Abstract
Purpose
This study was performed to evaluate the relationship between anterior disc displacement and effusion in temporomandibular disorder (TMD) patients using magnetic resonance imaging (MRI).
Materials and Methods
The study subjects included 253 TMD patients. MRI examinations were performed using a 1.5 T MRI scanner. T1- and T2-weighted images with para-sagittal and para-coronal images were obtained. According to the MRI findings, temporomandibular joint (TMJ) disc positions were divided into 3 subgroups: normal, anterior disc displacement with reduction (DWR), and anterior disc displacement without reduction (DWOR). The cases of effusion were divided into 4 groups: normal, mild (E1), moderate (E2), and marked effusion (E3). Statistical analysis was made by the Fisher's exact test using SPSS (version 12.0, SPSS Inc., Chicago, IL, USA).
Results
The subjects consisted of 62 males and 191 females with a mean age of 28.5 years. Of the 253 patients, T1- and T2-weighted images revealed 34 (13.4%) normal, DWR in 103 (40.7%), and DWOR in 116 (45.9%) on the right side and 37 (14.6%) normal, DWR in 94 (37.2%), and DWOR in 122 (48.2%) joints on the left side. Also, T2-images revealed 82 (32.4%) normal, 78 (30.8%) E1, 51 (20.2%) E2, and 42 (16.6%) E3 joints on the right side and 79 (31.2%) normal, 85 (33.6%) E1, 57 (22.5%) E2, and 32 (12.7%) E3 on the left side. There was no difference between the right and left side.
Magnetic resonance imaging (MRI) of the temporomandibular joint (TMJ) has been accepted as the best method for making a diagnostic assessment of TMJ status.1-3
Internal derangement (ID) of the TMJ is when the disc is located outside of its normal position in the joint spaces. The normal disc position means a 12 o'clock position of the posterior band and a 10 o'clock position of the intermediate zone of the disc. The disc has a "bow tie" shape with a thin intermediate zone with the narrowest inter-bony distance.2 Displacement of the disc can present along a spectrum of displacements in any direction, but anterior disc displacement is most common.
Larheim3 and Larheim et al4 reported that the TMJ disc position seemed to be different in temporomandibular disorder (TMD) patients and asymptomatic volunteers. Disc displacement without reduction (DWOR) was found to be frequent in TMD patients; however, it was very rare in asymptomatic volunteers.
Disc displacement with or without reduction of the TMJ is an intracapsular dysfunction that leads to degenerative changes in the disc and articular surface.5 TMJ dysfunction may be either a progressive disorder or one that resolves spontaneously. Initially, patients present with symptoms of clicking or popping, which is the result of anterior disc displacement with reduction (DWR). As the disease progresses, the posterior attachment becomes stretched and the disc is no longer recaptured on mouth opening. ID may eventually result in degenerative changes to the TMJ.2
Deformation of the disc is frequently found in non-reducing conditions, and the normal biconcave configuration seems to change as a result of the displacement.6 Deformations of the disc such as a thick posterior band, a folded shape, and particularly the later biconvex deformation, can be clearly seen in MRI.
Yano et al7 reported that effusion is the state of accumulation of joint fluid in the joint spaces and surrounding tissue. Joint effusion is defined in MRI as bright T2 signals in articular spaces, whereas the disc of a normal TMJ has relatively low signal intensity.
Various articles7-10 have reported ID or effusion in TMJ; however, Koh et al11 noted that a variety of diagnostic criteria have been used, and the relationship between ID and effusion is still unclear.
This study was performed to evaluate the relationship between ID and effusion in TMD patients using MRI.
The study subjects included 253 TMD patients (506 TMJs) who had visited Chonbuk National University Dental Hospital with signs and symptoms of ID from 2008 to 2012.
MRI examinations were performed using a 1.5 T MRI scanner (Symphony, Siemens, Olangan, Germany) with a 7.5-cm surface coil. A 3-mm section thickness with a 140 mm×140 mm field of view (FOV) and spin echo (SE) multisection images were used for the T1-weighted images (T1WIs: repetition time (RT) ms/echo time (TE) ms=510-520/11-15) and T2-weighted images (T2WIs: TR/TE=2410-2740/40-107). Eighteen para-coronal and 11 parasagittal images were obtained. According to the MRI findings, the TMJ disc positions were classified into the 3 subgroups of normal (Fig. 1A), DWR (Fig. 1B), and DWOR (Fig. 1C) on the T1WIs and T2WIs. Here, DWR and DWOR included antero-medial and antero-lateral displacement. The disc position classifications were defined as follows:
Normal: The posterior band of the disc was located above the apex of the condylar head (at the 12 o'clock position) in the closed mouth position as described by Styles and Whyte2 and the thin intermediate zone was between the condyle and the articular eminence with the mouth opened 1 inch.
DWR: The posterior band of the disc was located anteriorly to the condylar head in the closed position, but with a normal disc-condyle relationship with the mouth opened 1 inch.
DWOR: The posterior band was positioned anteriorly to the condyle both with the mouth closed and opened 1 inch.
The shape of each disc was classified as biconcave, biconvex, folded, lengthened, or a thick posterior band shape. Round configurations were classified as biconvex.
The degree of effusion was determined as described by Larheim et al,4 but TMJ effusions were classified into 4 subgroups of normal, mild effusion (E1), moderate effusion (E2), and marked effusion (E3) on T2WIs. The specifications for the classification of TMJ effusions are as follows:
Mild effusion: a dot or line of bright signal intensity along the articular surface as described by Westesson and Brooks9 (Fig. 2A)
Moderate effusion: between mild and marked signal intensity (Fig. 2B)
Marked effusion: collection with pooling in the joint space (Fig. 2C)
Evaluations of MR images were performed at different points in time by two experienced oral and maxillofacial radiologists. When there was disagreement, the final assessment was reached by consensus.
Statistical analysis was made by the Fisher's exact test using SPSS version 12.0 (SPSS Inc., Chicago, IL, USA). All of the P-values <0.05 in the comparison of ID and effusion were considered statistically significant.
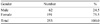
Table 1 shows the gender distribution of the study subjects. The subjects consisted of 62 males (24.5%) and 191 females (75.5%). The ratio between the males and females was 0.3. Table 2 shows the age distribution of the study subjects. Of the 253 TMD patients, the second and third decades were predominant (67.6%). The mean age was 28.5 years, with a range of 13 to 78 years.
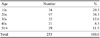
Table 3 shows the distribution of anterior disc displacement according to the site. All of the patients had a unilateral or bilateral TMJ disc ID. Of the 253 right TMJ discs examined, T1WIs and T2WIs revealed normal cases in 34 (13.4%), DWR in 103 (40.7%), and DWOR in 116 (45.9%) of the discs. Of the 253 left TMJ discs examined, T1WIs and T2WIs revealed normal cases in 37 (14.6%), DWR in 94 (37.2%), and DWOR in 122 (48.2%) of the discs. There was no difference between the right and left sides.
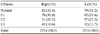
Table 4 shows the disc configuration of the TMJ. Deformity of the disc was found in 163 of 506 (32.2%) TMJ discs. There were 343 (67.8%) discs with no deformity, whereas 62 (12.2%) of the discs were biconvex, 52 (10.3%) were folded, 35 (6.9%) were lengthened, and 14 (2.8%) were thick posterior bands. Folded and biconvex configurations were more common in cases of DWR and DWOR.
Table 5 shows the distribution of effusion according to the site. Of the 253 right TMJs, T2WIs revealed normal cases in 82 (32.4%), E1 in 78 (30.8%), E2 in 51 (20.2%), and E3 in 42 (16.6%) joints, respectively. Of the 253 left TMJs, T2WIs revealed normal cases in 79 (31.2%), E1 in 85 (33.6%), E2 in 57 (22.5%), and E3 in 32 (12.7%) joints, respectively. There was no difference between the right and left side. Anterior disc displacement with/without reduction was not significantly related to effusion in the TMD patients (P>0.05) (Table 6, 7).
MRI has the advantage of displaying both soft and hard tissue changes in the TMJ, and clearly shows the shape of the disc. Many MRI studies have reported that about 80% of patients referred for diagnostic imaging of the TMJ will have an imaging diagnosis of disc displacement.1,3,4,12 However, MRI results can be influenced by such factors as MRI technique, imaging protocol, diagnostic criteria, and observer performance.11 In this study, the MRI protocol consisted of a 1.5 T field strength, TMJ coil, T1WIs and T2WIs, and para-saggital and para-coronal images. Therefore, the protocol probably had a minimal effect on the results.
On the other hand, diagnostic criteria used for the disc position on the MRI have varied. Some studies1,9,13 have used previously presented criteria, whereas several other studies have used their own classification systems.12,14-17 In this study, according to the diagnostic criteria as described by Styles and Whyte,2 76% of TMD patients had ID bilaterally, and there was no difference between the right and left side.
An alteration in disc shape has been recognized as an important feature of ID of the TMJ, and the disc deformation appears to occur secondary to disc displacement. Deformation most commonly begins with thickening and enlargement of the posterior band of the disc.18 Using MRI, Taşkaya-Yilmaz and Oğütcen-Toller5 categorized the disc configuration as biconcave (normal), folded, lengthened, round, biconvex, and thickened posterior band. Disc deformation associated with disc displacement appears more frequently with a greater degree of displacement such as disc displacement without reduction. Helms et al reported that 17% of joints that had anteriorly displaced discs with reduction had degenerative joint disease, whereas 95% of joints with displaced discs without reduction had degenerative changes.19 An MRI can be used to visualize the morphology of the disc in order to grade the severity of the ID.
In this study, round shapes were classified as biconvex, and folded and biconvex configurations were more common in cases of DWR and DWOR. Therefore, it seemed that many TMD patients had disc displacement in an advanced stage.
The differing definitions used for joint effusion in several studies9,20-23 might have affected their results. Larheim et al4 reported that there was a need to define what was an abnormal amount of fluid because TMJ fluid was frequently observed in asymptomatic volunteers as well and was related to the disc displacement. Therefore, Larheim et al4 classified joint effusion as moderate or marked. They reported that almost all of the TMD patients (96%) had ID, mostly bilateral (80%). The joint effusion was predominantly unilateral (61.4%). However, in this study, the degree of effusion was classified into three groups-minimal, moderate, or marked, and 44% of the TMD patients had bilateral effusion. Murakami et al24 reported that the quantity and quality of effusion varied according to the changes in the TMJ. Suenaga et al25 demonstrated that the change in the amount of effusion could be detected through biochemical analysis of the joint fluid.
Various studies concerning the relationship between ID and joint effusion have been performed.4,7-9 Effusion is frequently observed on MRI in patients with ID of the TMJ.4,9,20,22,26 Larheim et al4 demonstrated that moderate and marked fluid was related to disc displacement. Manfredini et al27 reported that joint effusion was related to disc displacement without reduction. Huh et al28 suggested that the effusion-disc displacement association might become evident at more advanced stages of disc displacement, thus representing an indicator of the progression of the disease to a more chronic condition. Tasaki et al1 reported that the disc displacement was observed unilaterally or bilaterally in 82% of the TMD patients and in 30% of the asymptomatic volunteers. Yano et al7 reported that no significant difference was observed between the quantity of joint fluid and the grade of disc displacement, although even a minimal amount of fluid was regarded as being positive for fluid in that study. In this study, ID was not related to joint effusion in the TMD patients.
Observer performance greatly influences MRI diagnosis of disc position and joint effusion.29 In this study, observations were performed by two experienced oral and maxillofacial radiologists for the minimization of inter-observer variation.
The results of this study suggested that ID with/without reduction was not related to the MRI findings of effusion in TMD patients. Further research will be required to determine the relationship between clinical findings and effusion on MRI.
Figures and Tables
 | Fig. 1Magnetic resonance images show the TMJ disc positions. A. Normal: The posterior band of the disc is located above the apex of the condylar head (at the 12 o'clock position) with the mouth closed (top) and with the mouth opened 1 inch (bottom). B. Disc displacement with reduction (DWR): The posterior band of the disc is located anteriorly to the condylar head with the mouth closed (top), but has a normal disc-condyle relationship with the mouth opened 1 inch (bottom). C. Disc displacement without reduction (DWOR): The posterior band is positioned anterior to the condyle both with the mouth closed (top) and with the mouth opened 1 inch (bottom). |
 | Fig. 2T2-weighted magnetic resonance images show effusion in the joint spaces. A. Mild effusion: a dot or line of bright signal intensity along the articular surface. B. Moderate effusion: between mild and marked effusion. C. Marked effusion: collection with pooling in the joint space. |
Table 6
Results of statistical analysis of the relationship between anterior disc displacement with/without reduction and effusion on the right temporomandibular joint

References
1. Tasaki MM, Westesson PL, Isberg AM, Ren YF, Tallents RH. Classification and prevalence of temporomandibular joint disk displacement in patients and symptom-free volunteers. Am J Orthod Dentofacial Orthop. 1996; 109:249–262.

2. Styles C, Whyte A. MRI in the assessment of internal derangement and pain within the temporomandibular joint: a pictorial essay. Br J Oral Maxillofac Surg. 2002; 40:220–228.

3. Larheim TA. Role of magnetic resonance imaging in the clinical diagnosis of the temporomandibular joint. Cells Tissues Organs. 2005; 180:6–21.

4. Larheim TA, Westesson P, Sano T. Temporomandibular joint disk displacement: comparison in asymptomatic volunteers and patients. Radiology. 2001; 218:428–432.

5. Taşkaya-Yilmaz N, Oğütcen-Toller M. Magnetic resonance imaging evaluation of temporomandibular joint disc deformities in relation to type of disc displacement. J Oral Maxillofac Surg. 2001; 59:860–866.
6. Westesson PL, Bronstein SL, Liedberg J. Internal derangement of the temporomandibular joint: morphologic description with correlation to joint function. Oral Surg Oral Med Oral Pathol. 1985; 59:323–331.

7. Yano K, Sano T, Okano T. A longitudinal study of magnetic resonance (MR) evidence of temporomandibular joint (TMJ) fluid in patients with TMJ disorders. Cranio. 2004; 22:64–71.

8. Schellhas KP, Wilkes CH. Temporomandibular joint inflammation: comparison of MR fast scanning with T1- and T2-weighted imaging techniques. AJR Am J Roentgenol. 1989; 153:93–98.

9. Westesson PL, Brooks SL. Temporomandibular joint: relationship between MR evidence of effusion and the presence of pain and disk displacement. AJR Am J Roentgenol. 1992; 159:559–563.

10. Larheim TA, Katzberg RW, Westesson PL, Tallents RH, Moss ME. MR evidence of temporomandibular joint fluid and condyle marrow alterations: occurrence in asymptomatic volunteers and symptomatic patients. Int J Oral Maxillofac Surg. 2001; 30:113–117.

11. Koh KJ, List T, Petersson A, Rohlin M. Relationship between clinical and magnetic resonance imaging diagnoses and findings in degenerative and inflammatory temporomandibular joint disease: a systematic literature review. J Orofac Pain. 2009; 23:123–139.
12. Paesani D, Westesson PL, Hatala MP, Tallents RH, Brooks SL. Accuracy of clinical diagnosis for TMJ internal derangement and arthrosis. Oral Surg Oral Med Oral Pathol. 1992; 73:360–363.

13. Drace JE, Enzmann DR. Defining the normal temporomandibular joint: closed-, partially open-, and open-mouth MR imaging of asymptomatic subjects. Radiology. 1990; 177:67–71.

14. Huddleston Slater JJ, Lobbezoo F, Chen YJ, Naeije M. A comparative study between clinical and instrumental methods for the recognition of internal derangements with a clicking sound on condylar movement. J Orofac Pain. 2004; 18:138–147.
15. Usumez S, Oz F, Guray E. Comparison of clinical and magnetic resonance imaging diagnoses in patients with TMD history. J Oral Rehabil. 2004; 31:52–56.
16. Katzberg RW, Westesson PL, Tallents RH, Drake CM. Anatomic disorders of the temporomandibular joint disc in asymptomatic subjects. J Oral Maxillofac Surg. 1996; 54:147–155.

17. Orsini MG, Kuboki T, Terada S, Matsuka Y, Yatani H, Yamashita A. Clinical predictability of temporomandibular joint disc displacement. J Dent Res. 1999; 78:650–660.

18. Katzberg RW, Tallents RH. Normal and abnormal temporomandibular joint disc and posterior attachment as depicted by magnetic resonance imaging in symptomatic and asymptomatic subjects. J Oral Maxillofac Surg. 2005; 63:1155–1161.

19. Helms CA, Kaban LB, McNeill C, Dodson T. Temporomandibular joint: morphology and signal intensity characteristics of the disk at MR imaging. Radiology. 1989; 172:817–820.

20. Adame CG, Monje F, Offnoz M, Martin-Granizo R. Effusion in magnetic resonance imaging of the temporomandibular joint: a study of 123 joints. J Oral Maxillofac Surg. 1998; 56:314–318.

21. Güler N, Yatmaz PI, Ataoglu H, Emlik D, Uckan S. Temporomandibular internal derangement: correlation of MRI findings with clinical symptoms of pain and joint sounds in patients with bruxing behavior. Dentomaxillofac Radiol. 2003; 32:304–310.
22. Takahashi T, Nagai H, Seki H, Fukuda M. Relationship between joint effusion, joint pain, and protein levels in joint lavage fluid of patients with internal derangement and osteoarthritis of the temporomandibular joint. J Oral Maxillofac Surg. 1999; 57:1187–1194.

23. Haley DP, Schiffman EL, Lindgren BR, Anderson Q, Andreasen K. The relationship between clinical and MRI findings in patients with unilateral temporomandibular joint pain. J Am Dent Assoc. 2001; 132:476–481.

24. Murakami K, Nishida M, Bessho K, Iizuka T, Tsuda Y, Konishi J. MRI evidence of high signal intensity and temporomandibular arthralgia and relating pain. Does the high signal correlate to the pain? Br J Oral Maxillofac Surg. 1996; 34:220–224.

25. Suenaga S, Abeyama K, Hamasaki A, Mimura T, Noikura T. Temporomandibular disorders: relationship between joint pain and effusion and nitric oxide concentration in the joint fluid. Dentomaxillofac Radiol. 2001; 30:214–218.

26. Rudisch A, Innerhofer K, Bertram S, Emshoff R. Magnetic resonance imaging findings of internal derangement and effusion in patients with unilateral temporomandibular joint pain. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001; 92:566–571.

27. Manfredini D, Basso D, Arboretti R, Guarda-Nardini L. Association between magnetic resonance signs of temporomandibular joint effusion and disk displacement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 107:266–271.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download