Abstract
One of the most common oral surgical procedures is the extraction of the lower third molar (LTM). Postoperative complications such as paresthesia due to inferior alveolar nerve (IAN) injury are commonly observed in cases of horizontal and vertical impaction. The present report discusses a case of a vertically impacted LTM associated with a dentigerous cyst. An intimate contact between the LTM roots and the mandibular canal was observed on a panoramic radiograph and confirmed with cone-beam computed tomographic (CBCT) cross-sectional cuts. An orthodontic miniscrew was then used to extrude the LTM prior to its surgical removal in order to avoid the risk of inferior alveolar nerve injury. CBCT imaging follow-up confirmed the success of the LTM orthodontic extrusion.
One of the most common oral surgical procedures is the lower third molar (LTM) extraction. The closer the relationship between LTM and the inferior alveolar nerve (IAN), the more difficult it is to remove the LTM.1 Postoperative complications such as paresthesia due to IAN injury are frequently observed in cases of this type of surgery, particularly in cases of LTM horizontal or vertical impaction, because of LTM proximity to the IAN.1,2 Curved or thin roots have also been described as risk factors causing IAN damage.3
Two different orthodontic maneuvers used to minimize the risk of IAN injury during LTM extraction have been recently described in the literature.4,5 According to their results, orthodontic forces might be used to extrude the vertically impacted LTM, allowing the surgeon to perform a safe extraction. However, both of these maneuvers involve application of orthodontic brackets, either in the mandibular molars4 or in the antagonist maxillary molars.5
Another study described the first-time use of an orthodontic miniscrew placed in the mandible, near the lower first molar, to offer the anchorage needed to apply orthodontic forces to extrude the LTM.6 Nevertheless, this study reported that passive bracketing on the mandibular molars of the same side was also required and led to patient discomfort during treatment.6 The role of miniscrews in cases of LTM orthodontic extrusion was also mentioned by Wang et al.5 However, no clinical or tomographic images of the procedure were shown in their study.
Thus, the present study aimed to report the usefulness of cone-beam computed tomographic (CBCT) imaging follow-up in a case of orthodontic extrusion of a vertically impacted LTM by using a sole orthodontic miniscrew.
A 34-year-old male patient with no systemic conditions or any metabolic disorders presented with a previously taken routine panoramic radiograph showing signs of a close relationship between the left LTM and the mandibular canal, such as darkening and deflection of the roots, and narrowing and diversion of the mandibular canal. This initial radiographic analysis led us to suggest that the patient undergo a CBCT scan, which he did. A CBCT machine (i-CAT Classic, Image Sciences International, Hatfield, PA, USA) was used and configured with the following diagnostic protocol: 0.25 mm voxel, 120 kVp, 8 mA, and field of view (FOV) 16 cm in diameter and 6 cm in height. From the scan, three-dimensional (3D) reconstructed images were rendered using DentalSlice® (Bioparts, São Paulo, Brazil) software.
On these preoperative CBCT images, the vertical impaction of the left LTM was confirmed and classified as level B(LTM partially buried in the bone), according to Pell and Gregory's classification.7 Additionally, a cyst-like lesion was found associated with its crown. Cross-sectional CBCT images showed that the mandibular canal came into contact with a root curvature and the lingual plate (Fig. 1). Because of its intimate contact with the mandibular canal, it could be foreseen that LTM surgical extraction would increase the risk of IAN injury. Therefore, we decided to use an orthodontic miniscrew to extrude the LTM prior to its surgical removal. The risks and benefits of the available treatment options were explained to the patient, and he decided in favor of using the miniscrew to extrude the LTM and provided informed consent.
The first step of the treatment was to perform an initial surgical procedure to remove the bone around the occlusal and buccal surfaces of the LTM crown by using a piezoelectric surgical unit (Piezosonic, Driller®, São Paulo, SP, Brazil) and to remove the cyst lesion associated with this crown. The diagnosis of a dentigerous cyst was confirmed by histological analysis. After an 8 week healing period, there was gingival recession, and part of the LTM occlusal surface was seen in the clinical examination. Accordingly, an orthodontic separator was installed to avoid LTM impaction caused by contact with the adjacent second molar. Two weeks later, a periapical radiograph was taken. According to the images, contact between the two teeth was actually prevented.
Thus, an orthodontic miniscrew (8 mm in length and 1.5 mm in diameter; Morelli, São Paulo, Brazil) was inserted into the buccal cortex between the first and second antagonist maxillary molars. Elastic traction was applied between the miniscrew and the orthodontic hook installed on the LTM occlusal surface with two orthodontic elastics. During the first week, the miniscrew orthodontic anchorage was applied. The patient reported a light "pins and needles" sensation in part of the tongue, lasting 3 days. At 3 weeks after miniscrew installation, the LTM was extruded markedly (Fig. 2), confirmed by CBCT coronal panoramic (Fig. 3) and cross-sectional follow-up images (Fig. 4). At this time, the LTM was surgically extracted. The roots did not fracture, and the LTM was easily removed from the alveolar socket. During surgery, there was no excessive bleeding or pain. No IAN damage or exposure was clinically observed. The root curvature, found to be in contact with the mandibular canal, was observed by examining the LTM after it was extracted and cleaned (Fig. 5). The patient's postoperative recovery was uneventful. The patient stated no significant discomfort during the LTM extrusion period, or during the extraction surgery. Additionally, no adjacent mandibular second molar loosening or displacement was observed during the entire treatment time. No postoperative complications were observed in a follow-up period of 28 months.
In some studies on LTM extraction, panoramic radiography has been used as an initial examination to check the proximity between LTM roots and the IAN.4,5,6 However, it does not offer cross-sectional images of the surgery site. Computed tomographic (CT) images have been described as essential tools to diagnose the contact between LTM and the mandibular canal three-dimensionally.8 These findings are in accordance with what was observed in the present case report, insofar as CBCT imaging detected the intimate contact between root curvatures and the IAN, confirmed by the LTM shape observed after its extraction.
In the present case, pre- and postoperative CBCT scans were necessary to confirm the detachment of the left LTM roots from the mandibular canal. Compared with other CT methods, CBCT offers advantages such as reduced effective radiation doses, shorter acquisition scan time, easier imaging, and lower costs.9 In addition, an FOV of 6 cm in height was used to restrain the scan to the mandible area. For this type of scan in standard resolution, the effective doses emitted by the CBCT device used in this study were 23.9 µSv and 96.2 µSv (using both the 1990 and the recently approved 2007 International Commission on Radiological Protection recommended tissue weighting factors, respectively).10
In order to avoid IAN injury risks during LTM extraction, different orthodontic approaches have been developed. 4,5 Bonetti et al4 demonstrated a technique of complex orthodontic appliances used in the inferior arch and required to achieve the anchorage needed to extrude LTM, which was the main disadvantage of their technique.4 On the other hand, two other studies on an orthodontic aid to extrude LTM described a simpler technique to make LTM surgical removal easier, and observed that this technique could also be important to improve the periodontal status of the neighboring sites.11 Additionally, these studies reported that a minimum period of 3 months was required to achieve satisfactory orthodontic extrusion of the LTM.4,11
Another article on orthodontic-aided extraction of a vertically impacted LTM showed a technique of bracketing the antagonist maxillary molars to achieve the anchorage required to extrude the LTM using elastic traction.5 According to their study, a mean period of 35 days was required to complete the orthodontic LTM traction. This finding supported the present case, which also used elastic traction, resulting in an orthodontic treatment time of 5 weeks (2 weeks with the orthodontic separator, and 3 weeks with the mini implant with elastic traction) to obtain LTM extrusion. However, in their study, an orthodontic bracket with a hook was placed on the LTM buccal surface to establish the orthodontic elastic,5 whereas in the present case, the hook was installed on the LTM occlusal surface, leading to less contact with the patient's cheek mucosa. Furthermore, in the present case, two elastics were used, thus reducing traction time. On the other hand, an initial surgical procedure was required to remove the bone around the occlusal and buccal surfaces of the LTM crown by using a piezoelectric surgical unit, which has recently been described as an effective method of significantly reducing surgical time and avoiding postoperative complications, such as facial swelling and trismus, in cases of third molar surgery.12
As a first-time application, Park et al6 used an orthodontic miniscrew placed in the mandible, near the lower first molar, to offer the anchorage needed to extrude the LTM. In their study, CBCT cross-sectional images were used to confirm the contact between the LTM roots and the mandibular canal, thus supporting the role of CBCT imaging, as described in the present case. On the other hand, passive bracketing was also used in their study, leading to variable degrees of patient discomfort during the traction periods, contrasting with the findings of the present case report, in which no significant discomfort during orthodontic traction was reported by the patient who was analyzed.
In conclusion, the present report demonstrated the role of the miniscrew in avoiding IAN injury in cases of vertically impacted LTM extraction. Our report further supported the usefulness of CBCT imaging to diagnose the initial contact between the mandibular canal and the LTM, and their later detachment during the course of the treatment. Therefore, enhanced visualization of the mandibular canal location and its relationship with the LTM roots could improve pre-treatment and surgical planning.
Figures and Tables
Fig. 1
Initial cross-sectional cone-beam computed tomographic (CBCT) images of the site show the contact between the mandibular canal and the curvatures of the mesial (A) and distal (B) roots, depicted in different CBCT cuts.
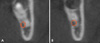
Fig. 2
A clinical photograph shows the lower third molar before (A) and after (B) orthodontic extrusion.

Fig. 3
Initial (A) and final (B) coronal panoramic CBCT reconstruction images of the site show the relationship between the lower third molar roots and the mandibular inferior alveolar canal.

References
1. Valmaseda-Castellón E, Berini-Aytés L, Gay-Escoda C. Inferior alveolar nerve damage after lower third molar surgical extraction: a prospective study of 1117 surgical extractions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001; 92:377–383.

2. Susarla SM, Blaeser BF, Magalnick D. Third molar surgery and associated complications. Oral Maxillofac Surg Clin North Am. 2003; 15:177–186.

3. Bui CH, Seldin EB, Dodson TB. Types, frequencies, and risk factors for complications after third molar extraction. J Oral Maxillofac Surg. 2003; 61:1379–1389.

4. Alessandri Bonetti G, Bendandi M, Laino L, Checchi V, Checchi L. Orthodontic extraction: riskless extraction of impacted lower third molars close to the mandibular canal. J Oral Maxillofac Surg. 2007; 65:2580–2586.

5. Wang Y, He D, Yang C, Wang B, Qian W. An easy way to apply orthodontic extraction for impacted lower third molar compressing to the inferior alveolar nerve. J Craniomaxillofac Surg. 2012; 40:234–237.

6. Park W, Park JS, Kim YM, Yu HS, Kim KD. Orthodontic extrusion of the lower third molar with an orthodontic mini implant. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 110:e1–e6.

7. Pell GJ, Gregory BT. Impacted mandibular third molars: classification and modified techniques for removal. Dent Digest. 1933; 39:330–338.
8. Tantanapornkul W, Okouchi K, Fujiwara Y, Yamashiro M, Maruoka Y, Ohbayashi N, et al. A comparative study of cone-beam computed tomography and conventional panoramic radiography in assessing the topographic relationship between the mandibular canal and impacted third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007; 103:253–259.

9. Scarfe WC, Farman AG, Sukovic P. Clinical applications of cone-beam computed tomography in dental practice. J Can Dent Assoc. 2006; 72:75–80.
10. Roberts JA, Drage NA, Davies J, Thomas DW. Effective dose from cone beam CT examinations in dentistry. Br J Radiol. 2009; 82:35–40.

11. Guida L, Cuccurullo GP, Lanza A, Tedesco M, Guida A, Annunziata M. Orthodontic-aided extraction of impacted third molar to improve the periodontal status of the neighboring tooth. J Craniofac Surg. 2011; 22:1922–1924.

12. Itro A, Lupo G, Marra A, Carotenuto A, Cocozza E, Filipi M, et al. The piezoelectric osteotomy technique compared to the one with rotary instruments in the surgery of included third molars. A clinical study. Minerva Stomatol. 2012; 61:247–253.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download