Abstract
Purpose
This study was performed to determine the efficacy of observers' prediction for the need of bone grafting and presence of perioperative complications on the basis of cone-beam computed tomography (CBCT) and panoramic radiographic (PAN) planning as compared to the surgical outcome.
Materials and Methods
One hundred and eight partially edentulous patients with a need for implant rehabilitation were referred for preoperative imaging. Imaging consisted of PAN and CBCT images. Four observers carried out implant planning using PAN image datasets, and at least one month later, using CBCT image datasets. Based on their own planning, the observers assessed the need for bone graft augmentation as well as complication prediction. The implant length and diameter, the need for bone graft augmentation, and the occurrence of anatomical complications during planning and implant placement were statistically compared.
Results
In the 108 patients, 365 implants were installed. Receiver operating characteristic analyses of both PAN and CBCT preoperative planning showed that CBCT performed better than PAN-based planning with respect to the need for bone graft augmentation and perioperative complications. The sensitivity and the specificity of CBCT for implant complications were 96.5% and 90.5%, respectively, and for bone graft augmentation, they were 95.2% and 96.3%, respectively. Significant differences were found between PAN-based planning and the surgery of posterior implant lengths.
Continuous advances in the field of implant dentistry have provided clinicians with various treatment options to facilitate the placement of dental implants in patients with deficiencies in bone volume in the posterior maxillae. Nowadays, one of the most common and predictable ways to compensate for inadequate vertical bone height is to elevate the sinus floor.1,2 Most of the time, this is done in combination with bone grafts and bone substitutes.3
Appropriate case selection requires a thorough (clinical and radiographic) examination. Further, the European Association for Osseointegration (EAO) reported on the current recommendations on radiographic diagnostic considerations in implant dentistry.4 They recommended cross-sectional imaging in clinical borderline situations where there appears to be limited bone height and/or bone width available for successful implant treatment. Intraoral and panoramic radiography (PAN) do not shed light on the orofacial bone width, and a majority of the proposed implant sites cannot be properly evaluated on this basis alone. These diagnostic errors can have significant clinical consequences.5,6,7 Implant surgery complications are not uncommon and should be anticipated during the planning phase to allow for predictable surgery.8,9,10
The overall goal of the present study was to compare the treatment planning using PAN or cone-beam computed tomography (CBCT) images with the surgical gold standard when performing the surgery.
This study was approved by the Institutional Ethical Review Boards of the KULeuven, Leuven (Belgium) under the number B32220083749 and the San Martin de Porres University, Lima (Peru) (protocol #012/2009). It was conducted from July 2009 to June 2010. Informed consent was obtained from patients to use their anonymized X-ray images and photographs. Consent for involvement in the study had no further implications on their treatment.
The patients were treated following the principles embodied in the World Medical Association Helsinki Declaration of 1975 for biomedical research involving human subjects, as revised in 2000.
The patients' inclusion criteria were as follows: at least 18 years of age, absence of general medical contraindications for oral surgery procedures (American Society of Anesthesiologists ASA-1 or ASA-2), full-mouth bleeding score and full-mouth plaque score of less than 25% at baseline, partial edentulism referred for one or more implants and with the intention of providing rehabilitation by means of implant-supported prostheses, absence of ongoing infection at the intended implant site or sinus pathologies for those scheduled for maxillary sinus augmentation, and ability to sign the informed consent form. Patients were excluded if they presented one or more of the following exclusion criteria: any systemic disease, condition, pathology, or medication that might compromise healing or implant osseointegration.
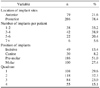
A total of 108 patients fulfilled the abovementioned inclusion criteria (59% males, 41% females, mean age: 55 years, range: 23-57 years) of which 20 had intraoral radiographs and 88 had panoramic radiographs taken.
Patients were included if both PAN images and CBCT images had been taken with a maximum interval of four months and if the presurgical planning phase was followed by implant placement. For PAN radiography, an Orthopantomograph® OP-100D (Instrumentarium Corp., Tuusula, Finland) was used. The unit used a charge-coupled device and was operated at 70 kV and 8 mA.
In order to make meaningful measurements from the PAN images, the magnification factors of the PAN unit were measured using an object of known dimensions. Prior to full implementation of the study, a pilot study was conducted to evaluate the magnification factor. Six reference balls having a diameter of 5 mm were fixed by a piece of wax in the maxillary and mandibular anterior, premolar, and molar regions of partially edentulous patients. The panoramic imaging unit reported a mean calculated magnification factor of 1.27±0.02 (range: 1.23-1.31).
All CBCT images were acquired using i-CAT® (Imaging Sciences International Inc., Hatfield, PA, USA), operating at 120 kVp and 8 mA, an exposure time of 26.9 s, and a voxel size of 0.2 mm. A list with the codes and the corresponding names was created and saved in an encrypted file so that patient confidentiality was protected and yet, the data were retrievable if needed.
Five experienced implant surgeons evaluated the intraoral radiographs, PAN, CBCT examinations, and intraoral photographs on two occasions under standardized conditions (e.g., those related to the room, dimmed light, monitor, and image size). In the first session, the surgeons evaluated only conventional images. The second session was based on conventional images and CBCT images. The viewings were separated by a four-week interval to avoid case memory. The order of images was randomized per session, as was the order of sessions for each rater.
For visualizing the CBCT images, the i-CATVision™ (Imaging Sciences International, Inc., Hatfield, PA, USA) software was used to visualize the cases. The slice thickness was 0.25 mm. The direct volume rendering screen and three-dimensional (3D) modality were used to scroll through the axial, sagittal, and coronal planes. Two training sessions were organized prior to the final observations for the calibration of the observers. For observing the panoramic images, the Digora® for Windows 2.7 software (Digora, Soredex, Tuusula, Finland) was used for implant planning. The values were corrected for the respective magnification factor of the panoramic X-ray unit. The images were viewed on a Dell Precision® Display (1920×1200 pixels) (Dell Inc., Round Rock, TX, USA) in a dimmed room at a distance of 60 cm from the diagnostic viewing screen.
For each patient, each practitioner had to select an implant for each prospective implant site. The choice of implants was restricted to the implants available in the Renova® and Prima Connex® implants library (Keystone Dental, Burlington, MA, USA). In the selection of implants, the observers were required to use a safety margin of 1.5 mm below the maxillary sinus or nasal floor and above the mandibular canal.
Based on their own planning, the observers needed to answer three categories of questions: 1) implant characteristics, 2) bone graft augmentation, and 3) expected complications. The implant length and diameter were the two implant characteristics studied. Considering bone graft augmentation, some bone substitutes were an alternative to the autogenous bone. Of the different available surgical techniques, onlay grafting, inlay grafting, ridge expansion, sinus floor augmentation using the crestal approach (osteotome technique), and maxillary sinus elevation using the lateral approach with implants placed simultaneously or in a second surgical phase, were included.
As a grafting material, the autogenous bone from the retromolar-ramus or the maxillary tuberosity area was used together with the anorganic bovine bone (Bios-Oss®, Geistlich Pharma AG, Wolhusen, Switzerland) covered with a collagen membrane (Bio-Gide®, Geistlich Pharma AG, Wolhusen, Switzerland). The implant systems used in the present study were Prima Connex® and Renova®. The proposed implant site was prepared according to the manufacturer's recommendation, and the implant with the desired length was placed. All surgical procedures were performed by an experienced periodontologist with more than 10 years of experience in implant dentistry.
For each patient, the following postoperative complications were measured intra-surgically and one week postoperatively: Schneiderian membrane perforation, wrong angulation, fenestration, dehiscence, sensory disturbance, and infection.
Observations of a small or medium (ø: <10 mm) Schneiderian membrane perforation were recorded. Wrong angulations were assessed in the mesiodistal, corono-apical, and orofacial view using photography. Fenestrations were measured from the coronal to the apical margin of the implant exposure, and dehiscence was assessed by measuring the height (in millimeters) of the bone defects at the mid-buccal or the lingual aspects of the exposed part of the implants by using a 1-mm marked periodontal probe and photography. The neurosensory functions of the chin and the lip were assessed according to a previously described methodology for clinical neurological testing.11 Finally, infection was recorded when patients had severe pain, pus, swelling, and inflammation.
The CBCT and PAN accuracy in estimating implant characteristics, the required bone graft augmentation in a deficient crest, and the expected complications were evaluated using the postoperative data as reference.
All statistical analyses were performed using STATA v12 for Windows (StataCorp LP, College Station, TX, USA). Differences in the implant length and diameter between CBCT and PAN planning were compared using the Kruskal-Wallis non-parametric analysis of variance (ANOVA), assuming that the samples did not follow a normal distribution. When assessing the overall bone graft augmentation and the expected complications during surgery with the preoperative planning on different modalities and observers, the z test for the difference in proportions was calculated. The statistical significance was set at p<0.05 for all the tests.
To compare the agreement among the four observers on PAN versus CBCT, Kappa coefficients were selected.12 Kappa coefficients were evaluated according to the following criteria: <0, no agreement; 0.0-0.20, slight agreement; 0.21-0.40, fair agreement; 0.41-0.60, moderate agreement; 0.61-0.80, substantial agreement; and 0.81-1.00, almost perfect agreement.
The receiver operating characteristic (ROC) curve was generated to graphically present the interaction between sensitivity and specificity. The overall test performance was quantified using the area under the ROC curve. The area under the curve (AUC) measures the overall capacity of the test to discriminate between participants with the disease and those without it. An AUC of 0.5 indicates a poor discriminative ability; 0.75-0.92 is good, 0.93-0.97 is very good, and an area of 1.0 indicates a perfect test.13
The number of patients observed and scored was 108. The specialists placed a total of 365 implants. A majority of the patients had 3 to 4 implants (38.9%), more frequently located on the molar and premolar positions (Table 1).
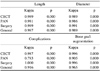
Significant differences were found for the implant length in the posterior position between PAN surgery (p<0.01) for the four observers. Considering the implant diameter on the posterior positions, the four observers reported significant differences between the two modalities when compared to the surgery (Table 2).
There were significant differences between CBCT planning and surgery (p=0.001) with 28% of the implant complications planned on CBCT, while in the case of surgery, this percentage reduced to 18%.
Regarding the presence of fenestrations, the percentages of modalities of PAN(1%) did not differ from that of surgery (2%); however, CBCT planning had a significantly higher percentage (5%) (p=0.00) than surgery. Observers 2 and 4 obtained similar results (p=0.00).
The four observers reported no differences in the prediction of dehiscence on the modalities planning with respect to the surgery. Only observers 2 and 4 found differences between intraoral planning and surgery (p=0.04).
No subjects had an immediate or permanent postoperative inferior alveolar nerve (IAN) paresthesia or anesthesia.
CBCT bone graft augmentation planning was very similar and did not differ statistically (p=0.71) from the gold standard; 52% of the implants needed this procedure during surgery, whereas in the case of CBCT planning, the percentage was 53% (Table 3).
When measuring the degree of agreement among the four observers, we found an overall agreement rate higher than 0.9 (almost perfect agreement) in terms of the length, diameter, complications, and the need for bone graft augmentation. In all cases, the degree of agreement was significant (p<0.01) (Table 4).
The ROC curve (Fig. 1) showed that CBCT had a greater ability to detect true positives for planning complications and the need for bone graft augmentation with the highest sensitivity of 96.5% and an AUC of 0.94. This technique was very similar to the surgical gold standard. A different situation occurred with complications planned on PAN, where this technique could not be recommended as a diagnostic test due to the inclusion of 0.5 on the 95% confidence interval (CI) (0.499-0.551) and an AUC of 0.52. However, for bone graft augmentation, the 95% CI was 0.571-0.621 with an AUC of 0.6, which was inferior to that found with CBCT (0.93) (95% CI: 0.931-0.957).
Several authors have suggested that preoperative radiological investigations can be very important for facilitating an understanding of the anatomy.14,15 According to Apostolakis and Brown,16 CBCT is necessary to accurately and reliably depict the anterior loop, which was measured to have a length of up to 5.7 mm. A safe distance of at least 6 mm from the anterior border of the mental foramen was suggested. In most of the partially edentulous patients included in our study, the implants were planned in the posterior area; this can explain the lack of neurosensory disturbances in the area of the lower lip and the chin.
Furthermore, the path of the IAN was clearly seen with CBCT, preventing the perforation of the IAN in five cases. Two-dimensional (2D) imaging offers a good overview of the maxillary-mandibular complex but cannot determine the spatial position of the IAN. If careful depth control is based on faulty information, perforation of the IAN can lead to permanent paresthesia. In a recent study, Schropp et al17 showed that the selected implant size differed considerably when planned on panoramic or cross-sectional tomography. On the basis of our results, we concluded that care should be taken when using PAN-intraoral-based preoperative planning of implants with a predisposition to select longer implants in a posterior position and therefore, a more risky location. A previous study comparing implant planning using panoramic versus CBCT images, found similar results.18 Similarly, Renton et al19 found that most of the cases of the permanent neuropathy of the IAN was associated with PAN preoperative imaging with the highest incidence of idiopathic trigeminal neuropathy observed in patients who had received presurgical 2D radiographs (90%), while with CBCT, only 10% of the cases presented this condition.
From the findings of this study, there are several considerations related to perioperative complications and bone graft augmentation. The 3D data from CBCT scans can be extremely revealing. Temmerman et al20 reported an intraosseous canal in the lateral sinus wall visible in 50% of the analyzed CT images. A presurgical CT evaluation of the course of this bony vessel and other anatomic important structures is recommended when performing a maxillary sinus augmentation procedure in order to prevent intense bleeding during osteotomy.6,21 In our study, CBCT allowed the visualization of an intraosseous artery and help localizing this structure during surgery (Fig. 2).
Perforation of the Schneiderian membrane is the main intraoperative complication and occurs in 11%-56% of the procedures according to a review of the literature.22 In this study, only 14% of the membrane perforations were seen during surgery. In addition, the angle of the buccolingual maxillary sinus wall has been proposed as a factor to determine the likelihood of sinus perforation.23 They reported that the narrower the angle between the medial and the lateral walls was, the higher was the membrane perforation rate. Sinuses with interwall angles of <30° had a perforation rate of 37.5%, compared with 0% for those with angles of >60°.
The normal anatomy in the esthetic region presents challenges during implant placement because of the high risks of buccal plate resorption, dehiscence, and fenestration, which could jeopardize the esthetics and function of the implants. Correct 3D positioning of implants is important for a successful outcome, particularly in the aesthetic region where the buccal plate is very thin. Braut et al24 reported that CBCT measurements of the facial bone wall for teeth in the anterior maxilla were rarely greater than 1mm, only in approximately 10% of the teeth. Less bone was presented in central incisors (4%-8%) and most in the first premolars (more than 25%). For orofacial positioning, implants should be placed 1.0-1.5 mm more to the palatal aspect inside the alveolar housing; this allows increased thickness of the facial bone wall for soft-tissue support. Recently, Chang et al25 reported an incidence of fenestrations of approximately 20% in implants placed in the cingulum position with the axis following that of its restoration. They concluded that fenestrations could be avoided by a minor correction (<10°) of implant angulation. The virtual planning on CBCT imaging revealed possible implants perforating the facial plate of the bone. This helped to prevent implant malpositions in 6% of the patients. In our study, CBCT availability allowed a better visualization of the bone defects.
Problems associated with 2D imaging modalities are well documented in the literature and can include overlapping of adjacent structures, poor spatial resolution, and lack of bone width information. This can lead to complications of an inaccurate diagnosis of implant sites and areas that require bone grafting, resulting in unfavorable outcomes. In our study, this is clearly seen in the form of the 95.2% sensitivity from bone grafting planning based on CBCT examinations. In contrast, PAN and intraoral imaging only allowed a sensitivity of 38.2% and 26.6% for this issue, respectively. The assessment of the potential dental implant diameters on anterior sites for the placement of standard or narrow-diameter implants was planned more accurately with CBCT. However, from the viewpoint of the implant diameter on a posterior location, significant differences were found for the three modalities when compared with the surgical standard. This can be explained due to the possibility of performing regenerative techniques on the posterior area and a subsequent change during surgical strategy.
The surgeon in the present study established the implant placement on the basis of the complete patient file (CBCT and PAN) findings, and the observers' implant planning was therefore based on the CBCT and PAN analysis. It is not possible to speculate on the number of postoperative complications that might have occurred if the treatment had been performed according to the first treatment plan, which was based on PAN, a method that is less dose- and work-demanding than CBCT. These authors emphasized that the need for CBCT in implant treatment planning is still to be justified in randomized controlled trials. However, in our opinion, it is not ethically acceptable to conduct prospective clinical trials when one part of the study could well be disadvantaged in terms of the treatment received. Moreover, most of the interesting outcomes ("success" of implant treatment) require years of follow-up. In this context, we planned a "scenario-based" study with implant surgeons to see whether CBCT alters treatment plans. Another study design, wherein the surgeon chooses his treatments only on the basis of clinical assessments, would have been a meaningful comparison of the efficacy of CBCT and conventional imaging. However, this is not clinically and ethically possible.
When oral implants are planned in the atrophic posterior maxilla, bone height is a diagnostic factor of primary importance. Conventional radiography may not be able to assess the true 3D anatomical presentation. CBCT observer-based planning gives more homogeneity of treatment plans as compared to the surgical gold standard. Further, complications were predicted better when the planning was based on CBCT images.
Figures and Tables
 | Fig. 1Receiver operating characteristic (ROC) analysis reveals an excellent diagnostic accuracy of CBCT for the planning of complications and the diagnosis of bone graft augmentation with an area under the curve (AUC) of 0.94. |
 | Fig. 2A. CBCT shows the posterior superior alveolar artery before creating a lateral window into the maxillary sinus. B. The artery is seen during the sinus lift procedure located at 15 mm from the alveolar crest as diagnosed with CBCT. |
References
1. Del Fabbro M, Rosano G, Taschieri S. Implant survival rates after maxillary sinus augmentation. Eur J Oral Sci. 2008; 116:497–506.

2. Emmerich D, Att W, Stappert C. Sinus floor elevation using osteotomes: a systematic review and meta-analysis. J Periodontol. 2005; 76:1237–1251.

3. Pjetursson BE, Tan WC, Zwahlen M, Lang NP. A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevation. J Clin Periodontol. 2008; 35:216–240.

4. Harris D, Horner K, Gröndahl K, Jacobs R, Helmrot E, Benic GI, et al. E.A.O. guidelines for the use of diagnostic imaging in implant dentistry 2011. A consensus workshop organized by the European Association for Osseointegration at the Medical University of Warsaw. Clin Oral Implants Res. 2012; 23:1243–1253.

5. Ella B, Sédarat C, Noble Rda C, Normand E, Lauverjat Y, Siberchicot F, et al. Vascular connections of the lateral wall of the sinus: surgical effect in sinus augmentation. Int J Oral Maxillofac Implants. 2008; 23:1047–1052.
6. Flanagan D. Arterial supply of maxillary sinus and potential for bleeding complication during lateral approach sinus elevation. Implant Dent. 2005; 14:336–338.

7. Kalpidis CD, Setayesh RM. Hemorrhaging associated with endosseous implant placement in the anterior mandible: a review of the literature. J Periodontol. 2004; 75:631–645.

8. Greenstein G, Cavallaro J, Romanos G, Tarnow D. Clinical recommendations for avoiding and managing surgical complications associated with implant dentistry: a review. J Periodontol. 2008; 79:1317–1329.

9. Misch K, Wang HL. Implant surgery complications: etiology and treatment. Implant Dent. 2008; 17:159–168.

10. Jacobs R, Quirynen M, Bornstein M. Neurovascular disturbances after implant surgery. Periodontol 2000. 2014; 66:188–202.

11. Guerrero ME, Botetano R, Beltran J, Horner K, Jacobs R. Can preoperative imaging help to predict postoperative outcome after wisdom tooth removal? A randomized controlled trial using panoramic radiography versus cone-beam CT. Clin Oral Investig. 2014; 18:335–342.

12. Fleiss JL. Statistical methods for rates and proportions. 2nd ed. New York: Wiley-Interscience;1981. p. 229–232.
13. Egger M, Smith GD, Altman DG. Systematic reviews in health care: meta-analysis in context. 2nd ed. London: BMJ;2001. p. 248–282.
14. Timmenga NM, Raghoebar GM, Liem RS, van Weissenbruch R, Manson WL, Vissink A. Effects of maxillary sinus floor elevation surgery on maxillary sinus physiology. Eur J Oral Sci. 2003; 111:189–197.

15. van den Bergh JP, ten Bruggenkate CM, Disch FJ, Tuinzing DB. Anatomical aspects of sinus floor elevations. Clin Oral Implants Res. 2000; 11:256–265.

16. Apostolakis D, Brown JE. The anterior loop of the inferior alveolar nerve: prevalence, measurement of its length and a recommendation for interforaminal implant installation based on cone beam CT imaging. Clin Oral Implants Res. 2012; 23:1022–1030.

17. Schropp L, Stavropoulos A, Gotfredsen E, Wenzel A. Comparison of panoramic and conventional cross-sectional tomography for preoperative selection of implant size. Clin Oral Implants Res. 2011; 22:424–429.

18. Guerrero ME, Noriega J, Castro C, Jacobs R. Does cone-beam CT alter treatment plans? Comparison of preoperative implant planning using panoramic versus cone-beam CT images. Imaging Sci Dent. 2014; 44:121–128.

19. Renton T, Dawood A, Shah A, Searson L, Yilmaz Z. Post-implant neuropathy of the trigeminal nerve. A case series. Br Dent J. 2012; 212:E17.

20. Temmerman A, Hertelé S, Teughels W, Dekeyser C, Jacobs R, Quirynen M. Are panoramic images reliable in planning sinus augmentation procedures? Clin Oral Implants Res. 2011; 22:189–194.

21. Marx RE, Garg AK. A novel aid to elevation of the sinus membrane for the sinus lift procedure. Implant Dent. 2002; 11:268–271.

22. Testori T, Wallace SS, Del Fabbro M, Taschieri S, Trisi P, Capelli M, et al. Repair of large sinus membrane perforations using stabilized collagen barrier membranes: surgical techniques with histologic and radiographic evidence of success. Int J Periodontics Restorative Dent. 2008; 28:9–17.
23. Cho SC, Wallace SS, Froum SJ, Tarnow DP. Influence of anatomy on Schneiderian membrane perforations during sinus elevation surgery: three-dimensional analysis. Pract Proced Aesthet Dent. 2001; 13:160–163.
24. Braut V, Bornstein MM, Belser U, Buser D. Thickness of the anterior maxillary facial bone wall - a retrospective radiographic study using cone beam computed tomography. Int J Periodontics Restorative Dent. 2011; 31:125–131.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download