Abstract
A retromolar canal is an anatomical variation in the mandible. As it includes the neurovascular bundle, local anesthetic insufficiency can occur, and an injury of the retromolar canal during dental surgery in the mandible may result in excessive bleeding, paresthesia, and traumatic neuroma. Using imaging analysis software, we evaluated the cone-beam computed tomography (CT) images of two Korean patients who presented with retromolar canals. Retromolar canals were detectable on the sagittal and cross-sectional images of cone-beam CT, but not on the panoramic radiographs of the patients. Therefore, the clinician should pay particular attention to the identification of retromolar canals by preoperative radiographic examination, and additional cone beam CT scanning would be recommended.
According to cadaveric dissections, the retromolar canal (RMC) branches off the main mandibular canal and follows a recurrent path, curving in a postero-superior direction behind the third molar to open into the retromolar foramen.1 The retromolar foramen (RMF) is the opening of a RMC found in the retromolar trigone, posterior to the last molar.1
A RMC includes neurovascular bundles, which consist of arteries, numerous venules, and myelinated nerve fibers.2-6 However, the elements of a RMC have not yet been clearly defined. The canal may conduct accessory innervations to the mandibular molars2,3,6 or can even contain aberrant buccal nerves.4,5
When a retromolar canal exists, local anesthetic insufficiency can arise. An injury of the retromolar canal during dental surgery in the mandible may result in excessive bleeding, paresthesia, and traumatic neuroma.3,7,8 Moreover, the canal may be a possible route for the spread of a tumor or infection.3 Although the RMC is of clinical importance, there have been few studies on the RMC, and even those studies mostly involved analyses of cadavers or mandibles focusing on the RMF.
The studies of the RMC using panoramic radiography have reported occurrence rates of less than 1%, so the canal has been considered a rare anatomical variation.9,10 Recently, high-resolution cone-beam CT (CBCT) has become notably effective for confirming anatomical variations of the mandibular canal that cannot be assessed on panoramic radiographs.11-13
Recently, dental surgery cases such as dental implants, the surgical extraction of an impacted mandibular third molar, sagittal split ramus osteotomy, and bone block harvesting in the retromolar area have been increasing.3,8,14 Therefore, it is important to confirm the presence and location of a RMC prior to surgical procedures in the mandible.
Routine panoramic radiography and CBCT scans were performed. CBCT scanning was performed using a Ray-Scan Symphony® scanner (Ray Medical System, Seoul, Korea) in the Department of Oral and Maxillofacial Radiology of the Yonsei University Dental Hospital. The sagittal and cross-sectional images were reconstructed from the volumetric CBCT data using the imaging analysis software OnDemand 3D™ (Cybermed, Seoul, Korea).
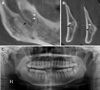
A 39-year-old male visited the Yonsei University Dental Hospital for extraction of the left mandibular third molar. On a sagittal CBCT image, a curving branch of the mandibular canal with a recurrent path at the right retromolar area was found. The passage of RMC, which branches from the mandibular canal, ended in a round radiolucent foramen of the retromolar fossa (RMF) as it moved superiorly approaching the most posterior molar area (Fig. 1A and B). The RMC was not detected on his panoramic radiograph (Fig. 1C).
A 30-year-old male visited the Yonsei University Dental Hospital with a chief complaint of inflammation in the right mandibular third molar area. Routine panoramic radiography and CBCT scans were performed for the extraction of the right third molar. It was observed that there was RMC branching from the mandibular canal that passed superiorly and in the reverse direction of the right retromolar area on sagittal images of CBCT (Fig. 2A). Two radiolucent canals surrounded by cortical bone were found on cross-sectional images perpendicular to the alveolar ridge (Fig. 2B). RMC was not detected on routine panoramic radiograph (Fig. 2C).
Analyses of the RMF using cadavers or dry mandibles have been inconsistent, with values ranging from 6.1% to 72.0%.1,11,15,16 The RMC is often classified as a subtype of the bifid mandibular canal in radiological studies.9,10,13,17 Because a RMC is generally very narrow,14 conventional radiography is not reliable in detecting RMC. However, CBCT can be used to confirm a number of anatomical variations of the mandibular canal that cannot be assessed with conventional imaging.7,12,13 Recent studies of the RMC using CBCT showed higher occurrence rates of 14.6%-65.3%7,13,18,19 than did those using panoramic radiography. The incidence of RMCs has been found to vary among different populations.1,19
Some authors have demonstrated that a neural branch to the mandibular molars arises from the mandibular canal,2,3,6 while the distal end of the RMC reaches the third mandibular molar and retromolar area. Others have reported that an aberrant buccal nerve originating from the inferior alveolar nerve within the ramus of the mandible, which runs through the RMC, can end up in the RMF and pass anterosuperiorly to be distributed into the buccinator muscle.4,5 Further studies are required to verify this buccal nerve connection.
With regard to the courses of the RMC, 3 types of RMCs were recognized by Ossenberg.1 Type 1 is a vertically curved RMC that branches from the mandibular canal around the molars from a single mandibular foramen, type 2 was a horizontally curved RMC that branches from the mandibular canal just beyond the single mandibular foramen, and type 3 is an RMC with separate foramina in the mandibular ramus that runs independently of the main mandibular canal. Some researchers7,18 have generally focused on the most common type of RMC (type 1) proposed by Ossenberg.
In conclusion, the RMC is an anatomical variation with clinical importance. It is difficult to identify a RMC using routine panoramic radiography. Therefore, the clinician must pay particular attention to the identification of a RMC by preoperative radiographic examination, and additional CBCT scanning is recommended.
Figures and Tables
Fig. 1
The sagittal (A) and cross-sectional images (B) clearly reveal a curving branch of the mandibular canal with a recurrent path at the right retromolar area (White arrow: retromolar canal, black arrow: main mandibular canal). C. The retromolar canal is not detectable on the routine panoramic radiograph.
References
2. Carter RB, Keen EN. The intramandibular course of the inferior alveolar nerve. J Anat. 1971; 108:433–440.
3. Bilecenoglu B, Tuncer N. Clinical and anatomical study of retromolar foramen and canal. J Oral Maxillofac Surg. 2006; 64:1493–1497.

4. Singh S. Aberrant buccal nerve encountered at third molar surgery. Oral Surg Oral Med Oral Pathol. 1981; 52:142.

5. Jablonski NG, Cheng CM, Cheng LC, Cheung HM. Unusual origins of the buccal and mylohyoid nerves. Oral Surg Oral Med Oral Pathol. 1985; 60:487–488.

6. Blanton PL, Jeske AH. ADA Council on Scientific Affairs, ADA Division of Science. The key to profound local anesthesia: neuroanatomy. J Am Dent Assoc. 2003; 134:753–760.
7. von Arx T, Hanni A, Sendi P, Buser D, Bornstein MM. Radiographic study of the mandibular retromolar canal: an anatomic structure with clinical importance. J Endod. 2011; 37:1630–1635.

8. Silva FM, Cortez AL, Moreira RW, Mazzonetto R. Complications of intraoral donor site for bone grafting prior to implant placement. Implant Dent. 2006; 15:420–426.

9. Langlais RP, Broadus R, Glass BJ. Bifid mandibular canals in panoramic radiographs. J Am Dent Assoc. 1985; 110:923–926.

10. Nortje CJ, Farman AG, Grotepass FW. Variations in the normal anatomy of the inferior dental (mandibular) canal: a retrospective study of panoramic radiographs from 3612 routine dental patients. Br J Oral Surg. 1977; 15:55–63.
11. Narayana K, Nayak UA, Ahmed WN, Bhat JG, Devaiah BA. The retromolar foramen and canal in south Indian dry mandibles. Eur J Anat. 2002; 6:141–146.
12. Naitoh M, Hiraiwa Y, Aimiya H, Gotoh M, Ariji Y, Izumi M, et al. Bifid mandibular canal in Japanese. Implant Dent. 2007; 16:24–32.

13. Naitoh M, Hiraiwa Y, Aimiya H, Ariji E. Observation of bifid mandibular canal using cone-beam computerized tomography. Int J Oral Maxillofac Implants. 2009; 24:155–159.
14. Kawai T, Asaumi R, Sato I, Kumazawa Y, Yosue T. Observation of the retromolar foramen and canal of the mandible: a CBCT and macroscopic study. Oral Radiol. 2012; 28:10–14.

15. Schejtman R, Devoto FC, Arias NH. The origin and distribution of the elements of the human mandibular retromolar canal. Arch Oral Biol. 1967; 12:1261–1268.

16. Sawyer DR, Kiely ML. Retromolar foramen: a mandibular variant important to dentistry. Ann Dent. 1991; 50:16–18.
17. Orhan K, Aksoy S, Bilecenoglu B, Sakul BU, Paksoy CS. Evaluation of bifid mandibular canals with cone-beam computed tomography in a Turkish adult population: a retrospective study. Surg Radiol Anat. 2011; 33:501–507.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download