This article has been corrected. See "Erratum to: Conversion coefficients for the estimation of effective dose in cone-beam CT" in Volume 44 on page 255.
Abstract
Purpose
To determine the conversion coefficients (CCs) from the dose-area product (DAP) value to effective dose in cone-beam CT.
Materials and Methods
A CBCT scanner with four fields of view (FOV) was used. Using two exposure settings of the adult standard and low dose exposure, DAP values were measured with a DAP meter in C mode (200mm×179 mm), P mode (154 mm×154 mm), I mode (102 mm×102 mm), and D mode (51 mm×51 mm). The effective doses were also investigated at each mode using an adult male head and neck phantom and thermoluminescent chips. Linear regressive analysis of the DAP and effective dose values was used to calculate the CCs for each CBCT examination.
Results
For the C mode, the P mode at the maxilla, and the P mode at the mandible, the CCs were 0.049 µSv/mGycm2, 0.067 µSv/mGycm2, and 0.064 µSv/mGycm2, respectively. For the I mode, the CCs at the maxilla and mandible were 0.076 µSv/mGycm2 and 0.095 µSv/mGycm2, respectively. For the D mode at the maxillary incisors, molars, and mandibular molars, the CCs were 0.038 µSv/mGycm2, 0.041 µSv/mGycm2, and 0.146 µSv/mGycm2, respectively.
Cone-beam computed tomography (CBCT) which provides three-dimensional (3D) images, was developed for the dental use in the late 1990s.1 The advantages of CBCT include a lower entrance dose, higher resolution, and lower cost than conventional computed tomography (CT). Moreover, CBCT provides 3D information via multiplanar and 3D reconstructed images. For this reason, its use in dental practice has rapidly increased and is commonly used in preoperative implant planning, the localization of impacted teeth, the diagnostic and surgical planning of oral and maxillofacial radiology, the evaluation of periodontal and periapical lesions, endodontic problems, and orthodontic treatment planning.2,3,4,5 Although the dose of CBCT is lower than that of conventional CT, it is higher than that of conventional radiography mainly used in dental practice. There have been numerous studies about effective doses of CBCT using thermoluminescent dosemeter (TLD) chips.6,7,8,9,10,11,12 However, this estimation method using TLD chips is laborious and time-consuming.
The establishment of diagnostic reference levels in medical imaging was recommended by the International Commission on Radiation Protection (ICRP) to promote the optimization of patient radiation exposure.13 In Korea, diagnostic reference levels for diagnostic radiology including dental radiographic procedures were reported by the Korea Food and Drug Administration.14,15,16,17 Since the entrance surface dose (ESD) and dose-area product (DAP) are well-defined and easy-to-use methods, they have been frequently used as the adequate dose quantities for DRLs.18,19 Especially, DAP was recommended as a dose quantity for CBCT by Health Protection Agency (HPA) in the United Kingdom.20 Lofthag-Hansen et al21 compared two methods of the CT dose index (CTDI) and DAP to calculate the effective dose of CBCT examination, and they proposed that the DAP measurement was the appropriate method to determine the effective dose. In addition, they commented that the conversion factors should be determined according to the dental regions and radiographic techniques.21
In diagnostic medical radiology, the conversion factors from DAP to effective dose have been suggested by a number of authors.22,23,24 There has been a very few reports about those in dental radiology. Looe et al25,26 suggested the conversion coefficients for the estimation of effective dose of the intraoral, panoramic, and lateral cephalometric radiography. However, the conversion coefficient for CBCT remains unknown.
The objectives of this study were to measure the DAP and effective dose in one CBCT device and to determine the conversion coefficients from the DAP value to effective dose.
The Alphard VEGA (Asahi Roentgen Ind. Co., Kyoto, Japan) CBCT scanner, which has four fields of view (FOVs) including the C mode (200 mm×179 mm), P mode (154 mm×154 mm), I mode (102 mm×102 mm), and D mode (51mm×51 mm), was used in this study.
The DAP was measured using the DIAMENTOR M4-KDK (PTW, Freiburg, Germany) (Fig. 1). In addition, the effective dose was measured using TLD-100 LiF chips (1.8×1.8×0.035 inch; Harshaw Chemical Co., Solon, OH, USA) in an adult male Alderson Radiation Therapy phantom of the head and neck (Radiology Support Devices, Inc., Long Beach, CA, USA) (Fig. 2).
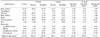
An ionization chamber of DAP meter was located on the tube side of the CBCT scanner (Fig. 3). The DAP value was measured with two different exposure settings (the standard adult and low-dose exposure setting) at the four FOVs. Table 1 shows the exposure parameters and specifications of the CBCT scanner used in this study. The tube voltage and exposure time were fixed at 80 kV for 17 seconds. The tube current, the only exposure parameter selectable by the operator, was set at 6 mA for the adult exposure and 4 mA for the low dose exposure in C mode, 9 mA and 5 mA in P mode, 8 mA and 4 mA in I mode, and 9 and 6 mA in D mode. For the calculation of the conversion coefficients, the child exposure setting was considered the low-dose exposure in this study. All measurements were repeated three times and averaged for both exposure settings. The measured values were corrected by correction factors considering the temperature and air pressure during the DAP measurement.
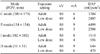
The TLD chips were calibrated and annealed by the Iljin Radiation Engineering Company (Hwaseong, Republic of Korea). Twenty-two TLD chips were inserted in the adult male phantom and CBCT examinations were performed using the two different exposure settings. The CBCT examinations were done in the C mode, P mode (maxilla and mandible), I mode (maxilla and mandible), and D mode (maxillary incisors, maxillary molars, and mandibular molars) (Fig. 4).
The effective dose was calculated using the method by Ludlow et al.27 The TLD chips were used to record the absorbed dose at 22 locations in the head and neck of the phantom (Table 2). One TLD chip was placed in the thyroid gland, four in the salivary gland, eight in the bone marrow, one in the esophagus, four in the skin, two in the brain, four in the eye. Two chips in the lenses of eye were used to measure the dose in the eyes and skin. Only TLD chips that were calibrated within a 5% error were used in this experiment. For each examination, background radiation was also measured using five TLD chips that were not exposed to radiation. The measured background radiation was subtracted from the measured dose of each irradiated TLD chip. The tissue-absorbed doses (in µGy) at each anatomical site were calculated from irradiated TLDs readout. The products of these values and the percentage of a tissue or organ irradiated in a radiographic examination (Table 3) were used to calculate the equivalent dose (HT) in µSv. Effective dose (E), expressed in µSv, was calculated using the equation: E=ΣWT×HT, where E is the product of tissue weighting factor (WT) and the equivalent dose (HT). Table 4 shows the 2007 ICRP tissue-weighting factors.28
The measured DAP value and effective dose was inserted into a linear regression model to calculate the conversion coefficients for each CBCT examination. The linear regression analysis was performed using the IBM SPSS software (version 19, IBM Corp., Somers, NY, USA).
The DAP values for each mode and exposure setting of CBCT used in this study are shown in Table 5. At the adult exposure level, the DAP values were 3704 mGycm2, 4499 mGycm2, 1910 mGycm2, and 644 mGycm2 in the C, P, I, and D modes, respectively.
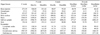
The equivalent and effective doses for each CBCT examination are shown in Tables 6,7,8,9. The effective doses in the adult exposure setting were 183.07 µSv in the C mode and 303.66 µSv and 288.48 µSv in the P mode for the maxilla and mandible, respectively. Additionally, the effective doses for the I mode in the maxilla and mandible were 145.85 µSv and 184.33 µSv, respectively. In the D mode, the effective doses were 22.34 µSv, 25.26 µSv, and 93.67 µSv for the maxillary incisors, maxillary molars, and mandibular molars, respectively.
The conversion coefficients for each of the eight different CBCT examinations are shown in Table 10. For the C mode, the P mode at the maxilla, and the P mode at the mandible, the conversion coefficients were 0.049 µSv/mGycm2, 0.067 µSv/mGycm2, and 0.064 µSv/mGycm2, respectively. For the I mode, the conversion coefficients at the maxilla and mandible were 0.076 µSv/mGycm2 and 0.095 µSv/mGycm2, respectively. For the D mode at the maxillary incisors, molars, and mandibular molars, the conversion coefficients were 0.038 µSv/mGycm2, 0.041 µSv/mGycm2, and 0.146 µSv/mGycm2, respectively.
Recently, investigation into the patient dose exposed during CBCT examination has been of increasing interest due to the profound dissemination of CBCT equipment in dental practice. This study showed that the DAP values of the Alphard VEGA CBCT examinations ranged from 644 mGycm2 to 4499 mGycm2, the effective doses from 22 µSv to 304 µSv at the adult standard exposure. The voxel sizes in the CBCT scanner were 0.39 mm, 0.3 mm, 0.2 mm, and 0.1 mm in the C, P, I, and D modes, respectively. In practice, each mode serves a specific purpose. The C mode (200mm×179 mm) is primarily used for orthodontic analysis; the P mode (154 mm×154 mm) for the evaluation of both impacted third molars or the diagnosis of lesions at the maxillofacial region; the I mode (102mm ×102 mm) for implant treatment planning involving more than three teeth or for the diagnosis of a jaw cyst; and the D mode (51 mm×51 mm) for implant treatment planning involving one or two teeth, one impacted tooth, the diagnosis of a small jaw cyst, or unilateral TMJ evaluation.
In descending order, the DAP values at the adult exposure setting were the highest in the P mode followed by the values in the C, I, and D mode. The differences among the DAP values tended to be proportional to the field size.21 However, the DAP value in the C mode, the largest FOV, was lower than that in the P mode in this study. This may be because the tube current for the C mode was two-thirds of that in the P mode. This result is in agreement with a previous study that observed an increasing DAP value at each mode as the tube current value increased.21
The Health Protection Agency of the United Kingdom proposed the use of the DAP as the dose quantity for the regular assessment of patient dose for dental CBCT.20,29 The Health Protection Agency Working Party on dental CBCT suggested that DRLs should be set for both adult and child radiography and the adult protocol should be that used for the placement of the upper first molar implant in a standard adult patient and the child measurement should be made using the clinical protocol used to image a single impacted maxillary canine in a 12 year old male.20 Given the wide range of DAP measurements recorded for different CBCT models, it was not considered appropriate to derive a National Reference Doses based on the third quartile DAP measurement of a dose survey as this would be little benefit for dose optimization.20 Instead they presented the achievable dose, which was based on the third quartile DAP value of a dose survey, where the X-ray field size had been normalized to an appropriate size to adequately image the two views proposed above, 4 cm diameter × 4 cm height cylindrical volume. 20 And an achievable dose of 250 mGycm2 was proposed for the adult procedure based on data by 41 CBCT units.20 The adjusted DAP value at D mode normalized to an area of 16 cm2 was 396 mGycm2. Since this value was higher than the achievable dose suggested by the Health Protection Agency, it was required to investigate methods to reduce patient dose in the CBCT device used in this study.
The effective doses are different according to the irradiated organs and areas of the body, despite being exposed by radiation with the same DAP value. The effective doses were calculated to determine the conversion coefficients at each mode of different sites. The effective doses at the adult exposure setting ranged from 22 µSv to 304 µSv across all CBCT examinations. These values were similar to those of Pauwels et al9 who reported that the effective doses from 14 CBCT devices ranged from 19 µSv to 368 µSv. In this study, the effective dose for the P mode at the maxilla was the highest. This might be due to the high tube current and large FOV in the P mode as well as the involvement of the radiosensitive salivary glands at the maxilla. In the D mode, a high variation from 22 µSv to 94 µSv was found according to the irradiated regions, and the effective dose at the maxillary incisors was lowest, but that of the mandibular molars was the highest. The high irradiation among these radiosensitive salivary glands may have influenced these results.
Previous studies about the conversion coefficients for other imaging modalities in dental radiology reported 0.009-0.108 µSv/mGycm2 for intraoral periapical radiography,25 0.087-0.131 µSv/mGycm2 for panoramic radiography,25 and 0.056-0.077 µSv/mGycm2 for lateral cephalometric radiography (ICRP 2006, draft).26 In this study, ICRP 103 tissue weighting factors were used to calculate the effective doses. In the D mode, the conversion coefficient for the maxillary incisors was the lowest and that for the mandibular molars was the highest. These results were similar to those from the intraoral periapical radiographic study,25 which showed the lowest conversion factors for maxillary incisor and highest for mandibular molar.25 In addition, the conversion coefficients tended to be dependent on tube voltage.25,26 However, we did not investigate the effect of tube voltage on the conversion coefficient because the CBCT scanner used in this study had a fixed tube voltage. Further research using a CBCT scanner with an adjustable tube voltage is needed.
In summary, the present study demonstrates the conversion coefficients in one CBCT device with fixed 80kV ranged from 0.038 µSv/mGycm2 to 0.146 µSv/mGycm2 according to the imaging modes and irradiated region and were highest for the D mode at the mandibular molar.
Figures and Tables
Fig. 2
Adult male ART head and neck phantom (A) and TLD-100 LiF chips (B) used for the measurement of effective dose.

Fig. 3
Ionization chamber of DAP meter is located at the tube side of CBCT machine for the measurement of DAP.

Table 3
Estimated fraction of tissue irradiated and the dosimeters used to provide an indication of dose to each organ

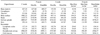
Table 4
Current International Commission on Radiological Protection (ICRP) tissue weighting factors (WT)28 for calculation of effective dose
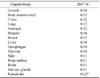
Table 6
Equivalent dose (µSv) at various organ and tissues exposed on the adult standard exposure setting according to the imaging modes
References
1. Arai Y, Tammisalo E, Iwai K, Hashimoto K, Shinoda K. Development of a compact computed tomographic apparatus for dental use. Dentomaxillofac Radiol. 1999; 28:245–248.

2. Momin MA, Matsumoto K, Ejima K, Asaumi R, Kawai T, Arai Y, et al. Correlation of mandibular impacted tooth and bone morphology determined by cone beam computed topography on a premise of third molar operation. Surg Radiol Anat. 2013; 35:311–318.

3. Patel S, Dawood A, Whaites E, Pitt Ford T. New dimensions in endodontic imaging: part 1. Conventional and alternative radiographic systems. Int Endod J. 2009; 42:447–462.

4. Silva MA, Wolf U, Heinicke F, Bumann A, Visser H, Hirsch E. Cone-beam computed tomography for routine orthodontic treatment planning: a radiation dose evaluation. Am J Orthod Dentofacial Orthop. 2008; 133:640.e1–640.e5.

5. Lofthag-Hansen S, Gröndahl K, Ekestubbe A. Cone-beam CT for preoperative implant planning in the posterior mandible: visibility of anatomic landmarks. Clin Implant Dent Relat Res. 2009; 11:246–255.

6. Loubele M, Bogaerts R, Van Dijck E, Pauwels R, Vanheusden S, Suetens P, et al. Comparison between effective radiation dose of CBCT and MSCT scanners for dentomaxillofacial applications. Eur J Radiol. 2009; 71:461–468.

7. Jeong DK, Lee SC, Huh KH, Yi WJ, Heo MS, Lee SS, et al. Comparison of effective dose for imaging of mandible between multi-detector CT and cone-beam CT. Imaging Sci Dent. 2012; 42:65–70.

8. Roberts JA, Drage NA, Davies J, Thomas DW. Effective dose from cone beam CT examinations in dentistry. Br J Radiol. 2009; 82:35–40.

9. Pauwels R, Beinsberger J, Collaert B, Theodorakou C, Rogers J, Walker A, et al. Effective dose range for dental cone beam computed tomography scanners. Eur J Radiol. 2012; 81:267–271.

10. Qu XM, Li G, Ludlow JB, Zhang ZY, Ma XC. Effective radiation dose of ProMax 3D cone-beam computerized tomography scanner with different dental protocols. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 110:770–776.

11. Davies J, Johnson B, Drage N. Effective doses from cone beam CT investigation of the jaws. Dentomaxillofac Radiol. 2012; 41:30–36.

12. Theodorakou C, Walker A, Horner K, Pauwels R, Bogaerts R, Jacobs R, et al. Estimation of paediatric organ and effective doses from dental cone beam CT using anthropomorphic phantoms. Br J Radiol. 2012; 85:153–160.

13. ICRP. Diagnostic reference levels in medical imaging: review and additional advice. A web module produced by Committee 3 of the International Commission on Radiological Protection (ICRP) [Internet]. Otawa: ICRP;2001. cited 2012 September 30. Available from: http://www.icrp.org/docs/DRL_for_web.pdf.
14. Kim EK. Development of diagnostic reference level in dental x-ray examination in Korea [Internet]. Osong: Korea Food and Drug Administration;2009. cited 2012 September 30. Available from: http://rnd.mfds.go.kr.
15. Goo HW. Development of the diagnostic reference level of pediatric chest radiography [Internet]. Osong: Korea Food and Drug Administration;2009. cited 2012 September 30. Available from: http://rnd.mfds.go.kr.
16. Kim HJ. Study for establishment of diagnostic reference level of patient dose in skull radiography [Internet]. Osong: Korea Food and Drug Administration;2009. cited 2012 September 30. Available from: http://rnd.mfds.go.kr/.
17. Sung DW. Investigation of patient dose for diagnostic reference levels (DRL) in radiographic examination: National survey in Korea [Internet]. Osong: Korea Food and Drug Administration;2011. cited 2012 September 30. Available from: http://rnd.mfds.go.kr.
18. Thilander-Klang A, Helmrot E. Methods of determining the effective dose in dental radiology. Radiat Prot Dosimetry. 2010; 139:306–309.

19. Helmrot E, Alm Carlsson G. Measurement of radiation dose in dental radiology. Radiat Prot Dosimetry. 2005; 114:168–171.

20. Holroyd JR, Walker A. HPA-RPD-065. Recommendations for the design of X-ray facilities and quality assurance of dental Cone Beam CT (Computed Tomography) systems. Chilton: Health Protection Agency;2010.
21. Lofthag-Hansen S, Thilander-Klang A, Ekestubbe A, Helmrot E, Gröndahl K. Calculating effective dose on a cone beam computed tomography device: 3D Accuitomo and 3D Accuitomo FPD. Dentomaxillofac Radiol. 2008; 37:72–79.

22. Schultz FW, Zoetelief J. Dose conversion coefficients for interventional procedures. Radiat Prot Dosimetry. 2005; 117:225–230.

23. Compagnone G, Giampalma E, Domenichelli S, Renzulli M, Golfieri R. Calculation of conversion factors for effective dose for various interventional radiology procedures. Med Phys. 2012; 39:2491–2498.

24. Hart D, Wall BF. NRPB-W4. Radiation exposure of the UK population from medical and dental X-ray examinations. Chilton: National Radiological Protection Board;2002.
25. Looe HK, Eenboom F, Chofor N, Pfaffenberger A, Steinhoff M, Rühmann A, et al. Conversion coefficients for the estimation of effective doses in intraoral and panoramic dental radiology from dose-area product values. Radiat Prot Dosimetry. 2008; 131:365–373.

26. Looe HK, Eenboom F, Chofor N, Pfaffenberger A, Sering M, Rühmann A, et al. Dose-area product measurements and determination of conversion coefficients for the estimation of effective dose in dental lateral cephalometric radiology. Radiat Prot Dosimetry. 2007; 124:181–186.

27. Ludlow JB, Ivanovic M. Comparative dosimetry of dental CBCT devices and 64-slice CT for oral and maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008; 106:106–114.

28. The 2007 Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann ICRP. 2007; 37:1–332.
29. Radiation protection No. 172. Evidence based guidelines on cone beam CT for dental and maxillofacial radiology [Internet]. Luxemburg: European commission;2012. cited 2012 September 30. Available from: http://ec.europa.eu/energy/nuclear/radiation_protection/doc/publication/172.pdf.




 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download