Abstract
A 28-year-old male patient with a history of cystic fibrosis (CF) was referred to the University of Connecticut School of Dental Medicine for an evaluation of a cystic lesion in the right maxilla using cone-beam computed tomography (CBCT). CF is an autosomal recessive disease characterized by an abnormal production of viscous mucus, affecting the mucociliary clearance. The CBCT scan revealed a large cystic lesion in the right maxilla extending from the right maxillary second molar to the midline in the region of the right central incisor with a significant buccal expansion. Further evaluation revealed complete opacification of the paranasal sinuses with medial bulging of the lateral maxillary sinus walls. The maxillary and sphenoid sinuses also appeared hypoplastic. The peculiar finding seen in this case was the presence of marked sclerosis and an increase in the thickness of the adjacent bony framework. This report aimed to describe the common sinonasal findings associated with CF and its underlying pathophysiology.
Cystic fibrosis (CF) is a chronic inherited disease affecting more than 30,000 children and adults in the United States and 80,000 people worldwide.1 It is a multisystem disorder caused by mutations in the gene encoding CF transmembrane conductance regulator (CFTR).2 CFTR is a protein involved in the transport of chloride ions across cell membranes or the gene that encodes this protein. It is present in the epithelium of most of the body lumen and regulates the sodium and water balance. A dysfunction of this subtle balance severely affects the airway epithelium, increases viscosity of the mucous, and in turn, causes a reduction in the mucociliary clearance, which consequently leads to bacterial retention. CF most commonly leads to pancreatic insufficiency, electrolyte imbalance, gastrointestinal manifestations, elevated sweat and chloride levels, infertility in males, and obstructive sinopulmonary disease.2,3,4
Chronic sinusitis associated with CF has a different underlying pathophysiology as described above. Nishioka et al found a significant difference in the appearance of the paranasal sinuses on computed tomography (CT), such as agenesis of the frontal sinus, medial bulging, and extensive maxilloethmoidal opacification in CF patients as compared to non-CF patients.5 However, CT can only determine the extent of opacification and cannot differentiate between thickened mucosa and pus.6 Eggesbø et al assessed the role of magnetic resonance imaging (MRI) by utilizing short inversion time inversion recovery (STIR) and T1-weighted sequences and found three major patterns in the maxillary sinus lumen: air-filled, oval pus-filled, and streak-shaped pus-filled lumen.6
Long-standing inflammation caused by sinonasal polyposis and sinusitis when involving the adjacent bony framework of the paranasal sinuses leads to localized osteitis. This osteitis coupled with chronic rhinosinusitis is known as osteitic rhinosinusitis. Cone-beam computed tomography (CBCT) is a three-dimensional imaging modality that is gaining widespread use in the field of dentistry.7 Radiographic findings specifically associated with the maxillofacial skeleton in CF patients need to be evaluated thoroughly by a trained oral and maxillofacial radiologist in order to understand the severity of the disease and to make appropriate referrals as deemed necessary. The aims of this case report were to report an unusual presentation of chronic rhinosinusitis involving the bony framework of the paranasal sinuses, and to describe the common radiographic appearances of the sinonasal complex in patients with CF.
A 28-year-old male patient complaining of pain and mild swelling on the right side of the maxilla for over a period of one year with a known medical history of CF was referred to the Oral and Maxillofacial Surgery Clinic at the University of Connecticut School of Dental Medicine. Panoramic imaging revealed a large cystic-appearing lesion extending from the right maxillary second molar to the midline in the region of the right central incisor (Fig. 1). A further evaluation of the lesion was deemed necessary and the patient was referred to the Advanced Oral and Maxillofacial Imaging Center at the University of Connecticut School of Dental Medicine. A CBCT exam was done using a Hitachi CB MercuRay (Hitachi Medical Corporation, Tokyo, Japan) CBCT machine with a 12-inch field of view. The acquisition parameters were set at 120 kVp and 15 mA with an acquisition time of 10 s for the device that does a 360° rotation around the patient; image acquisition was done with the patient in an upright position. The scan generated 256 basis projections and reconstructed 512 images. The images were viewed in the multiplanar reformat mode with the ability to reconstruct the entire area as a single volumetric projection.
CBCT images revealed a well-defined, corticated, ellipsoidal, expansile radiolucent lesion in the right maxilla extending from the region of the right second molar to the midline in the region of the right central incisor. This lesion measured approximately 44 mm×22 mm×31 mm at the greatest right-angled diameters. The margins were undulated, and expansion was particularly marked on the buccal aspect (Fig. 2), while superiorly, the lesion extended well below the floor of the right maxillary sinus. No internal calcifications were present. The radiographic differential diagnosis of a keratocystic odontogenic tumor (KOT) was made; although after follow-up, the aspiration fluid revealed only an inflammatory exudate.
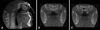
The maxillary sinuses appeared hypoplastic, round to ovoid in shape on the axial slices, with severe mucosal thickening and complete opacification (Fig. 3). Ostia were enlarged significantly with erosive changes in the lateral wall of the nasal cavity, highly suggestive of sinonasal polyposis. The anterior, lateral, and posterior walls of both maxillary sinuses showed severe sclerosis. Complete opacification of the anterior and posterior ethmoidal air cells (Fig. 4A) was noted bilaterally with sclerosis of the adjacent bony framework. An additional finding was the presence of an osteoma in the left ethmoidal air cells (Fig. 4B). The imaged portions of the orbital roofs also appeared sclerotic. The sphenoid sinus appeared severely hypoplastic with complete opacification and sclerosis of the body and a part of the greater wing of the sphenoid bone (Fig. 5).
Although the predominant findings associated with CF are in the lower airway, the membrane linings of the nasal cavity and the paranasal sinuses are identical to those in the lungs.8,9,10 Thus, the pathophysiology of the disease process is essentially the same as that in the lower respiratory system. The most common sinonasal pathogens in CF patients are Pseudomonas aeruginosa, Hemophilius influenza, Staphylococcus aures, and anaerobic species.7 Bacterial colonization can also act as a secondary inflammatory inducer that leads to goblet cell hyperplasia, squamous cell metaplasia, and loss of cilia. The common symptoms associated with sinonasal involvement are nasal obstruction, rhinorrhea, facial pain, headache, and anosmia,8 although the incidence of clinical and self-reported sinonasal symptoms associated with CF is low. A study conducted by King et al showed that only 10% of the patients with CF complain about sinonasal symptoms.11 Eggesbø et al found significant developmental variation of paranasal sinuses in CF patients.12 The common CT findings are frontal sinus aplasia, hypoplasia of maxillary sinuses, severely hypoplastic sphenoid sinuses with sclerotic borders, and reduced diameter of ethmoidal air cells as compared to normal individuals. Although the pathogenesis of the development of paranasal sinuses in CF patients is not completely known, the presence of local chronic sinusitis during childhood is a suggested cause for aplasia and agenesis. Reduced oxygen saturation due to sinus polyposis or sinusitis is also considered one of the factors in the developmental variations of the paranasal sinus.12 In this case, all the findings are consistent with those of Eggesbø et al except that the frontal sinus is not imaged and hence, not visualized in the imaged field of view. Another important finding seen in this case is the presence of the medial bulging of the lateral sinus wall with opacification of a part of the nasal fossa at the level of the ostium. These processes clearly indicate the pressure effect. This finding was consistent with the findings of Nishioka et al,5 Eggesbø et al (82% of cases),13 and April et al (74% cases),14 who found the presence of medial bulging exclusively in the CF group and suggested that this finding could be the characteristic that could lead to the diagnosis of CF. The anterior ethmoidal air cells in this patient were completely opacified, while posterior cells showed areas of air density, which is again consistent with the findings of Eggesbø et al. Gentile and Isaacson15 found a correlation between the CT appearance of the sinonasal complex and the pattern of sinusitis in terms of the symptoms and the physical findings.
The additional but peculiar finding associated with this case is the involvement of the adjacent bony framework of paranasal sinuses. The walls of maxillary sinuses showed significant sclerosis and thickening with areas of small radiolucent foci. Other sinuses showed similar findings, particularly the marked sclerosis adjacent to the severely hypoplastic sphenoid sinus. These findings could be associated with an underlying inflammatory process in the paranasal sinuses. Histological studies conducted by Kennedy et al16 showed that the peri-sinus bone remodeling appears identical to that seen in osteomyelitis. Osteitis and osteomyelitis may show similar histologic features, including bone remodeling and inflammatory infiltrate,17 but radiographically, their appearance may vary with the type of bone involved. Cho et al demonstrated marked bone remodeling, including periosteal thickening and neo-osteogenesis with woven bone formation, in chronic rhinosinusitis patients, and the correlations were identified radiographically on the CT acquisitions.18 However, to the best of our knowledge, in English literature, such peri-sinus bone changes have not been reported in CF patients.
Apart from CF, many other risk factors are associated with the development of chronic rhinosinusitis,19 and CT is commonly utilized for the evaluation of the inflammatory conditions of the paranasal sinuses. The common CT appearance of chronic rhinosinusitis includes mucoperiosteal thickening, partial-to-complete opacification, air-fluid levels, and sclerosis of the adjacent bony framework. Since bones in the paranasal sinuses are flat and consist of relatively little or no marrow, the term "osteitis" can be used when such a bone is inflamed. Other terms such as chronic osteitis, neo-osteogenesis, and osteoneogenesis have been used to describe the thickened, sclerosed walls of the sinus seen on the CT.20
Georgalas et al developed the global osteitis scoring scale to grade both the extent and the severity of the radiologically defined osteitis in chronic rhinosinusitis. Grading is based on the involvement of the sinus wall and the thickness of osteitis, although in this study, we found no link between the severity of the symptoms and the radiographic evidence of osteitis.21
Due to technological advances, new-generation CBCT scanners provide an opportunity to adjust the field of view according to the diagnostic need at a relatively low radiation dose and high spatial resolution. This technology can be effectively utilized for grading and staging chronic sinonasal inflammatory conditions, such as those seen in CF and multifactorial chronic rhinosinusitis. With the ubiquitous availability of CBCT scanners and an increasing number of scans being done for three-dimensional evaluations of the maxillofacial structures by dentists, it is very useful to recognize the sinonasal manifestations of cystic fibrosis to aid in an overall team-based management of the patient.
Figures and Tables
Fig. 1
Panoramic image shows a large cystic lesion extending from the right maxillary second molar to the midline in the region of the right central incisor.
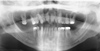
Fig. 2
Axial cone-beam computed tomography (CBCT) image shows an expansile cystic lesion in the right maxilla with thinning of the buccal cortical plate.
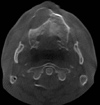
Fig. 3
A. Axial CBCT image at the level of maxillary sinuses shows hypoplastic-appearing maxillary sinuses with complete opacification and sclerosis of the adjacent bony walls. B. Coronal CBCT image shows complete opacification of maxillary sinuses with enlarged ostium (white arrow), sclerosis, and thickening of the adjacent bone (white arrow).

References
1. Boucher RC, Knowles MR, Yankaskas JR. Cystic fibrosis. In : Mason RJ, Broaddus VC, Martin T, King T, Schraufnagel DM, Murray JE, editors. Murray and Nadel's textbook of respiratory medicine. 5th ed. Philadelphia: Elsevier;2010. p. 985–1022.
2. Matsui H, Grubb BR, Tarran R, Randell SH, Gatzy JT, Davis CW, et al. Evidence for periciliary liquid layer depletion, not abnormal ion composition, in the pathogenesis of cystic fibrosis airways disease. Cell. 1998; 95:1005–1015.

4. Lobo J, Rojas-Balcazar JM, Noone PG. Recent advances in cystic fibrosis. Clin Chest Med. 2012; 33:307–328.

5. Nishioka GJ, Cook PR, McKinsey JP, Rodriguez FJ. Paranasal sinus computed tomography scan findings in patients with cystic fibrosis. Otolaryngol Head Neck Surg. 1996; 114:394–399.

6. Eggesbø HB, Dølvik S, Stiris M, Søvik S, Storrøsten OT, Kolmannskog F. Complementary role of MR imaging of ethmomaxillary sinus disease depicted at CT in cystic fibrosis. Acta Radiol. 2001; 42:144–150.

7. Scarfe WC, Farman AG. What is cone-beam CT and how does it work? Dent Clin North Am. 2008; 52:707–730.

8. Chang EH. New insights into the pathogenesis of cystic fibrosis sinusitis. Int Forum Allergy Rhinol. 2014; 4:132–137.

9. Berkhout MC, Rijntjes E, El Bouazzaoui LH, Fokkens WJ, Brimicombe RW, Heijerman HG. Importance of bacteriology in upper airways of patients with cystic fibrosis. J Cyst Fibros. 2013; 12:525–529.

10. Gysin C, Alothman GA, Papsin BC. Sinonasal disease in cystic fibrosis: Clinical characteristics, diagnosis, and management. Pediatr Pulmonol. 2000; 30:481–489.

11. King VV. Upper respiratory disease, sinusitis, and polyposis. Clin Rev Allergy. 1991; 9:143–157.

12. Eggesbø HB, Søvik S, Dølvik S, Eiklid K, Kolmannskog F. CT characterization of developmental variations of the paranasal sinuses in cystic fibrosis. Acta Radiol. 2001; 42:482–493.

13. Eggesbø HB, Søvik S, Dølvik S, Kolmannskog F. CT characterization of inflammatory paranasal sinus disease in cystic fibrosis. Acta Radiol. 2002; 43:21–28.

14. April MM, Zinreich SJ, Baroody FM, Naclerio RM. Coronal CT scan abnormalities in children with chronic sinusitis. Laryngoscope. 1993; 103:985–990.

15. Gentile VG, Isaacson G. Patterns of sinusitis in cystic fibrosis. Laryngoscope. 1996; 106:1005–1009.

16. Kennedy DW, Senior BA, Gannon FH, Montone KT, Hwang P, Lanza DC. Histology and histomorphometry of ethmoid bone in chronic rhinosinusitis. Laryngoscope. 1998; 108:502–507.

18. Cho SH, Min HJ, Han HX, Paik SS, Kim KR. CT analysis and histopathology of bone remodeling in patients with chronic rhinosinusitis. Otolaryngol Head Neck Surg. 2006; 135:404–408.

19. Loebinger MR, Bilton D, Wilson R. Upper airway 2: bronchiectasis, cystic fibrosis and sinusitis. Thorax. 2009; 64:1096–1101.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download