Abstract
Glandular odontogenic cyst (GOC) is a rare, potentially aggressive jaw lesion. The common radiographic features include a well-defined radiolucency with distinct borders, presenting a uni- or multilocular appearance. A cystic lesion in the posterior mandible of a 78-year-old female was incidentally found. Radiographs showed a unilocular lesion with a scalloped margin, external root resorption of the adjacent tooth, and cortical perforation. This lesion had changed from a small ovoid shape to a more expanded lesion in a period of four years. The small lesion showed unilocularity with a smooth margin and a well-defined border, but the expanded lesion produced cortical perforation and a lobulated margin. The provisional diagnosis was an ameloblastoma, whereas the histopathological examination revealed a GOC. This was a quite rare case, given that this radiographic change was observed in the posterior mandible of an elderly female. This case showed that a GOC can grow even in people in their seventies, changing from the unilocular form to an expanded, lobulated lesion. Here, we report a case of GOC with characteristic radiographic features.
Glandular odontogenic cyst (GOC) is known as a slowly growing, painless, but aggressive lesion. The potentially aggressive nature of the lesion was suggested by penetration of the cortical bone and high incidence of recurrence after conservative treatment.1 GOC is a rare lesion with an incidence of 0.2% of odontogenic cysts.2 It affects males twice as frequently as females and the mandible almost three times as frequently as maxilla.3 The age range is 14-75 years, and the mean age is 45.7 years.2 It is a recently described cystic lesion among odontogenic cysts.4 In 1987, Padayachee and Van Wyk5 first reported the sialo-odontogenic cyst; this cyst was later renamed GOC by Gardner et al.6 Although few cases of GOC have been reported thus far, its usual radiographic features have been found to be uni/multilocular lesions with frequent cortical perforation, tooth displacement, and root resorption of the adjacent teeth.2,3,7,8 However, the radiographic diagnosis can be challenging due to similarities in radiographic features between the GOC and the other radiolucent jaw lesions because there are no radiological features distinctive for GOC.9,10
The radiograph of this case showed a well-defined, lobulated radiolucent lesion occurring in the posterior mandible. The provisional diagnosis was an ameloblastoma. However, the histopathological examination diagnosed a cyst fulfilling the criteria for a GOC. We believe that this case shows interesting and characteristic radiographic features of GOC.
This case shows that a GOC can grow in people in their seventies, changing from a unilocular lesion to an expanded, lobulated lesion over a period of time. The periodic radiographs showed the changes in the lesion shape and the lobular margin that took place during a period of four years. Furthermore, it is a rare case in that the above mentioned radiographic changes were observed in the posterior mandible of an elderly woman. Here, we report this interesting case of GOC with characteristic radiographic jaw features and a literature review.
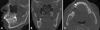
A 78-year-old female was referred from a local clinic to Wonkwang Dental Hospital for a cystic lesion in the left mandibular posterior region. This lesion was incidentally observed on a panoramic radiograph. There were no remarkable clinical findings except tooth mobility (++) of the left mandibular second molar. The past medical history revealed that the patient had experienced some facial trauma four years ago. The facial computed tomography (CT) taken at the medical hospital showed no definite bony fracture line on the facial bone, but there was a cystic lesion on the left mandibular angle that had not been reported by the medical radiologist. This cystic lesion had a unilocular ovoid shape (11.8 mm×5.2 mm) (Fig. 1) and was incidentally, retrospectively observed at our dental hospital after four years by an oral radiologist.
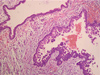
A panoramic radiograph and cone-beam CT (CBCT) were taken at the dental hospital. The panoramic radiograph showed a lobulated lesion with a well-defined, scalloped margin from the left lower second molar to the left mandibular ramus, with slight involvement of the apices of the mandibular second molar. There was no tooth displacement, but the external root resorption of the second molar was remarkable (Fig. 2). The CBCT represented a lobulated margin and the thinning, erosion, and perforation of the lingual cortex. Further, a mild expansion of the lingual cortex was observed. This lesion had changed into a more expanded ovoid shape (26.0 mm×11.3 mm) (Fig. 3). The provisional diagnosis was an ameloblastoma due to the extensive root resorption. Because of the rare occurrence of GOC in the jaw, we did not consider GOC for the differential diagnosis.
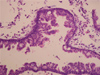
The histopathological examination showed multiple cystic compartments. The cyst was lined by several surface eosinophilic cuboidal cells exhibiting apocrine snouting. Microcysts and papillary projections that had formed adjacent to "open" microcysts were also noted. Cilia were not evident (Figs. 4 and 5). The histopathological diagnosis was GOC.
The treatment was composed of the extraction of the lower second molar, cyst enucleation, and peripheral osteotomy. We carried out close follow-up for recurrence.
This report described a very rare case of GOC, which was found in the posterior mandible of an elderly female. The lesion had showed various radiographic features during the past four years. The lesion shape had changed from a small ovoid shape to that of a more expanded cyst. The small lesion had shown unilocularity and a well-defined border, whereas the expanded lesion produced cortical perforation and a lobulated margin. All GOCs larger than 6 cm in diameter showed perforated margins radiologically in a case report by Noffke and Raubenheimer.11 In this case, cortical perforation and erosion were also observed, suggesting its aggressiveness; however, the mild expansion of the lingual cortex represents the benign nature of the lesion. There was no tooth displacement, but extensive external root resorption of the second molar was seen (Fig. 2). Therefore, we suspected ameloblastoma because ameloblastoma commonly presents extensive root resorption of the adjacent tooth; however, the patient's old age (78 years) was a factor responsible for the hesitation in the radiographic diagnosis. Ameloblastoma usually presents in the second half of the fourth decade, whereas the age range of GOC was reported to be 14-85 years (mean age: 49 years) and the majority of patients were older than 40 years.11 In contrast, East Asians with GOCs were nearly a decade younger.3 Another possible lesion was keratocystic odontogenic tumor (KCOT). KCOT is commonly found in the posterior mandible, in patients between 10 and 30 years of age.12 Resorption of the adjacent root is less common. Although radiologically, the GOC lacked specific features, making the distinction from ameloblastoma and KCOT difficult, the radiographic appearance of multiple foci of the cortical perforation in this case was helpful in distinguishing the GOC from ameloblastoma and KCOT.11 Other jaw lesions necessary for a radiographic differential diagnosis with GOC include the central giant cell lesion, lateral periodontal cyst, botryoid odontogenic cyst, simple bone cyst, and central mucoepidermoid tumor depending on the multilocularity.11,13
Numerous histopathological features for the GOC have been described, but the exact microscopic criteria necessary for the diagnosis have not been universally accepted. Furthermore, some of the microscopic features of GOC might be found in dentigerous, botryoid, radicular, and surgical ciliated cysts.14 Kaplan et al2,13 added that a diagnosis of GOC had to be based on the mandatory presence of the following five major features: squamous epithelium, varying thickness, cuboidal eosinophilic (hobnail) cells, mucous (goblet) cells, and intraepithelial glandular or duct-like structures. The histopathology of this cyst consisted of cuboidal epithelial cells with papillary projections extending into the lumen. Occasional very small duct-like structures were seen to be lined by cuboid or polygonal cells. Cilia were not visible on the surface epithelium (Figs. 4 and 5). These histopathological findings were compatible with those of GOC as described by Kaplan et al. The clinical importance of GOC relates to the fact that it has a high recurrence rate2 and an aggressive growth potential15 and that it may be confused microscopically with central mucoepidermoid carcinoma.14 The lesions vary considerably in size and aggressiveness, and the treatment ranges from simple curettage to marginal resection.16 A more aggressive surgical removal rather than simple curettage was suggested, and cases should be followed up carefully.11 Cyst enucleation and peripheral osteotomy for safe removal were performed for this patient, and close follow-ups have been carried out for recurrence.
Considering our case of GOC with characteristic radiographic features, we can conclude that GOC can grow in people in their seventies, changing from a unilocular form to a lobulated lesion in a few years.
Figures and Tables
Fig. 1
Axial (A) and coronal (B) computed tomography images show an ovoid, unilocular cystic lesion on the left mandibular angle.

Fig. 2
The panoramic radiograph shows an ovoid, lobulated lesion with a well-defined margin from the left lower second molar to the left mandibular ramus. The external root resorption of the second molar is remarkable.

References
1. Hussain K, Edmondson HD, Browne RM. Glandular odontogenic cysts. Diagnosis and treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995; 79:593–602.
2. Kaplan I, Anavi Y, Hirshberg A. Glandular odontogenic cyst: a challenge in diagnosis and treatment. Oral Dis. 2008; 14:575–581.

3. Macdonald-Jankowski DS. Glandular odontogenic cyst: systematic review. Dentomaxillofac Radiol. 2010; 39:127–139.

4. Kramer IR, Pindborg JJ, Shear M. Histological typing of odontogenic tumors. 2nd ed. Berlin/New York: Springer Verlag;1992.
5. Padayachee A, Van Wyk CW. Two cystic lesions with features of both the botryoid odontogenic cyst and the central mucoepidermoid tumour: sialo-odontogenic cyst? J Oral Pathol. 1987; 16:499–504.

6. Gardner DG, Kessler HP, Morency R, Schaffner DL. The glandular odontogenic cyst: an apparent entity. J Oral Pathol. 1988; 17:359–366.

7. Manor R, Anavi Y, Kaplan I, Calderon S. Radiological features of glandular odontogenic cyst. Dentomaxillofac Radiol. 2003; 32:73–79.

8. Tambawala SS, Karjodkar FR, Yadav A, Sansare K, Sontakke S. Glandular odontogenic cyst: a case report. Imaging Sci Dent. 2014; 44:75–79.

9. Ramer M, Montazem A, Lane SL, Lumerman H. Glandular odontogenic cyst: report of a case and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997; 84:54–57.
10. Koppang HS, Johannessen S, Haugen LK, Haanaes HR, Solheim T, Donath K. Glandular odontogenic cyst (sialo-odontogenic cyst): report of two cases and literature review of 45 previously reported cases. J Oral Pathol Med. 1998; 27:455–462.

11. Noffke C, Raubenheimer EJ. The glandular odontogenic cyst: clinical and radiological features; review of the literature and report of nine cases. Dentomaxillofac Radiol. 2002; 31:333–338.

12. White SC, Pharoah MJ. Oral radiology: principles and interpretation. 4th ed. St. Louis: Mosby;1999. p. 364.
13. Kaplan I, Anavi Y, Manor R, Sulkes J, Calderon S. The use of molecular markers as an aid in the diagnosis of glandular odontogenic cyst. Oral Oncol. 2005; 41:895–902.

14. Fowler CB, Brannon RB, Kessler HP, Castle JT, Kahn MA. Glandular odontogenic cyst: analysis of 46 cases with special emphasis on microscopic criteria for diagnosis. Head Neck Pathol. 2011; 5:364–375.

15. Shear MS, Speight PM. Cysts of the oral and maxillofacial regions. 4th ed. Oxford: Blackwell Pub;2007. p. 94–99.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download