22.9%) in our study was very similar to the straight projection (12.2%) observed by Ozturk et al, and the other curves were not similar to their findings.22 In the study conducted by Liu et al,23 elliptic curves (48.5%) were the most common, and spoon-shaped curves (29.3%) were the next most common course. The most common course found in our study was an elliptic curve (64.7%), and this was followed by linear (22.9%) and spoon-shaped curves (6.9%). Elliptic and spoon-shaped curves could provide more space for implant placement than linear curves.
The visibility of the mandibular canal may vary between patients and between different areas of the mandible.1 Klinge et al15 reported that the mandibular canal of specimen cadavers was not visible in 36.1% of panoramic radiographs. Naitoh et al25 reported that on panoramic images, the canal was entirely invisible in 32% of the examined sites in the molar region. In our study, the mandibular canal was not invisible in 22.7% of the examined sites in the first molar region on panoramic radiographs. In addition, Lindh et al26 reported that the mandibular canal of specimen cadavers was clearly visible in 25% of panoramic radiographs. In this study, on panoramic radiographs, the mandibular canal was clearly visible in 13.0% of the examined sites in the first molar region and 46.8% of the examined sites in the third molar region. The depiction of the mandibular canal wall on panoramic images was related to the bone density in the alveolar region.25 Reduced visibility of the mandibular canal wall on a panoramic radiograph might indicate lower integrity of the mandibular canal wall and reduced bone trabeculation.27
The mandibular canal presented overall satisfactory visibility on CBCT cross-sectional images in most cases.1 De Oliveira-Santos et al14 reported that on CBCT cross-sectional images of the first molar region, corticalization of the mandibular canal was observed in 59% of hemimandibles, and in 23% of the cases, the canal was not corticalized but could be visualized. Our results showed that the mandibular canal was clearly visible in 50.4% of the examined sites in the first molar region on CBCT images and was probably visible in 41.4% of the sites. Further, the visibility of the mandibular canal differed according to the course of the mandibular canal on panoramic radiographs. The percentage of clearly visible mandibular canals was the highest in spoon-shaped curves and the lowest in linear curves.
CBCT was found to be superior to panoramic images for the identification of the mandibular canal.19 Kamrun et al4 confirmed that the visibility of cross-sectional CT images was significantly higher than that of panoramic images of the mandibular canal. Our results showed that the visualization of the mandibular canal on panoramic images was remarkably improved by the use of cross-sectional CBCT images.
The mandibular canal was more readily identified in posterior areas, and the visibility gradually decreased towards the mental foramen.1 The most frequently missing portion of the canal was the superior border apical to the first molar.10 The visualization of the canal in the posterior third of the mandibular canal was significantly better than that in the other areas on both panoramic and CBCT images.19 Our results showed that the visibility of the mandibular canal in the third molar region was better than that in the first molar region.
In conclusion, the visibility of the mandibular canal was affected by the course of the canal, and the percentage of clearly visible mandibular canals was the lowest in linear curves. Further, the visibility of the mandibular canal increased in more distal regions of the canal, and the canal was more visible on CBCT cross-sectional images than on panoramic radiographs.
Figures and Tables
Fig. 1
Classifications of the course of the mandibular canal on panoramic radiographs: A. Linear curve, the canal curve is approximately a straight line; B. Elliptic curve, the curve is approximately symmetrical; C. Spoon-shaped curve, the canal has an approximate spoon shape that is similar to an asymmetric elliptic arc; and D. Turning curve, the course is unsmooth and has a turning point.
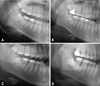
Fig. 2
Classification of the visibility of the mandibular canal on cross-sectional cone-beam computed tomography images: A. Clearly visible, the whole circumference of the bony wall is clearly visible; B. Probably visible, the canal wall is partly visible; and C. Invisible, the canal is not identifiable with certainty.

Table 2
Relationship between the course and the visibility of the mandibular canal on panoramic radiographs
References
1. Oliveira-Santos C, Capelozza AL, Dezzoti MS, Fischer CM, Poleti ML, Rubira-Bullen IR. Visibility of the mandibular canal on CBCT cross-sectional images. J Appl Oral Sci. 2011; 19:240–243.

2. Escoda-Francoli J, Canalda-Sahli C, Soler A, Figueiredo R, Gay-Escoda C. Inferior alveolar nerve damage because of overextended endodontic material: a problem of sealer cement biocompatibility? J Endod. 2007; 33:1484–1489.

3. Tsuji Y, Muto T, Kawakami J, Takeda S. Computed tomographic analysis of the position and course of the mandibular canal: relevance to the sagittal split ramus osteotomy. Int J Oral Maxillofac Surg. 2005; 34:243–246.

4. Kamrun N, Tetsumura A, Nomura Y, Yamaguchi S, Baba O, Nakamura S, et al. Visualization of the superior and inferior borders of the mandibular canal: a comparative study using digital panoramic radiographs and cross-sectional computed tomography images. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013; 115:550–557.

5. Worthington P. Injury to the inferior alveolar nerve during implant placement: a formula for protection of the patient and clinician. Int J Oral Maxillofac Implants. 2004; 19:731–734.
6. Kieser JA, Paulin M, Law B. Intrabony course of the inferior alveolar nerve in the edentulous mandible. Clin Anat. 2004; 17:107–111.

7. Nortjé CJ, Farman AG, Grotepass FW. Variations in the normal anatomy of the inferior dental (mandibular) canal: a retrospective study of panoramic radiographs from 3612 routine dental patients. Br J Oral Surg. 1977; 15:55–63.

8. Anderson LC, Kosinski TF, Mentag PJ. A review of the intraosseous course of the nerves of the mandible. J Oral Implantol. 1991; 17:394–403.
9. Carter RB, Keen EN. The intramandibular course of the inferior alveolar nerve. J Anat. 1971; 108:433–440.
10. Denio D, Torabinejad M, Bakland LK. Anatomical relationship of the mandibular canal to its surrounding structures in mature mandibles. J Endod. 1992; 18:161–165.

11. Wadu SG, Penhall B, Townsend GC. Morphological variability of the human inferior alveolar nerve. Clin Anat. 1997; 10:82–87.

12. Gowgiel JM. The position and course of the mandibular canal. J Oral Implantol. 1992; 18:383–385.
13. Başa O, Dilek OC. Assessment of the risk of perforation of the mandibular canal by implant drill using density and thickness parameters. Gerodontology. 2011; 28:213–220.

14. de Oliveira-Santos C, Souza PH, de Azambuja Berti-Couto S, Stinkens L, Moyaert K, Rubira-Bullen IR, et al. Assessment of variations of the mandibular canal through cone beam computed tomography. Clin Oral Investig. 2012; 16:387–393.

15. Klinge B, Petersson A, Maly P. Location of the mandibular canal: comparison of macroscopic findings, conventional radiography, and computed tomography. Int J Oral Maxillofac Implants. 1989; 4:327–332.
16. Lindh C, Petersson A, Klinge B. Visualisation of the mandibular canal by different radiographic techniques. Clin Oral Implants Res. 1992; 3:90–97.

17. Ylikontiola L, Moberg K, Huumonen S, Soikkonen K, Oikarinen K. Comparison of three radiographic methods used to locate the mandibular canal in the buccolingual direction before bilateral sagittal split osteotomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002; 93:736–742.

18. Kim EK. Comparison of different radiographic methods for the detection of the mandibular canal. Korean J Oral Maxillofac Radiol. 2003; 33:199–205.
19. Angelopoulos C, Thomas SL, Hechler S, Parissis N, Hlavacek M. Comparison between digital panoramic radiography and cone-beam computed tomography for the identification of the mandibular canal as part of presurgical dental implant assessment. J Oral Maxillofac Surg. 2008; 66:2130–2135.

20. Lofthag-Hansen S, Gröndahl K, Ekestubbe A. Cone-beam CT for preoperative implant planning in the posterior mandible: visibility of anatomic landmarks. Clin Implant Dent Relat Res. 2009; 11:246–255.

21. Monsour PA, Dudhia R. Implant radiography and radiology. Aust Dent J. 2008; 53:Suppl 1. S11–S25.

22. Ozturk A, Potluri A, Vieira AR. Position and course of the mandibular canal in skulls. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012; 113:453–458.

23. Liu T, Xia B, Gu Z. Inferior alveolar canal course: a radiographic study. Clin Oral Implants Res. 2009; 20:1212–1218.

24. Heasman PA. Variation in the position of the inferior dental canal and its significance to restorative dentistry. J Dent. 1988; 16:36–39.

25. Naitoh M, Katsumata A, Kubota Y, Hayashi M, Ariji E. Relationship between cancellous bone density and mandibular canal depiction. Implant Dent. 2009; 18:112–118.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download