Abstract
Purpose
To investigate the prevalence of bifid and trifid mandibular canals using cone-beam computed tomography (CBCT) images, and to measure their length, diameter, and angle.
Materials and Methods
CBCT images of 500 patients, involving 755 hemi-mandibles, were used for this study. The presence and type of bifid mandibular canal was evaluated according to a modified classification of Naitoh et al. Prevalence rates were determined according to age group, gender, and type. Further, their diameter, length, and angles were measured using PACSPLUS Viewer and ImageJ 1.46r. Statistical analysis with chi-squared and analysis of variance (ANOVA) tests was performed.
Results
Bifid and trifid mandibular canals were found in 22.6% of the 500 patients and 16.2% of the 755 sides. There was no significant difference between genders and among age groups. The retromolar canal type accounted for 71.3% of the identified canals; the dental canal type, 18.8%; the forward canal type, 4.1%; and the trifid canal type, 5.8%. Interestingly, seven cases of the trifid canal type, which has been rarely reported, were observed. The mean diameter of the bifid and trifid mandibular canals was 2.2 mm and that of the main mandibular canal was 4.3 mm. Their mean length was 16.9 mm; the mean superior angle was 149.2°, and the mean inferior angle was 37.7°.
The location and the configuration of the mandibular canal are important in surgical procedures involving the mandible, such as the extraction of the impacted third molar, dental implant treatment, and sagittal split ramus osteotomy.1 Anatomical variations of the mandibular canal, such as the bifid or trifid mandibular canal, have been reported using panoramic radiography,2,3,4,5,6,7,8,9 computed tomography (CT),10,11,12 and cone-beam CT (CBCT).1,13,14,15,16,17,18,19,20 Radiological studies using panoramic radiography showed lower incidence rates than those using CT and CBCT. Localization of the mandibular canal might be difficult on the panoramic radiograph, because the mandibular ramus region would overlap with the opposite side of the mandible, soft palate, and pharynx on the images.1 CT and CBCT are superior to panoramic radiography in displaying the mandibular canal and their variations because these imaging modalities provide high-resolution, three-dimensional images.15,17 The bifid mandibular canals were found in 0.08%-0.95% of the cases when evaluating panoramic radiographs,2,8 and 10.2%-65% of the cases when using CBCT images.1,15,20
Several researchers1,2,3,4 classified the bifid mandibular canals according to their anatomic location and configuration by using panoramic radiographs and CBCT images. Some of them2,3,4 classified these canals using panoramic radiographs, and Naitoh et al1 classified them into four main patterns - retromolar type, dental type, forward type, and buccolingual type - by using CBCT imaging. They did not include the trifid canal type, but a few cases of trifid mandibular canals have been reported.6,18 In addition, the length,1,16,19,20 diameter,1,17,19,20 and angle16 of the bifid mandibular canals measured according to type were reported.
The objectives of the present study were to investigate the prevalence of bifid and trifid mandibular canals through an analysis of CBCT images, and to measure their length, diameter, and angle.
CBCT images of 500 patients (755 hemi-mandibles) who visited Dankook University Dental Hospital between January 2012 and May 2012 for the extraction of the impacted mandibular third molar were used for this study. They were taken with an Alphard VEGA CBCT scanner (Asahi Roentgen Ind. Co., Ltd., Kyoto, Japan). The exposure volume was set at a diameter of 102 mm and height of 102mm(I mode; voxel size: 0.2 mm), or at a diameter of 51 mm and height of 51 mm (D mode; voxel size: 0.1 mm). I-mode CBCT images were taken at the exposure parameters of 80 kV, 7 mA, and 17 s, and D-mode images were taken at the exposure parameters of 80 kV, 8 mA, and 17 s.
The bifid mandibular canal was classified into five types by anatomic location and configuration as described below. One group of the trifid canal type was added to the classification of Naitoh et al.1
Type 1 (Retromolar canal type): The retromolar canal, which bifurcates from the mandibular canal in the mandibular ramus region, courses forward at first, reaching the retromolar region after the crook (Fig. 1).
Type 2 (Dental canal type): The dental canal, which bifurcates from the mandibular canal in the mandibular ramus region, courses forward, reaching the root of the molar (Fig. 2).
Type 3 (Forward canal type): A. Forward canal without confluence: The forward canal, which bifurcates from the mandibular canal in the mandibular ramus region, courses forward to the second molar region (Fig. 3A). B. Forward canal with confluence: The forward canal, which bifurcates from the mandibular canal in the mandibular ramus, courses anteriorly and then, joins the main mandibular canal (Fig. 3B).
Type 4 (Buccolingual canal type): A. Lingual canal: The lingual canal, which bifurcats from the mandibular canal in the mandibular ramus, courses lingually and then penetrates through the lingual cortical bone. B. Buccal canal: The buccal canal, which bifurcates from the mandibular canal in the mandibular ramus, courses bucco-inferiorly.
Type 5 (Trifid canal type): A. Two accessory canals of the retromolar canal type (Fig. 4). B. Two accessory canals of one retromolar and one dental canal type (Fig. 5). C. Two accessory canals of the dental canal type (Fig. 6). D. Two accessory canals of one dental and one forward canal type (Fig. 7). E. Two accessory canals of the retromolar canal type with two mandibular foramina (Fig. 8).
The presence and the type of bifid mandibular canal were evaluated at the left and right posterior mandibles by the consensus of three oral and maxillofacial radiologists. The images were evaluated on a high-resolution, 5-megapixel mono-display monitor (IF2105M, Wide Corp., Yongin, Korea). The prevalence rate was calculated according to age group, gender, and type.
The diameter of the main mandibular canal was measured immediately after bifurcation on the cross-sectional image and that of the bifid mandibular canal at the widest portion of the bifid canal. They were measured using PACS Plus Viewer (Medical Standard Co., Ltd., Seoul, Korea).
The length of the bifid mandibular canal was measured from the bifurcated point to the end point that is observable on panoramic reconstructed images using the ImageJ 1.46r program (Wayne Rasband, NIH, USA), which allows the observer to measure the curved structure.
The superior and inferior angles of the bifid mandibular canal were measured on panoramic reconstructed images using the ImageJ 1.46r program. The superior angle was measured between the main canal and the superior wall of the bifid canal and the inferior angle between the main canal and the inferior wall of the bifid canal.
Differences in the prevalence rate of the bifid mandibular canal according to age group, gender, and type were evaluated using the chi-squared and analysis of variance (ANOVA) tests. Differences in diameters, lengths, and the angles among types were assessed using the ANOVA test by means of IBM SPSS Statistics version 19 (IBM Corp., Somers, NY, USA).
Bifid mandibular canals were found in 22.6% of the 500 patients and 16.2% of the 755 sides (Table 1). There was no significant difference at the prevalence between genders and among age groups (Tables 2 and 3). The retromolar canal type was the most common (71.3%), followed by the dental canal type (18.8%), the trifid type (5.8%), and the forward type (4.1%) (Table 4).
Table 5 shows the mean diameters of the bifid mandibular canal and the main mandibular canal according to the abovementioned classification. The mean diameter of the bifid mandibular canal was 2.2 mm and that of the main mandibular canal was 4.3 mm. There was no statistically significant difference among each type.
The mean lengths of the bifid mandibular canal according to type are listed in Table 6. The mean length of the bifid mandibular canal was 16.9 mm. There was a statistically significant difference between the dental canal type and the trifid canal type.
The mean angles of the bifid mandibular canal according to type are listed in Table 7. The mean superior angle of the bifid mandibular canal was 149.2°, and the mean inferior angle of the bifid mandibular canal was 37.7°. There was no statistically significant difference among the superior angles of each type. In the case of the inferior angle, there was a statistically significant difference between the retromolar canal and the dental canal types, and between the retromolar canal and the trifid canal types.
The bifid mandibular canal was found in 22.6% of the 500 patients, and the retromolar canal type was observed to be the most common. When the prevalence rate was compared according to age and gender, there was no significant difference between genders and among age groups. The bifid and trifid variations of the mandibular canal have been reported using different imaging modalities. Studies using panoramic radiographs have demonstrated the prevalence of the bifid mandibular canal at low rates ranging from 0.08% to 0.95%.2,8 However, those using CT and CBCT images have reported incidence rates of the bifid mandibular canal ranging from 10.2% to 65%.1,15,17,19,20 Since CT and CBCT can provide high-resolution three-dimensional images, it can detect accessory canals with a narrow diameter and those that bifurcate in any direction. CT or CBCT is considered a suitable modality for a detailed evaluation of the presence of bifid mandibular canals.11,15,20,21 Wide variations of the prevalence rate were reported in different countries - 46.5% in Turkey,16 19% in Belgium,17 30.6% in Taiwan,19 and 15.6%-65% in Japan.1,15 The prevalence rate of 10.2% in the Korean population as reported by Kang et al20 was lower than the 22.6% found for the Korean population in this study. They demonstrated that the retromolar canal type was the most common and the buccolingual canal type, the least common,20 which is similar to our results.
Several classifications of the mandibular canal according to the anatomical location and configuration have been used in previous studies. Carter and Keen3 examined dissected human mandibles and described three types of inferior alveolar nerve arrangement: single canal, lower canal, and duplicated canal. Nortje et al4 described three main patterns of duplication: type 1 was two canals originating from one foramen; type 2, a short upper canal extending to the second or the third molar teeth; and type 3, two mandibular canals of equal dimensions apparently arising from separate foramina in the mandibular ramus and joining in the molar region. Langlais et al2 classified the mandibular canals into four types according to the anatomical location and configuration using panoramic radiography, and Naitoh et al1 classified them into four types using CBCT images: retromolar, dental, forward, and buccolingual canal. They observed the forward canal type (59.6%), retromolar canal type (29.8%), dental canal type (8.8%), and buccolingual canal type (1.8%).1 Orhan et al16 used the classification of Naitoh et al for a Turkish population and reported that the most frequently encountered type was the forward canal type, followed by the retromolar canal type.16 In contrast, Kuribayashi et al15 following the classification of Nortje et al demonstrated that Type II (dental canal type) was the most common. Fu et al19 observed the bifid canal in 30.6% of the Taiwanese subjects, and more than half were the dental or retromolar type. In the present study, we used a slightly modified version of the classification of Naitoh et al, adding the trifid canal type. It was observed that the retromolar canal type was the most common (71.3%), followed by the dental canal type (18.8%), the trifid mandibular canal (5.8%), and the forward type (4.1%). Not even one case of the buccolingual canal type was observed. Although the result by Kang et al20 was not the same as ours, it was consistent that the retromolar canal type was the most common in the Korean population. One important finding in our study was the observation of a relatively high prevalence rate of the trifid mandibular canal. To the best of our knowledge, only four cases of the trifid mandibular canal have been reported.6,18 In this study, seven cases of the trifid mandibular canal were observed, and they were classified into five subtypes: A. two accessory canals of the retromolar type, B. two accessory canals of one retromolar and one dental type, C. two accessory canals of the dental type, D. two accessory canals of one dental and one forward type, and E. two accessory canals of the retromolar type with two mandibular foramina. Subtype A was observed in two cases, subtype B in one case, subtype C in one case, subtype D in two cases, and subtype E in one case. Interestingly, two mandibular foramina were observed in the subtype E case, and two accessory canals of the retromolar canal type were divided from the accessory foramina.
The classification of the bifid mandibular canal, particularly of the retromolar and dental canal type, may be clinically important.1 When the retromolar region is used as a donor site for harvesting a bone block, the identification of the retromolar canal is important for a safe harvest. Further, identification of the dental canal may be important in the extraction and the root canal treatment of the teeth.1
In addition, the detection of bifid and trifid canals may have some other important clinical implications such as inadequate anesthesia, complications after mandibular osteotomy or implant placement, pain, and discomfort due to the additional pressure of the mandibular prosthesis.6,8,16,18
Some studies have included a morphometric analysis of the bifid mandibular canal and have considered the differences in factors such as length, angles, and diameter according to the canal type.1,15,16,17,19 Orhan et al16 reported that the mean length of the bifid mandibular canal was 13.6 mm on the right side and 14.1 mm on the left side. The mean superior angle between the main canal and the superior wall of the bifid mandibular canal was 139° on the right side and 141° on the left side, whereas the mean inferior angle between the main canal and the inferior wall was 38° on the right side and 32° on the left side. Naitoh et al1 reported 9.6 mm for forward canals, 14.8 mm for retromolar canals, 8.9 mm for dental canals, and 1.6 mm for buccolingual canals. Fu et al19 reported that the canal was 10.1 mm in length and 0.9 mm in width. The present study showed that the mean length of the bifid mandibular canal was 16.9 mm and that this value was longer than that reported in the previous literature. As for the angles of the bifid mandibular canal, the mean superior angle was 149.2° and the mean inferior angle was 37.7°, which was similar to the result obtained by Orhan et al.16 The diameters of the bifid mandibular canal were reported using the following two categories: greater than 50% of the main canal and less than 50% of the main canal.15,17 The mean diameter of the bifid canal was 1.27-1.68 mm and that of the main canal was 2.85-3.28 mm.15,20 Further, bifid canals greater than 50% of the main canal and less than 50% of the main canal appeared at an almost equal ratio.15 In this study, the mean diameter of the bifid canal was 2.2 mm and that of the main canal was 4.3 mm, which was slightly larger than the results obtained by others. Further, the diameter of the bifid canal appeared to be nearly half of that of the main canal. The slightly larger diameter of the bifid and the main canals was attributed to the fact that the canal diameters were measured on a cross-sectional image oblique to the long axis of the bifid and the main mandibular canals, particularly in the mandibular ramus region. Previous studies have not described how to measure the diameter of the canal precisely.
In summary, this study shows that the bifid and trifid mandibular canals in the Korean population have a relatively high prevalence rate through a CBCT evaluation and that the retromolar canal is the most common type of mandibular canal in this population. CBCT is suggested for a detailed evaluation of the bifid and trifid mandibular canals before mandibular surgery.
Figures and Tables
Fig. 4
CBCT image shows canal type 5A (trifid canal type: two accessory canals of the retromolar canal type).
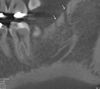
Fig. 5
CBCT images show canal type 5B (trifid canal type: two accessory canals of one retromolar (A) and one dental canal (B) type).

Fig. 6
CBCT image shows canal type 5C (trifid canal type: two accessory canals of the dental canal type).
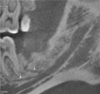
Fig. 7
CBCT image shows canal type 5D (trifid canal type: two accessory canals of one dental and one forward canal type).
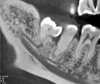
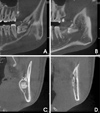
Fig. 8
CBCT images show canal type 5E (trifid canal type: two accessory canals of the retromolar canal type (A-C) with two mandibular foramina (D)).
References
1. Naitoh M, Hiraiwa Y, Aimiya H, Ariji E. Observation of bifid mandibular canal using cone-beam computerized tomography. Int J Oral Maxillofac Implants. 2009; 24:155–159.
2. Langlais RP, Broadus R, Glass BJ. Bifid mandibular canals in panoramic radiographs. J Am Dent Assoc. 1985; 110:923–926.

3. Carter RB, Keen EN. The intra mandibular course of the inferior alveolar nerve. J Anat. 1971; 108:433–440.
4. Nortjé CJ, Farman AG, Grotepass FW. Variations in the normal anatomy of the inferior dental (mandibular) canal: a retrospective study of panoramic radiographs from 3612 routine dental patients. Br J Oral Surg. 1977; 15:55–63.

5. Bogdán S, Pataky L, Barabás J, Németh Z, Huszár T, Szabò G. Atypical courses of the mandibular canal: comparative examination of dry mandibles and x-rays. J Craniofac Surg. 2006; 17:487–491.
6. Auluck A, Pai KM, Mupparapu M. Multiple mandibular nerve canals: radiographic observations and clinical relevance. Report of 6 cases. Quintessence Int. 2007; 38:781–787.
7. Wadhwani P, Mathur RM, Kohli M, Sahu R. Mandibular canal variant: a case report. J Oral Pathol Med. 2008; 37:122–124.

8. Grover PS, Lorton L. Bifid mandibular nerve as a possible cause of inadequate anesthesia in the mandible. J Oral Maxillofac Surg. 1983; 41:177–179.

9. Juodzbalys G, Wang HL, Sabalys G. Anatomy of mandibular vital structures. Part 1: mandibular canal and inferior alveolar neurovascular bundle in relation with dental implantology. J Oral Maxillofac Res. 2010; 1:e2.

10. Claeys V, Wackens G. Bifid mandibular canal: literature review and case report. Dentomaxillofac Radiol. 2005; 34:55–58.

11. Naitoh M, Hiraiwa Y, Aimiya H, Gotoh M, Ariji Y, Izumi M, et al. Bifid mandibular canal in Japanese. Implant Dent. 2007; 16:24–32.

12. Rouas P, Nancy J, Bar D. Identification of double mandibular canals: literature review and three case reports with CT scans and cone beam CT. Dentomaxillofac Radiol. 2007; 36:34–38.

13. Lee JS, Yoon SJ, Kang BC. Mandibular canal branches supplying the mandibular third molar observed on cone beam computed tomographic images: reports of four cases. Korean J Oral Maxillofac Radiol. 2009; 39:209–212.
14. Lee HW, Kim YG, Lee BS, Kwon YD, Choi BJ, Kim YR. Bifid mandibular canal: radiographic observation and clinical relevance - a case report. J Korean Dent Soc Anesthesiol. 2009; 9:24–29.
15. Kuribayashi A, Watanabe H, Imaizumi A, Tantanapornkul W, Katakami K, Kurabayashi T. Bifid mandibular canals: cone beam computed tomography evaluation. Dentomaxillofac Radiol. 2010; 39:235–239.

16. Orhan K, Aksoy S, Bilecenoglu B, Sakul BU, Paksoy CS. Evaluation of bifid mandibular canals with cone-beam computed tomography in a Turkish adult population: a retrospective study. Surg Radiol Anat. 2011; 33:501–507.

17. de Oliveira-Santos C, Souza PH, de Azambuja Berti-Couto S, Stinkens L, Moyaert K, Rubira-Bullen IR, et al. Assessment of variations of the mandibular canal through cone beam computed tomography. Clin Oral Investig. 2012; 16:387–393.

18. Mizbah K, Gerlach N, Maal TJ, Bergé SJ, Meijer GJ. The clinical relevance of bifid and trifid mandibular canals. Oral Maxillofac Surg. 2012; 16:147–151.

19. Fu E, Peng M, Chiang CY, Tu HP, Lin YS, Shen EC. Bifid mandibular canals and the factors associated with their presence: a medical computed tomography evaluation in a Taiwanese population. Clin Oral Implants Res. 2014; 25:e64–e67.





 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download