Abstract
Purpose
This study aimed to provide comparative measurements of the effective dose from direct and indirect digital panoramic units according to phantoms and exposure parameters.
Materials and Methods
Dose measurements were carried out using a head phantom representing an average man (175 cm tall, 73.5 kg male) and a limbless whole body phantom representing an average woman (155 cm tall, 50 kg female). Lithium fluoride thermoluminescent dosimeter (TLD) chips were used for the dosimeter. Two direct and 2 indirect digital panoramic units were evaluated in this study. Effective doses were derived using 2007 International Commission on Radiological Protection (ICRP) recommendations.
Results
The effective doses of the 4 digital panoramic units ranged between 8.9 µSv and 37.8 µSv. By using the head phantom, the effective doses from the direct digital panoramic units (37.8 µSv, 27.6 µSv) were higher than those from the indirect units (8.9 µSv, 15.9 µSv). The same panoramic unit showed the difference in effective doses according to the gender of the phantom, numbers and locations of TLDs, and kVp.
Conclusion
To reasonably assess the radiation risk from various dental radiographic units, the effective doses should be obtained with the same numbers and locations of TLDs, and with standard hospital exposure. After that, it is necessary to survey the effective doses from various dental radiographic units according to the gender with the corresponding phantom.
Panoramic radiography has been widely used as a diagnostic tool because it is easy to provide a radiographic overview of the teeth and surrounding anatomical structures.1,2 Recently, a number of dental practitioners have come to prefer digital radiography over conventional film radiography.3-6 One of the main advantages of digital radiography compared with conventional film radiography is the possibility of reducing the radiation dose to patients.7 Diagnostic benefits and possible dose hazard trade-offs are important considerations in the choice of radiographic procedures. Since X-ray risks are cumulative, the choice of radiographic unit should be considered in examining all patients for dose reduction.8 Digital panoramic equipment requires the evaluation of the radiation dose to patients according to the machines, and in maxillofacial panoramic imaging, the radiation dose of the machines should follow the principle of keeping the dose as low as reasonably achievable (ALARA).
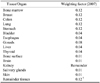
The effective dose (E) is a concept and approach recommended by the International Commission on Radiological Protection (ICRP) to estimate the damage from radiation to the exposed population.9 E is a widely used calculation that permits comparison of the detriment of different exposures, including specific area exposure,10 to ionizing radiation to an equivalent detriment produced by a full body dose of radiation.8 White11 used this approach in 1992 in assessing the radiation risk from various dental radiographic examinations. The unit of the effective dose is the sievert (Sv) and it is calculated by the equation: E=ΣHT×WT, where E is the product of the tissue weighting factor (WT), which represents the relative contribution of each organ or tissue to the overall risk, and the equivalent dose (HT).12 The whole-body risk is acquired by the summation of the weighted equivalent doses to all exposed tissues or organs. The earlier 1990 ICRP tissue-weighting factors,13 2005 weighting factors, and the new 2007 weighting factors12 were used to calculate the effective dose.7,8,14 Newly adopted recommendations from the ICRP provide revision of tissue-weighting factors and inclusion of salivary glands as a weighted tissue. These changes resulted in an upward reassessment of the effective dose from oral and maxillofacial radiographic examinations.12
The studies of the absorbed dose or effective dose from each exposure program of the film-based panoramic machine with a limbless whole body phantom and a head phantom were reported by Lecomber et al in 200015 and Choi et al in 2001,16 respectively. The tissue-absorbed dose and the whole-body effective dose (E) for a new generation film-based panoramic machine (Planmeca PM 2002 CC Proline, Planmeca, Helsinki, Finland), operating in the panoramic examination mode with a head phantom, was studied by Danforth et al in 2000.14 Gijbels et al7 reported that the effective radiation doses ranged from 4.7 µSv to 14.9 µSv for various digital panoramic units with a head phantom using the 2005 recommendations of the ICRP.
Few studies have reported the difference in radiation dose between direct and indirect digital panoramic units. Also, to our knowledge, no studies have been published addressing the difference in the assessment of the effective dose using a head versus a whole body phantom.
Ludlow and Ivanovic8 reported that there was large difference in the radiation dose between the "standard" and "ultra" exposure in the Iluma CBCT unit. They also mentioned that a substantial difference in the effective dose was found according to variations in technique even when they evaluated the same CBCT unit. Therefore, it is necessary to prepare standardized conditions for calculation of the effective dose to compare the radiation risk from various dental radiographic examinations.
The aim of the present study is to provide the comparative measurements of the effective dose from direct and indirect digital panoramic units according to phantoms and exposure parameters. The average tissue-absorbed dose, weighted (equivalent) radiation dose, and effective dose were calculated for the anatomy of the head and neck area and the whole body with the corresponding phantom, respectively.
The digital panoramic units used for this study were the ProMax (Planmeca, Helsinki, Finland), Orthopantomograph OP100 (Imaging Instrumentarium, Tusula, Finland), and 2 ProlineXC units (Planmeca, Helsinki, Finland). Table 1 shows the technical and phantom parameters for the direct and indirect panoramic units used. Both the radiation exposure dose and the latitude of the TLD are too small to be measured with reliability; therefore, the TLD loaded phantom was exposed to radiation by the dosimeters ten times. Then, the obtained values were divided by ten to obtain one individual value for each region, subtracting each background dose. The phantom was positioned in accordance with the manufacturer's specifications for each machine, following the reference lines and head rests. The standard examination was carried out for each unit and the dosimetry was performed for each technique in order to ensure reliability.
Dose measurements were carried out using two anthropomorphic phantoms. The head phantom (Rando ART-210, Alderson Research Laboratories, Long Beach, CA, USA) representing an average man (175 cm tall, 73.5 kg male) (Fig. 1) and the limbless whole body phantom (Rando ART-300, Alderson Research Laboratories, Long Beach, CA, USA) representing an average woman (155 cm tall, 50 kg female) (Fig. 2) consisted of 9 and 31 transverse sections, respectively. The reservoirs for the placement of radiation dosimetry measuring devices were prepared to correspond to the anatomic sites of interest. Lithium fluoride thermoluminescent dosimeter (TLD) chips (Harshaw TLD-100, Thermo Electron Co., Oakwood Village, OH, USA) were used as dosimeters. The absorbed doses at the selected locations, corresponding to the radiosensitive organs of interest, were measured using two sets of 60 and 96 TLDs. The 30 and 48 phantom sites both inside and on the surface of each phantom can be seen in Table 2. Two dosimeters were placed in each anatomical site to calculate the mean value of each location, while retaining the same dosimeters in the same positions for each exposure. A set of dosimeters were kept separately to record the background radiation. Before the study, all of the dosimeters were calibrated using the same type and range of radiation that would be used during the experiments. Prior to every exposure, the dosimeters were annealed at 100℃ for 1 hour, 400℃ for 2 hours, and then cooled to 35℃. All of the TLDs were read in accordance with the manufacturer's directions after each exposure using a Harshaw 3500 TLD Reader (Harshaw/Bicron, Solon, OH, USA).
After reading, an individual sensitivity value was applied for each TLD. Exposure doses were recorded in nanocoulombs (nC) and, after the application of energy calibration factors (RCF, reader calibration factor; and ECC, element correction coefficient), the dosimetry data were converted into micrograys (µGy) and subsequently recorded. The standard deviation of the readings from the TLDs was less than 30%. Doses from two TLDs located at different points in the same tissue or organ were averaged, resulting in the average organ absorbed dose. The weighted dose for bone marrow of the whole body phantom was calculated using the sum of the radiation from the calvarium, mandibular body and ramus, cervical, thoracic, and lumbar vertebrae, and sacrum. The weighted dose for the bone marrow of the head phantom was calculated using the sum of the radiation from the calvarium, mandibular body and ramus, and cervical vertebra. Sublingual, submandibular, and parotid salivary gland doses were used for calculating the weighted dose for the salivary glands. The thyroid gland dose was individually calculated taking its specific weighted factor into consideration. For the skin surface area, fifteen points were measured: the posterosuperior surface of the head, thyroid surface, back of the thorax, and both sides of the right and left of the temporal region, lens of the eye, cheek, back of the neck, axilla, and breast (Table 2).
The products of these average organ absorbed doses and the percentage of a tissue or organ irradiated (Tables 3 and 4) in a radiographic examination were used to calculate the equivalent dose (HT) in microsieverts (µSv).12 The effective dose was calculated by multiplying actual organ doses (equivalent dose; HT) by 'risk weighting factors' as follows: E=ΣHT×WT. The tissue weighting factor (WT) represents the contribution that each specific tissue or organ makes to the overall risk. The whole-body risk was found by the summation of the tissue weighted equivalent doses to all tissues or organs exposed. Effective doses were derived using 2007 ICRP recommendations12 (Table 5). This dose was expressed in microsieverts (µSv). The obtained effective dose from each panoramic unit was compared with the dosimetric values calculated from the 24 anatomical sites of the phantoms used by Ludlow and Ivanovic8.
Table 6 shows the dosimetric results. The equivalent doses and the effective doses were expressed in µSv. The greatest individual organ doses for all examinations were measured in the salivary tissue.
The effective radiation doses ranged between 8.9 µSv and 37.8 µSv for the 4 digital panoramic units. By using a head phantom, the effective doses from the ProMax (37.8 µSv) and ProlineXC (27.6 µSv) direct digital panoramic units were higher than those from the Orthopantomograph OP100 (8.9 µSv) and ProlineXC (15.9 µSv) indirect units.
The effective dose from the same panoramic unit (Orthopantomograph OP100) using the same head phantom was higher at 83 kVp than at 72 kVp.
Comparison of effective doses with parameters; the exposure, phantom (gender), and calculation method can be found in Table 7.
The effective dose from the ProlineXC (direct) with an exposure of 70 kVp and 12 mA was 36.8 µSv by the calculation for the head region of the whole body phantom and 27.6 µSv by the head phantom. The effective dose from the Orthopantomograph OP100 (indirect) with an exposure of 72 kVp and 12 mA was 13.6 µSv by the calculation for the head region of the whole body phantom and 8.9 µSv by the head phantom. The effective doses from the direct and indirect digital units were both higher with the female phantom than with the male one.
The effective doses calculated by the method of Ludlow and Ivanovic were lower than those calculated by the authors from each panoramic examination.
The equivalent dose is used to compare the effects of different types of radiation on tissues or organs, presented in sieverts (Sv). The equivalent dose (HT) was calculated according to the equation: HT=ΣWR×DT, where the equivalent dose (HT) for a tissue or organ is the product of the radiation weighting factor (WR) and the average absorbed dose (DT) measured for that specific organ.13 The products of these values and the percentage of a tissue or organ irradiated (Table 3) in a radiographic examination were used to calculate the equivalent dose (HT) in microsieverts (µSv).12
The equivalent doses from the indirect and direct digital panoramic units were highest in the remainders and salivary glands (Table 6). The next highest equivalent doses to other organs were the following, in order: bone surface, thyroid gland, and bone marrow. Several studies on panoramic units have pointed out that the salivary gland tissue is one of the organs receiving the highest individual organ doses during maxillofacial imaging7,15,17 and our results confirmed these findings. Lecomber et al15 indicated that the influence on the calculated effective dose of treating the salivary tissue as a remainder organ deserved discussion in 2000. Ludlow and Ivanovic8 explained this by the fact that the rotational centers of panoramic units for the jaws coincide with the location of the salivary glands. Because anatomy at the rotational center is continuously exposed, effective doses from dental panoramic imaging will be larger than imaging procedures that produce a more uniform distribution of absorbed energy within the scanned region. It seems reasonable to include salivary gland exposures in calculations of effective dose until these exposures could be shown not to be significant.18 The effective doses in this study were calculated with inclusion of the salivary gland tissue using 0.01 according to the 2007 ICRP tissue weights.12 Dental radiographic examinations resulted in negligible doses to the gonads, and hereditary doses were not effective for the calculation of detriment in this study. The use of a head phantom or only the head region calculation of the whole body phantom is thought to be reasonable for the calculation of detriment from dental radiographic examinations.
The effective dose is the product of the ICRP's tissue weighting factor (WT) for the type of tissue or body and the human-equivalent dose for tissue (HT). The effective dose is calculated by multiplying actual organ doses by 'risk weighting factors' (associated with individual organ sensitivities) and represents the dose that the total body could receive and that would provide the same cancer risk as the application of different doses to various organs.13 One sievert of effective dose carries with it a 4.1% chance of developing fatal cancer in an adult worker and a 5.5% chance in a whole population, and a 0.8% chance of hereditary defect in future offspring.12 The ICRP recommends limiting artificial irradiation of the public to an average effective dose of 1 mSv per year, not including medical and occupational exposures.12
The effective doses from the ProMax (37.8 µSv) and ProlineXC (27.6 µSv) direct digital panoramic units were higher than those from the Orthopantomograph OP100 (8.9 µSv) and ProlineXC (15.9 µSv) indirect units by using the head phantom (Table 7). Gijbels et al7 reported that comparable results (9.35 µSv for CCD, 8.1 µSv for storage phosphor) were found for the various digital panoramic units when the effective dose data of the direct panoramic units were averaged and compared with the indirect units. The effective doses from both types of digital panoramic unit evaluated in this study were larger than the results of Gijbels et al.
Given that comparison of the effective doses from the different panoramic units was difficult because of the different exposure settings, Gijbels et al7 reported that by considering per unit of exposure (mAs), the Orthoralix yielded the lowest dose per mAs (0.10 µSv mAs-1), but the Veraviewepocs the highest (0.17 µSv mAs-1), and that the influence of the tube potential was less clear. Actually, for the comparison of the effective doses from the different units having different exposure settings recommended for the preservation of diagnostic image quality, the doses per unit of exposure are thought not to be significant. In the present study design, the X-ray parameters used were those for an adult as usual in the hospital. The results obtained are thought to be reasonable for the comparison of effective doses from several digital panoramic units considering the respective technical aspects of each radiation unit for good image quality, such as the size of the radiation field and shape of the focal trough.
Considering the phantom parameters, the effective dose from the indirect digital panoramic units by the calculation for the head region of the whole body phantom (13.6 µSv) was higher than that of the head phantom (8.9 µSv). The effective dose from the direct units by the calculation for the head region of the whole body phantom (36.8 µSv) was also higher than that of the head phantom (27.6 µSv) (Table 7). In addition, the effective dose was higher with the female phantom than with the male phantom in both types of digital units. This is because the absorbed dose at each TLD dose in the phantom depends on the skull size19 and soft tissue morphology of the phantom, which simulate an actual man and woman.
The effective dose calculated from the 24 anatomical sites of the phantom used by Ludlow and Ivanovic8 was lower than the obtained effective dose from each panoramic unit in this study. The numbers of anatomical sites of the phantoms for their calculation of the effective dose were less than the numbers of anatomical sites in this study. Furthermore, the difference in the location (left, center, right) and numbers of sites for the TLDs at the same selected organs can account for the small difference in effective dose between the calculations of the present study and their study.
Besides, small variations in collimator adjustment or phantom position within the unit may account for the very nearly 23% difference seen between the dosimeter values for the 2 modes of one unit.8 The slight discrepancy in the location of the TLD or phantom position are magnified as the TLD is positioned inside or outside of the field of direct radiation.18
The effective doses from direct digital panoramic units were higher than from the indirect units. Even the same panoramic unit showed a difference in effective doses according to the gender of the phantom, number and locations of TLDs, and kVp. To reasonably assess the radiation risk from various dental radiographic units, the effective doses should be obtained with the same number and locations of TLDs, and with usual hospital exposure. After that, a survey on the effective doses from various dental radiographic units must be performed according to the gender with corresponding phantoms.
Figures and Tables
Table 3
Estimated percentage of tissue irradiated with the head phantom

*Bone surface dose=bone marrow dose×bone/muscle mass energy absorption, coefficient ratio=-0.0618×2/3 kV peak+6.9406 using data.8
Table 4
Estimated percentage of tissue irradiated with the whole body phantom

*Bone surface dose=bone marrow dose×bone/muscle mass energy absorption coefficient ratio=-0.0618×2/3 kV peak+6.9406 using data.8
References
1. Rushton VE, Horner K, Worthington HV. Aspects of panoramic radiography in general dental practice. Br Dent J. 1999. 186:342–344.

2. Tugnait A, Clerehugh V, Hirschmann PN. Radiographic equipment and techniques used in general dental practice: a survey of general dental practitioners in England and Wales. J Dent. 2003. 31:197–203.

3. Hildebolt CF, Couture RA, Whiting BR. Dental photostimulable phosphor radiography. Dent Clin North Am. 2000. 44:273–297.
7. Gijbels F, Jacobs R, Bogaerts R, Debaveye D, Verlinden S, Sanderink G. Dosimetry of digital panoramic imaging. Part I: Patient exposure. Dentomaxillofac Radiol. 2005. 34:145–149.

8. Ludlow JB, Ivanovic M. Comparative dosimetry of dental CBCT devices and 64-slice CT for oral and maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008. 106:106–114.

9. Radiation protection. Protection from potential exposures: application to selected radiation sources. A report of a task group of the International Commission on Radiation Protection. Ann ICRP. 1997. 27:1–61.
10. Cho JY, Han WJ, Kim EK. Absorbed and effective dose from periapical radiography by portable intraoral X-ray machine. Korean J Oral Maxillofac Radiol. 2007. 37:149–156.
11. White SC. 1992 assessment of radiation risk from dental radiography. Dentomaxillofac Radiol. 1992. 21:118–126.

12. The 2007 Recommendations of the International Commission on Radiological Protection. ICRP Publication 103. Ann ICRP. 2007. 37:1–332.
13. 1990 Recommendations of the International Commission on Radiological Protection. Ann ICRP. 1991. 21:1–201.
14. Danforth RA, Clark DE. Effective dose from radiation absorbed during a panoramic examination with a new generation machine. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000. 89:236–243.

15. Lecomber AR, Downes SL, Mokhtari M, Faulkner K. Optimisation of patient doses in programmable dental panoramic radiography. Dentomaxillofac Radiol. 2000. 29:107–112.

16. Choi SC, Lee SM. The absorbed dose from each exposure program of the Orthopos® panoramic machine. Korean J Oral Maxillofac Radiol. 2001. 31:215–219.
17. Lecomber AR, Yoneyama Y, Lovelock DJ, Hosoi T, Adams AM. Comparison of patient dose from imaging protocols for dental implant planning using conventional radiography and computed tomography. Dentomaxillofac Radiol. 2001. 30:255–259.

18. Ludlow JB, Davies-Ludlow LE, Brooks SL. Dosimetry of two extraoral direct digital imaging devices: NewTom cone beam CT and Orthophos Plus DS panoramic unit. Dentomaxillofac Radiol. 2003. 32:229–234.

19. Lee JN, Han WJ, Kim EK. Absorbed and effective dose from newly developed cone beam computed tomography in Korea. Korean J Oral Maxillofac Radiol. 2007. 37:93–102.




 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download