Abstract
Purpose
This study was performed to determine the prevalence of bifid mandibular condyles (BMCs) in asymptomatic and symptomatic temporomandibular joint (TMJ) subjects with no traumatic history, and to assess their impact on clinical and radiographic manifestations of TMJ.
Materials and Methods
A total of 3,046 asymptomatic and 4,378 symptomatic patients were included in the study. Cone-beam computed tomography (CBCT) images were reviewed for bifid condyles. T-tests were used to compare the frequency of BMCs when stratified by symptom, gender, and side. In BMC patients, the clinical features of pain and noise, osseous changes, and parasagittal positioning of the condyles were compared between the normally shaped condyle side and the BMC side using chi-squared tests.
Results
Fifteen (0.49%) asymptomatic and 22 (0.50%) symptomatic patients were found to have BMCs. Among the bilateral cases, the number of condyles were 19 (0.31%) and 25 (0.29%), respectively. No statistically significant differences were found between asymptomatic and symptomatic patients, between female and male patients, or between the right and left sides (p>0.05). Compared with the normally shaped condyle side, the BMC side showed no statistically significant differences in the distribution of pain and noise, parasagittal condylar position, or condylar osseous changes, with the exception of osteophytes. In the symptomatic group, osteophytes were found more frequently on the normally shaped condyle side than the BMC side (p<0.05).
A bifid mandibular condyle (BMC) is a rare anomaly, first described by Hrdlička in 1941.1 BMCs are usually asymptomatic and generally discovered as an incidental finding during routine radiographic examinations.2-4 With the use of advanced imaging modalities such as computed tomography (CT), cone-beam computed tomography (CBCT), and magnetic resonance imaging (MRI), there has been an increase in the number of cases reported. Its incidence has been reported to be from 0.018% to 1.82%.4-7 Its morphology varies from grooving to two discrete condylar heads, oriented mediolaterally or anteroposteriorly.2,4
Although the exact etiology of BMCs is not yet fully understood, trauma and developmental factors have been considered to be the two major possible etiologies.2,7 Vascular, nutritional, endocrinal, teratogenic, or infectious causes of this malformation have also been proposed.4,8,9 Excluding known traumatic causes, the incidence and clinical significance of BMC regarded as having a developmental origin should be investigated.
This study was performed to assess the prevalence of BMCs using CBCT images and to evaluate their impact on the clinical and radiographic features of temporomandibular joint (TMJ).
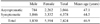
We retrospectively reviewed CBCT images of 3,046 asymptomatic and 4,378 symptomatic TMJ patients over the age of 16, assuming that the mandibular condyle has completed its development by age 16 years (Table 1). The symptomatic group consisted of patients complaining of the clinical signs and symptoms of TMJ.
Clinical examinations were performed to assess the presence of TMJ pain and noise. TMJ pain was assessed by asking the patients if they felt either joint or muscle pain during mandibular function. TMJ noise was based on either crepitation or clicking sounds. The asymptomatic group consisted of the patients with no TMJ signs and symptoms. Most of the asymptomatic patients had undergone CBCT scans either for a thorough examination of tooth impaction or an orthodontic evaluation. In both groups, the patients who had a traumatic history related to TMJ and any conditions that could affect TMJ components, such as skeletal abnormalities, TMJ tumors, or other infectious diseases were excluded.
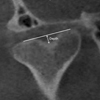
CBCT scans had been obtained with a PaX-Zenith3D (Vatech, Yongin, Korea) in the maximal intercuspal position with a field of view of 24 cm×19 cm. Real-time reconstruction was performed using an Ez3D 2009 3D image viewer (Vatech, Yongin, Korea) and the acquired image data consisted of a 14-bit scale with a 0.3mm3 voxel size. Mediolateral bifidity was assessed using coronal images parallel to the long axis of the condyle, and anteroposterior bifidity was assessed using lateral images perpendicular to the long axis of the condyle. The BMC depth was measured by the shortest distance from the line connecting the two highest points of the condyles to the lowest point of the condyles (Fig. 1). The osseous changes and parasagittal positioning of the condyles were evaluated by using the same method performed in a previous study.10 Two experienced oral and maxillofacial radiologists assessed the images together and their concordant results were used for analysis.
The differences in prevalence between the asymptomatic and symptomatic groups, between male and female patients, and between right and left sides were assessed by a t-test. In the BMC patients, comparisons were carried out using chi-squared tests to evaluate the differences between the normally shaped condyle and BMC sides with regard to the clinical features of pain and noise, osseous changes of flattening, sclerosis, osteophytes, and erosion, as well as the parasagittal positions of the condyles. The level of statistical significance was set at 0.05. The analyses were performed with PASW Statistics version 18 software (SPSS Inc., Chicago, IL, USA).
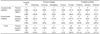
Table 2 shows the BMC distribution. Among the 7,424 patients, 37 (0.50%) patients were found to have BMC: 15 (0.49%) patients in the asymptomatic group and 22 (0.50%) patients in the symptomatic group. Among these 37 patients, 30 (81.1%) patients had unilateral BMC and 7 (18.9%) patients had bilateral BMC; therefore, in total, 44 BMCs and 30 normal condyles were found in 37 patients. All of the BMCs showed a mediolateral orientation and seven of them appeared to have anteroposterior bifidity as well (Figs. 2 and 3). The mean depth of the BMC was 2.3 mm in the asymptomatic group and 2.7 mm in the symptomatic group. There was no statistically significant difference in the prevalence of the asymptomatic and symptomatic groups. Gender and side also showed no significant differences (p>0.05).
In the 37 patients with BMCs, there were 22 symptomatic patients who had pain and/or noise and 15 asymptomatic patients. In the 44 mandibular condyles of the symptomatic patients, pain occurred in 11 normal condyles and 14 BMCs, and TMJ noise in 9 normal condyles and 8 BMCs. There was no statistically significant difference in pain and noise in the symptomatic group between the normally shaped condyles and BMCs (p>0.05).
Bone changes of the condyles were present in 33.3% of asymptomatic and in 40.9% of symptomatic patients. For osseous changes and parasagittal positioning of the condyles, there were no significant differences between the normally shaped condyle and BMC sides in both asymptomatic and symptomatic groups with one exception. In the symptomatic group, osteophytes were more frequently observed in the normally shaped condyle side than the BMC side (p<0.05) (Table 3).
BMC is an uncommon anomaly, characterized by a division of the mandibular condylar head. This study examined a population consisting of both asymptomatic and symptomatic subjects to assess the impact of BMC on clinical and radiographic findings of TMJ and used CBCT as an imaging tool to prevent misinterpretation. CBCT is an excellent imaging modality for the assessment of BMC. It allows detailed visualization of condylar morphology without osseous superimposition. On the other hand, panoramic radiographs can misread bifidity by the overlapping of anatomical structures or inherent image distortion.2,4 They can either under- or overestimate bifidity.
Several epidemiological studies have been carried out on living subjects. Menezes et al4 found only nine (0.018%) cases of BMC from 50,080 panoramic radiographs in a Brazilian population. However, Miloglu et al2 and Sahman et al6 examined panoramic radiographs in Turkish subjects and reported the prevalence of BMC as 0.31% and 0.52%, respectively. In 2012, Sahman et al5 performed a retrospective study using CT records of 550 patients and found BMCs in 10 patients (1.82%). Our study presented 37 (0.50%) cases of BMC from 7,424 subjects, in total, 44 BMCs (0.30%) from 14,848 condyles. The prevalence in the symptomatic group did not differ from that of the asymptomatic group, from which we assumed that BMC might not cause TMJ disorder and that it was just a coincidental finding.
The prevalence of BMCs in this study was quite similar to that in the panoramic study by Sahman et al6 which reported 0.52% of patients with BMC and 0.33% of condyles with BMC. Szentpétery et al7 investigated skulls and reported a similar incidence rate of 0.34% in 2,077 condyles. Sahman et al5 speculated that BMC might be a more frequent condition in the Turkish population. They also stated that the difference between CT-based and panoramic image-based studies in the same Turkish population might have occurred from misinterpretations of the panoramic radiographs. The discrepancies could reflect the diversity of imaging modalities, race, and sample size.
Although Dennison et al11 considered only the anteroposterior division of a condyle to be a "true" bifid condyle, BMC has been generally regarded as when a condyle appears to be duplicated either anteroposteriorly or mediolaterally. In our study, all BMCs were mediolaterally oriented, and among them, seven condyles showed anteroposterior bifidity as well. Considering the fact that no condyle solely showed anteroposterior bifidity, it was presumed that anteroposterior bifidity in this study presented as a concomitant of mediolateral orientation. In our cases, BMCs having a groove only presented mediolateral bifidity and BMCs having a central pit on the top of the condyle showed both mediolateral and anteroposterior bifidity (Figs. 2 and 3). Shriki et al12 proposed the hypothesis that a bifid condyle with mediolateral heads was a developmental phenomenon rather than based on trauma, and our results also supported their claim. Many studies have reported that most patients showing mediolateral bifidity had no traumatic history,12-16 although Melo et al17 reported a very rare case of a nontraumatic anteroposterior bifid condyle. In connection with BMC orientation, it has been suggested that a sagittal split with anteroposterior orientation was associated with a traumatic event.7,12,13,18,19 However, other authors have demonstrated that fractures of the mandibular condyle could result in mediolateral as well as anteroposterior BMCs.20-22
Unilateral BMCs have been found about four times as often as the bilateral form,1,2,4,5,11,23 and our study, accounting for 81.1% of BMCs as unilateral, was also consistent with these findings.
A review of the literature supported the notion that the occurrence of BMC showed no predilection for gender.2,5,6,23 Although our study revealed a significantly higher femalemale ratio of 3.1 : 1, it was caused by a substantial difference in the number of males and females in the sample. The prevalence was 0.49% for males and 0.50% for females, and there was no statistically significant difference between female and male prevalence (p>0.05).
In the literature, the majority of studies have reported that BMCs involve the left side more often than the right side,2,4,6,11,23 while Miloglu et al2 presented a predilection for the right side. We found a higher frequency of BMCs in the left than in the right side, but there was no statistically significant difference (p>0.05), which was in agreement with the survey of Sahman et al.6
In most nontraumatic cases, clinical symptoms were absent,2,4,6,13-15,24 and BMC was usually discovered as an incidental radiological finding. On the other hand, a few studies reported BMC patients complaining of TMJ clicking, limited mouth opening, and pain.5,23,25,26 Our study showed no significant differences in the distribution of clinical symptoms between normally shaped condyles and BMC sides (p>0.05), which meant that BMC was not provoking any TMJ symptoms.
In this survey, flattening was the predominant finding, which was in agreement with the result of dos Anjos Pontual et al.27 Flattening was more common on the BMCs than the normally shaped condyles, even though there was no significant difference (p>0.05). The only statistically significant difference between normally shaped condyles and BMC sides was found in the number of osteophytes of symptomatic patients. Interestingly, the normally shaped condyles had more osteophytes than the BMCs (Table 3). We speculated that the high prevalence of flattening and the low prevalence of osteophytes on the BMC side might be attributed to the morphological features of BMCs. Grooving tended to make the condyle flat and lack the potential to form osteophytes.
The asymptomatic group showed an almost randomly distributed condylar position in the glenoid fossa, while in the symptomatic group, a retruded position was relatively common. However, there were no significant differences between the condylar position of the normally shaped condyle and BMC sides (p>0.05). McCormick et al28 stated that bifidism might lead to TMJ syndrome in some patients, but our study revealed no evidence to support this claim.
In conclusion, BMCs are generally identified as an incidental finding during radiographic examination, and with the widespread use of advanced imaging modalities, they are now more commonly detected. Our results demonstrated that BMCs had no predilection for gender or side, and they had no relationship with the clinical and radiographic manifestations of TMJ in general.
Figures and Tables
Fig. 2
Condyle presenting mediolateral bifidity. A. Coronal image parallel to the long axis of the condyle. B. Lateral image perpendicular to the long axis of the condyle. C. Coronal image of the 3D reconstructed condyle. D. Lateral image of the 3D reconstructed condyle.
Fig. 3
Condyle presenting mediolateral and anteroposterior bifidity. A. Coronal image parallel to the long axis of the condyle. B. Lateral image perpendicular to the long axis of the condyle. C. Coronal image of the 3D reconstructed condyle. D. Lateral image of the 3D reconstructed condyle. E. Aeroview shows a central pit (arrow).

References
2. Miloglu O, Yalcin E, Buyukkurt M, Yilmaz A, Harorli A. The frequency of bifid mandibular condyle in a Turkish patient population. Dentomaxillofac Radiol. 2010. 39:42–46.

3. Espinosa-Femenia M, Sartorres-Nieto M, Berini-Aytés L, Gay-Escoda C. Bilateral bifid mandibular condyle: Case report and literature review. Cranio. 2006. 24:137–140.

4. Menezes AV, de Moraes Ramos FM, de Vasconcelos-Filho JO, Kurita LM, de Almeida SM, Haiter-Neto F. The prevalence of bifid mandibular condyle detected in a Brazilian population. Dentomaxillofac Radiol. 2008. 37:220–223.

5. Sahman H, Sisman Y, Sekerci AE, Tarim-Ertas E, Tokmak T, Tuna IS. Detection of bifid mandibular condyle using computed tomography. Med Oral Patol Oral Cir Bucal. 2012. 17:e930–e934.

6. Sahman H, Sekerci AE, Ertas ET, Etoz M, Sisman Y. Prevalence of bifid mandibular condyle in a Turkish population. J Oral Sci. 2011. 53:433–437.

7. Szentpétery A, Kocsis G, Marcsik A. The problem of the bifid mandibular condyle. J Oral Maxillofac Surg. 1990. 48:1254–1257.

8. Gundlach KK, Fuhrmann A, Beckmann-Van der Ven G. The double-headed mandibular condyle. Oral Surg Oral Med Oral Pathol. 1987. 64:249–253.

9. Quayle AA, Adams JE. Supplemental mandibular condyle. Br J Oral Maxillofac Surg. 1986. 24:349–356.
10. Cho BH, Jung YH. Osteoarthritic changes and condylar positioning of the temporomandibular joint in Korean children and adolescents. Imaging Sci Dent. 2012. 42:169–174.

11. Dennison J, Mahoney P, Herbison P, Dias G. The false and the true bifid condyles. Homo. 2008. 59:149–159.

12. Shriki J, Lev R, Wong BF, Sundine MJ, Hasso AN. Bifid mandibular condyle: CT and MR imaging appearance in two patients: case report and review of the literature. AJNR Am J Neuroradiol. 2005. 26:1865–1868.
13. Plevnia JR, Smith JA, Stone CG. Bifid mandibular condyle without history of trauma or pain: report of a case. J Oral Maxillofac Surg. 2009. 67:1555–1561.

14. Ramos FM, Filho JO, Manzi FR, Bóscolo FN, Almeida SM. Bifid mandibular condyle: a case report. J Oral Sci. 2006. 48:35–37.

16. Stefanou EP, Fanourakis IG, Vlastos K, Katerelou J. Bilateral bifid mandibular condyles. Report of four cases. Dentomaxillofac Radiol. 1998. 27:186–188.

17. Melo SL, Melo DP, Oenning AC, Haiter-Neto F, Almeida SM, Campos PS. Magnetic resonance imaging findings of true bifid mandibular condyle with duplicated mandibular fossa. Clin Anat. 2012. 25:650–655.

18. Forman GH, Smith NJ. Bifid mandibular condyle. Oral Surg Oral Med Oral Pathol. 1984. 57:371–373.

19. Balciunas BA. Bifid mandibular condyle. J Oral Maxillofac Surg. 1986. 44:324–325.
20. Yao J, Zhou J, Hu M. Comparative experimental study between longitudinal fracture and transverse fracture of mandibular condyle. Zhonghua Kou Qiang Yi Xue Za Zhi. 1999. 34:178–180.
21. Li Z, Djae KA, Li ZB. Post-traumatic bifid condyle: the pathogenesis analysis. Dent Traumatol. 2011. 27:452–454.

22. Antoniades K, Hadjipetrou L, Antoniades V, Paraskevopoulos K. Bilateral bifid mandibular condyle. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004. 97:535–538.

24. Alpaslan S, Ozbek M, Hersek N, Kanli A, Avcu N, Firat M. Bilateral bifid mandibular condyle. Dentomaxillofac Radiol. 2004. 33:274–277.

25. Almasan OC, Hedesiu M, Baciut G, Baciut M, Bran S, Jacobs R. Nontraumatic bilateral bifid condyle and intermittent joint lock: a case report and literature review. J Oral Maxillofac Surg. 2011. 69:e297–e303.
26. Corchero-Martín G, Gonzalez-Terán T, García-Reija MF, Sánchez-Santolino S, Saiz-Bustillo R. Bifid condyle: case report. Med Oral Patol Oral Cir Bucal. 2005. 10:277–279.
27. dos Anjos Pontual ML, Freire JS, Barbosa JM, Frazão MA, dos Anjos Pontual A. Evaluation of bone changes in the temporomandibular joint using cone beam CT. Dentomaxillofac Radiol. 2012. 41:24–29.

28. McCormick SU, McCormick SA, Graves RW, Pifer RG. Bilateral bifid mandibular condyles. Report of three cases. Oral Surg Oral Med Oral Pathol. 1989. 68:555–557.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download