Introduction
The success of dental implants can be assessed clinically and radiologically. In terms of the radiological assessment, the features of successful implantation include a mean crestal bone loss of no greater than 1.6 mm during the first postoperative year and no greater than 0.13 mm through the maintenance period, and lack of peri-implant radiolucency.
1,
2 However, we have little knowledge of the effects produced by functional endosseous implants on the quality and architecture of the surrounding trabecular bone.
Imaging is an essential part of endosseous implant therapy in preoperative, intraoperative, and follow-up assessments. An ideal imaging technique should reveal many significant characteristics at specific stages of the implant therapy. Therefore, a combination of radiograph techniques is used with certain indications.
3
Digital radiography is known to be one of the most sensitive methods for assessing subtle changes in trabecular bone density. It has high image photometric accuracy, wide dynamic range, and high resolution capacity for dental assignments.
3 Furthermore, it allows for image enhancement and processing on a computer monitor, such as magnification, skeletonization, and contrast optimization.
3,
4,
5
The objective of this study was to assess the trabecular bone changes that occurred around functional endosseous dental implants by means of radiographic image analysis techniques. A specific image analysis technique was performed in order to quantify the structural elements of the trabecular bone. Accordingly, the null hypothesis was as follows: There would be no significant quantifiable differences in the trabecular bone structure on radiographs subjected to repeated analyses.
Discussion
The development of a non-invasive technique for measuring bone architectural changes has been a challenge for many research groups.
7 Texture analysis of peripheral microtomographs has been suggested as an alternative approach.
7 However, in a dental context, these techniques are difficult for many clinical research groups because of the limited availability of equipment or practical problems in their use. However, although two-dimensional radiographic measurements fail to spot some information regarding the out-of-plane curvature of trabeculae, they have significant correlation with data provided by three-dimensional computed microtomography. Furthermore, it has been shown that trabecular bone microarchitecture can be measured by the texture analysis of radiographs of the dried bone.
8
There were some technical limitations in this clinical study that should be addressed. The first was that the images had to be modified in Adobe Photoshop, processed in EMAGO and then analyzed in Win TAS. This long course of action was rather time consuming and tedious in terms of filing and saving the images, and confusing in terms of transferring them from one system to another. This difficulty could have been overcome if a special software system had been designed specifically for dental radiology practice.
The second limitation was the size and inflexibility of the rectangular marquee tool used in the Adobe Photoshop elements, which was larger than the implant and as a result, could not follow the implant contour. This led, in some cases, to the elimination of one or two out of the three ROIs (a, b, and c). However, the elimination was consistent through the first and the second sets of the image analysis. A solution for this problem might be achieved by designing the marquee tool to be freely variable in size and shape, perhaps by using a cursor-generated freehand ROI.
Third, although images were acquired by a paralleling technique with the same X-ray machine and fixed exposure parameters, there was still some variation in the X-ray angulation that resulted in a minor difficulty of retaining the same proportions of ROI on the paired images. In some cases, there was a shortage of space around the implant on one radiograph, such that it was difficult to obtain the same ROI, leading to the exclusion of that ROI from the analysis or a change in the position of the marquee tool in others. The importance of standardization was highlighted by Jonasson et al, particularly, as mentioned above, in relation to the angulation of the X-ray beam.
9 Grondahl et al have mentioned that even minor deviations in the vertical angulations of the X-ray beam could cause discrepancies in bone measurements that could be easily observed between serial radiographs.
10 Consequently, some researchers could have reported measurement discrepancies as bone loss or gain.
11 However, our preliminary study provides a foundation for future work and gives technical guidance for a prospective study on the scope of assessment of the trabecular bone in the periapical region of dental implants. A majority of similar studies have focused on the marginal bone height and the osseointegration phase.
12,
13,
14
Our results showed a significant difference between some parameters in the baseline and follow-up sets of radiographs in terms of the increase in the value of the quantifiable changes in the trabecular bone structure around the Frialit-2 implant after being put into clinical function. This can be masked by few data throughout the individual cases, meaning that although some cases showed an increase in the follow-up values while others did not, there was an increase in the overall results. However, it can be argued that this difference could be related to the lack of perfect standardization measures in the procedure for taking radiographs.
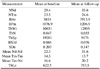
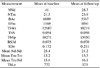
When the data from all of the patients were considered, there was no significant difference between the baseline and the follow-up radiographs for almost all the bone parameters except the bone area (BAr) and the mean distance between nodes (mean Nd-Nd). Thus, the null hypothesis was rejected for these two parameters and accepted for the others, indicating that there were no significant quantifiable changes in the trabecular bone structure around the endosseous implants after being put into clinical function for almost all of the parameters. Regarding the marrow spaces, the null hypothesis was accepted for all the parameters except for bone area (BAr) and trabecular length (TbLe). What do these results mean? Seemingly, the most convincing result was the increase in bone area in the ROIs and the concordant fall in the marrow area. Thus, it appeared that the bone around the implant underwent remodeling that resulted in a net increase in the bone after implant placement. Therefore, the effect of successful implants on the bone did not appear to be limited to the immediate implant/bone contact area. If this result was correct, then the likely explanation was the effect of stresses and strains of implant function on the bone. However, this could be related to the scientific fact that the bone is a complex organ with cells specifically devoted to a continuous process of remodeling. According to Wolff's law,
15 bone has the ability to alter its strength through the production of collagen fibers and increased deposition of minerals as a protective measure. Therefore, disuse of bone leads to atrophy, whereas increased stresses lead to bone deposition. Another probable effect of mechanical stress is the increased production of the calcitonin hormone that inhibits bone resorption. This information could be of great significance in explaining the increase in trabecular bone area (BAr) around Frialit-2 implants and relating the success of the implant to the equal distribution of stress around it.
Our cases involved implant placements into the edentulous areas of varying durations. Therefore, it was likely that a degree of bone loss in the implant site space occurred during the intervening period. Thus, we postulated that implant placement and subsequent functional stresses caused the bone deposition detected by our analysis. It would be interesting to see whether this observation would be identifiable in cases of immediate implant therapy, where there would be no intervening time allowing for bone atrophy.
In conclusion, several methods should be used in parallel to measure the trabecular architecture, as a single technique may focus on a given aspect and neglect the others. In the context of our study, identification of alternative techniques was more difficult. The small scale and fine details on dental intraoral images implied that other suggested alternative techniques (such as peripheral microtomographs) are probably not applicable. Rather, it would be possible to perform a subjective image analysis of the architectural or densitometric measurement.






 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download