Abstract
Mucoepidermoid carcinomas (MECs) arising within the jaws as primary central bony lesions are termed central MECs. Central MECs are extremely rare, comprising 2-3% of all mucoepidermoid carcinomas. We herein report a rare case of central MEC of the maxilla in a 52-year-old male whose plain radiographs showed a "ground glass" pattern and computed tomographic images, a hypodense mass with numerous calcifications. To the best of our knowledge, this is the first report of central MEC showing a "ground glass" appearance.
Mucoepidermoid carcinoma (MEC) is an unusual type of malignant epithelial salivary gland tumor that originates in both major and minor salivary glands. As the name implies, MEC is composed of a mixture of cell types such as mucus secreting, epidermoid, and intermediate cells.1
Central MECs are uncommon tumors, comprising 2-3% of all mucoepidermoid carcinomas reported.2 They have been reported in patients of all ages, ranging from 1 to 78 years, with the overwhelming majority occurring in the 4th and 5th decades of life.2 They are histologically low-grade cancers, usually affecting the mandible as unilocular or multilocular radiographic lesions.3 Other radiographic manifestations of central MECs include mixed radiopaqueradiolucent lesions, destructive osteolytic lesions with ill-defined margins, and radiolucency with calcifications or new bone formation.1,2,3 However, in the present case, the lesion-affected maxilla showed a "ground glass" pattern on conventional radiographs and a destructive lesion with calcifications on computed tomographic (CT) images.
A 52-year-old male presented with a chief complaint of painful swelling of the left upper jaw; he had had the swelling for 2 months. The swelling was associated with decreased vision and watering from the left eye for this period. The patient's past medical history and family history were non-contributory. He had had the habit of smoking and alcohol consumption for 30 years.
Extraorally, a solitary swelling was observed involving the left middle third of the face, which was non-tender and hard in consistency with no changes in surface temperature (Fig. 1A). Intraorally, a well-defined swelling was located on the alveolus of the left maxilla in the region of the first, second, and third molars with obliteration of the buccal vestibule. On palpation, the swelling was non-tender, and firm to hard in consistency (Fig. 1B).
Periapical radiographs (Fig. 2) showed a characteristic "ground glass" appearance and symmetric widening of the periodontal ligament space in relation to the left maxillary canine and the first and second premolars. A panoramic radiograph (Fig. 3) revealed complete destruction of the left maxillary antral walls and zygomatic process of the maxilla, and the center of the lesion exhibited numerous calcifications.
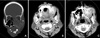
The coronal section of the CT scan (bone algorithm; Fig. 4A) revealed a hypodense mass involving the left maxillary antrum with complete destruction of the superior, inferior, medial, and lateral walls, with invasion of the mass into the nasal fossa, orbit, and the hard palate. There was also destruction of the conchae of the left nasal fossa. The inferior aspect of the lesion showed a micro-multilocular pattern, whereas the rest of the areas exhibited calcifications distributed haphazardly.
Axial sections of CT (soft tissue algorithm) showed calcifications at the left maxillary alveolar process as well as in the left maxillary antrum. Complete destruction of all walls of the left maxillary antrum was observed with diffuse calcifications (Figs. 4B and C).
Based on the radiological findings, differential diagnoses of osteosarcoma and osteoblastic metastatic malignancy such as prostate cancer were considered. An incisional biopsy was taken, and histopathology (Fig. 5) revealed solid nests of malignant tumor cells (epidermoid, intermediate, and occasional mucous cells); many of these tumor islands showed central necrosis with dystrophic calcification and a few cystic spaces. The fibrous stroma consisted of blood vessels and inflammatory cells. Histopathology confirmed high-grade MEC. Based on these findings, a final diagnosis of a central MEC of the left maxilla was made.
Central MECs are uncommon malignancies affecting the jaws, which are usually of the "low-grade" variety. The mandible has a higher predilection than the maxilla often with a unilocular/multilocular radiographic presentation.3 However, in the present case, the maxilla was affected and did not exhibit a regular radiographic unilocular/multilocular pattern. Instead, an osteolytic lesion containing calcifications with infiltrative margins was seen, which was probably attributed to the "high-grade" variety observed in this case. This was in accordance with Rabinov's study, which stated that high-grade lesions might show infiltration, cyst formation, necrosis, and calcifications.4
The present case was considered to be a central variety of MEC, as all the criteria proposed and modified by Browand and Waldron were satisfied.5 The intactness of the cortical plates was one of the most important criteria for a lesion to be considered of the central variety. However, the present case was considered "central" in spite of cortical destruction since Brookestone and Huvos considered similar cases with cortical perforation/destruction to be the "central" variety and categorized them as stage III.6
Radiographically, central MECs exhibit a unilocular/multilocular appearance.3 The present case showed various unusual radiographic findings. The plain radiographs showed a characteristic "ground glass" appearance, which has not been previously reported elsewhere in the literature. We hypothesized that the presence of numerous calcifications in the lesion, at the level of the maxillary alveolus as demonstrated on the axial CT images of our case, could have contributed to the "ground glass" appearance in this case. Secondly, the presence of diffuse calcification within the lesion, as observed in the CT images, is an unusual radiographic finding for central MEC cases. Only a few case reports with calcifications have been documented in the literature.7,8 Kurabayashi et al described the degree of malignancy with calcifications in salivary gland malignant tumors. The higher the grading, the greater are the chances of calcification.9
Yoon et al proposed four mechanisms to explain the process of calcification: as a result of hypercalcemia, as a component of the tumor, as dystrophic calcification of necrotic areas, and as calcification of the material secreted by neoplastic cells.10
Histologically, the present case conformed to all the characteristic findings of a high-grade MEC, like infiltration, necrosis, and calcification.4
Most of the reported central MECs were histologically low-grade tumors and usually carried a favorable prognosis.3 However, since the present case was a "high-grade" variant, which behaved aggressively, the patient was subjected to surgical resection of the maxilla followed by radiotherapy.
To conclude, the present case exhibited unusual radiographic findings like a "ground glass" pattern with concurrent "calcifications." With the increasing number of case reports of central MECs showing a mixed radiolucentradiopaque pattern due to calcifications, one has to consider central MEC to be one of the radiographic differential diagnoses for mixed radiolucent-radiopaque lesions, particularly those involving the maxillary antrum. Moreover, it was interesting to observe the "ground glass" pattern in our case of central MEC, which has never been reported in the previous literature.
Figures and Tables
Fig. 1
A. A well-defined extraoral swelling is present on the left middle third of the face. B. A well-defined intraoral swelling is present on the left maxilla causing obliteration of the buccal vestibule.

Fig. 2
Periapical radiographs show a "ground glass" appearance and symmetric widening of the periapical ligament space of the teeth.

Fig. 3
Panoramic radiograph shows complete destruction of all walls of the left maxillary antrum with calcifications.

Fig. 4
A. A coronal computed tomographic (CT) image exhibits a large hypodense mass with calcifications involving the left maxillary antrum invading the orbit and the nasal fossa. B. Axial CT image shows numerous calcifications in the left maxillary alveolus region. C. Axial CT image shows calcifications in the left maxillary antrum with complete destruction of the antral walls.
References
1. Varma S, Shameena P, Sudha S, Nair RG, Varghese IV. Clear cell variant of intraosseous mucoepidermoid carcinoma: report of a rare entity. J Oral Maxillofac Pathol. 2012; 16:141–144.

2. Simon D, Somanathan T, Ramdas K, Pandey M. Central mucoepidermoid carcinoma of mandible - A case report and review of the literature. World J Surg Oncol. 2003; 1:1.
3. Tucci R, Matizonkas-Antonio LF, de Carvalhosa AA, Castro PH, Nunes FD, Pinto DD Jr. Central mucoepidermoid carcinoma: report of a case with 11 years' evolution and peculiar macroscopical and clinical characteristics. Med Oral Patol Oral Cir Bucal. 2009; 14:E283–E286.
5. Browand BC, Waldron CA. Central mucoepidermoid tumors of the jaws. Report of nine cases and review of the literature. Oral Surg Oral Med Oral Pathol. 1975; 40:631–643.
6. Brookstone MS, Huvos AG. Central salivary gland tumors of the maxilla and mandible: a clinicopathologic study of 11 cases with an analysis of the literature. J Oral Maxillofac Surg. 1992; 50:229–236.

7. do Prado RF, Lima CF, Pontes HA, Almeida JD, Cabral LA, Carvalho YR, et al. Calcifications in a clear cell mucoepidermoid carcinoma: a case report with histological and immunohistochemical findings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007; 104:e40–e44.

8. Sherin S, Sherin N, Thomas V, Kumar N, Sharafuddeen KP. Central mucoepidermoid carcinoma of maxilla with radiographic appearance of mixed radiopaque-radiolucent lesion: a case report. Dentomaxillofac Radiol. 2011; 40:463–465.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download