Abstract
Purpose
The purpose of this study was to determine the prevalence of missing and impacted third molars in people aged 25 years and above.
Materials and Methods
The study sample of 3,799 patients was chosen randomly from patients who visited Pusan National University Dental Hospital and had panoramic radiographs taken. The data collected included presence and impaction state, angulation, and depth of impaction of third molars, and radiographically detected lesions of third molars and adjacent second molars.
Results
A greater percentage of men than women retained at least one third molar. The incidence of third molars decreased with increasing age. The incidence of partially impacted third molars greatly declined after the age of 30. Vertically impacted maxillary third molars and horizontally impacted mandibular third molars were most frequent in all age groups. Among the maxillary third molars, those impacted below the cervical line of the second molar were most frequent in all age groups, and among the mandibular third molars, deeply impacted third molars were most frequent in those aged over 40. Dental caries was the most common radiographic lesion of the third molars. Mesioangularly impacted third molars showed radiographic lesions in 13 (9.5%) adjacent maxillary second molars and 117 (27.4%) mandibular second molars.
Conclusion
The number of remaining third molars decreased and the percentage of Class C depth increased with age. Caries was the most frequent lesion in third molars. Partially impacted mesioangular third molars showed a high incidence of caries or periodontal bone loss of the adjacent second molar. Regular oral examination will be essential to keep asymptomatic third molars in good health.
Surgical extraction of third molars is one of the most common surgical procedures in dentistry.1 Removal of a diseased or symptomatic third molar tooth reduces pain and symptoms and enhances patients' oral health and function.2
The National Institute of Clinical Excellence (NICE) introduced guidance on the extraction of wisdom teeth in 2000. This guideline recommended that the practice of prophylactic removal of pathology-free, impacted third molars should be discontinued and suggested indications for surgical extraction as follows: recurrent pericoronitis, cellulitis, abscess, osteomyelitis, disease of follicles including cysts and tumors, nonrestorable caries, untreatable pulpal and/or periapical pathology, internal/external resorption of adjacent teeth, tooth fracture, a tooth impeding surgery or reconstructive jaw surgery, and a tooth that is involved in or within the field of tumor resection.3
Prophylactic extraction of third molars should be based on an estimate of the balance between the risks and advantages of retained wisdom teeth because there is no reliable research to suggest that the removal of disease-free, impacted third molars is beneficial to patients and because unnecessary surgery exposes patients to risks.3,4 Surgical extraction of third molars is often accompanied by pain, swelling, bleeding, trismus, and general oral dysfunction during the healing phase; less commonly, nerve damage, damage to adjacent teeth, fracture of the mandible, and oroantral communication can occur.5
The size of the aging population is increasing. The average lifespan is expected to increase by another 10 years by 2050.6 Early removal of abnormal third molars could reduce the increased risk for complications in older patients.7 Since the introduction of the NICE guidelines, the average age has increased for third molar surgery, and surgery was less likely to be associated with impaction, and increasingly associated with other pathologies such as dental caries or pericoronitis.8 Ventä9 reported that one-fourth of retained and disease-free third molars needed to be removed preventively based on evidence, whereas the rest needed to be treated according to signs and symptoms.
The purpose of this study was to determine the eruption and impaction state of third molars in people aged 25 years and above by age group and investigate the prevalence of third molar loss and associated pathologies with age.
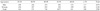
In this retrospective study, the study sample was chosen randomly from patients who visited Pusan National University Dental Hospital and underwent panoramic radiographic examination in 2011. The subject population comprised 3,799 patients aged 25 years and older (mean age 50.0 years, ranging from 25 to 92 years). Patients were distributed in groups as follows: 25-29 years; 30-39 years; 40-49 years; 50-59 years; 60-69 years; and over 70 years (Table 1). Patients with a history of trauma or pathology were not included in this study. All panoramic radiographs were taken with a Proline XC (Planmeca Co., Helsinki, Finland).
On panoramic radiographs, we examined the presence and impaction state of third molars, angulation and position of impacted third molars, and radiographic lesions of third molars and adjacent second molars. The remaining third molars present, as shown on the radiographs, were subclassified as erupted, partially impacted, or fully impacted. The angulation of the third molars was classified into vertical, mesioangular, horizontal, distoangular, buccolingual, or inverted using a modified Winter's classification.10,11 The position of the impacted third molars in relation to the occlusal plane was classified into Class A, B, or C by the Pell and Gregory system: Class A, the occlusal plane of the impacted tooth was at the same level as the adjacent tooth; Class B, the occlusal plane of the impacted tooth was between the occlusal plane and the cervical line of the adjacent tooth; Class C, the impacted tooth was apical to the cervical line of the adjacent molar.12
The radiographically detectable pathologic conditions of third molars and adjacent second molars were examined, including caries, retained root, periapical radiolucencies, alveolar bone loss, pericoronal radiolucencies, and supernumerary tooth in relation to third molars, and caries, bone loss of the distal aspect, and root resorption of the adjacent second molar.
A chi-squared test for statistical analysis was performed for the study data. P<0.05 was considered statistically significant. All analyses were carried out using IBM SPSS Statistics 21.0 (IBM, Armonk, NY, USA).
Maxillary and mandibular third molars from 3,799 patients were examined. At least one third molar was present in 2,048 (53.9%). A greater percentage of men compared to women retained at least one third molar, and this finding was statistically significant (P<0.001; Table 2). We found that 5,695 (75.0%) maxillary third molars and 5,046 (66.4%) mandibular third molars were missing, and older patients had fewer third molars. The percentage of partially impacted mandibular third molars in patients aged 30-39 years (19.2%) was much lower than for those aged 25-29 years (35.1%). The percentage of fully impacted mandibular third molars in people over 70 years (1.7%) was higher than in those aged 60-69 years (1.0%; Table 3).
The most frequent inclination was vertical impaction in maxillary third molars and horizontal impaction in mandibular third molars, followed by mesioangular impaction (Table 4). Distoangular maxillary third molars occurred in 33.3% and horizontal mandibular third molars in 64.3% of patients over 70 years of age (Table 5). When evaluating the impaction depth of third molars, most maxillary third molars were Class C in all age groups, whereas in mandibular third molars, Class C was more frequent than Class B only in patients over 40 years old (Table 6).
Lesions were detected radiographically in 135 (7.1%) maxillary third molars and 258 (10.1%) mandibular third molars. The most common radiographic lesion of the third molar was dental caries. Cyst formation was seen in one (0.1%) maxillary third molar and 23 (0.9%) mandibular third molars (Table 7).
Radiographic lesions of adjacent second molars were found in 13 (9.5%) of the mesioangular maxillary third molars and 117 (27.4%) of the mesioangular mandibular third molars. In erupted third molars, caries of second molars was most frequent, and in impacted third molars, bone loss of the distal aspect of adjacent second molars was most frequent. In mandibular third molars, 30 (9.3%) of the adjacent second molars showed caries with bone loss of the distal aspect (Table 8).
We examined the presence and impaction state of third molars and radiographic lesions of third or adjacent second molars. In a previous study, when offered the choice of retention or extraction, most patients (60%) with asymptomatic, disease-free third molars preferred extraction to retention.13 The frequency of remaining third molars showed a substantial reduction with increasing age in our study. It was obvious that some patients with asymptomatic third molars chose surgical extraction.
Greater surgical difficulty occurred in cases classified in the impaction depth Class C category and those with horizontal impaction.14,15 The percentage of horizontal mandibular third molars in patients older than 40 years was greater than the total average percentage in all ages. All impacted maxillary third molars were Class C for patients over 60 years, and all impacted mandibular third molars were Class C for patients over 70 years.
It has been reported that caries in erupted third molars increase in prevalence with increasing age.16 Patients over the age of 30 have been shown to be more likely to have third molar teeth removed due to caries than younger people.17-19 In our study, the incidence of radiographic lesions, including caries, increased with age, and the most frequently observed pathology was caries (5.4% of mandibular third molars). This prevalence was similar to that of a previous study20 but less than in other studies.21-23 We found the prevalence of periodontal bone loss to be 1.7% of mandibular third molars, and this prevalence was similar to a review by Mercier and Precious (1-4.5%)24 but less than that of a study by Polat et al (9.7%).20
Allen et al25 pointed out that disease or potential disease in the adjacent second molar teeth passed unnoticed in the NICE guidelines for surgical extraction of third molars. Mesioangular and horizontal mandibular third molars have been found to have a high risk of caries development and periodontal tissue damage at the second molar.26 Prophylactic removal of mesioangular and horizontal mandibular third molars has been suggested, especially for molars with an impaction depth of Class A.20 Risk factors for the development of caries in the second molar appeared to be erupted lower third molars and mesioangular impaction present for 4 to 5 years.17 In our results, mesioangularly impacted third molars showed pathologic lesions the most frequently. Caries of the second molar adjacent to the third molar was more frequent in erupted maxillary third molars and mesioangular mandibular third molars. Periodontal bone loss was more frequent than caries in the second molars adjacent to mesioangular third molars, and the prevalence of alveolar bone loss was relatively high in second molars adjacent to horizontal or inverted mandibular third molars. With careful monitoring, the development of lesions in adjacent second molars may be detected early, and a mesioangular or horizontal third molar associated with caries of the second molar should be removed and a restoration should be placed on the adjacent second molar.25 Oral hygiene instruction and preventive advice should be emphasized to patients with mesioangularly or horizontally impacted third molars.
Stathopoulos et al4 insisted that surgical removal of third molars should only be performed in the presence of specific indications because the incidence of cysts and tumors related to mandibular third molars was relatively low.4,27 In our results, cysts had rarely developed and most cysts were found in fully impacted third molars. However, the possibility of cystic changes associated with impacted third molars should be taken into consideration as an indication for the removal of asymptomatic impacted teeth.19
We found the prevalence of fully impacted third molars in patients over 60 years to be low (maxillary third molars, 3.6%; mandibular third molars, 2.7%). However, elderly patients requiring surgical removal of an impacted molar might have a medical problem.7 Surgical extraction in geriatric patients can be associated with increased risk of complications and more difficult postoperative recovery.28,29 In an aging population, impacted third molars may become visible due to periodontal bone loss and subsequent gingival recession.30,31 In our study, a small number of impacted mandibular third molars were exposed due to periodontal bone loss of adjacent teeth. A late erupted third molar might become infected in older patients. Prophylactic extraction of impacted third molars could be considered when it is difficult for patients to maintain good general health and oral hygiene.
Because there is no dependable way to predict pathologic changes associated with impacted teeth, they should be monitored regularly.16,32,33 Marciani34 suggested that patients who have decided to retain their third molars should have periodic clinical and radiographic examinations to detect disease before it becomes symptomatic. We consider a future study using a larger study group on why third molars are extracted to be necessary.
In conclusion, our data showed that about half of third molars were retained in patients under the age of 30 years, and the retention of third molars decreased with age. Vertical and horizontal impaction was most frequent in maxillary and mandibular third molars, respectively. Class C impaction depth was found in most of the patients over 40 years old. Caries was the most frequent lesion in third molars, and the prevalence of cyst changes was low. Partially impacted, mesioangular third molars showed a high incidence of caries or periodontal bone loss of the adjacent second molar. Regular oral examination is essential to keep asymptomatic third molars in good health.
Figures and Tables
Table 6
The depth of impacted third molars by age: number (percentage)
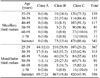
A: The occlusal plane of the impacted tooth is at the same level as the adjacent tooth. B: The occlusal plane of the impacted tooth is between the occlusal plane and the cervical line of the adjacent tooth. C: The occlusal plane of the impacted tooth is apical to the cervical line of the adjacent tooth.
References
1. McArdle LW, Renton T. The effects of NICE guidelines on the management of third molar teeth. Br Dent J. 2012; 213:E8.

2. Phillips C, Norman J, Jaskolka M, Blakey GH, Haug RH, Offenbacher S, et al. Changes over time in position and periodontal probing status of retained third molars. J Oral Maxillofac Surg. 2007; 65:2011–2017.

3. Technology appraisal guidance. No. 1. Guidance on the extraction of wisdom teeth [Internet]. London: National Institute for Clinical Excellence;2000. cited 2012 September 12. Available from: http://www.nice.org.uk/nicemedia/pdf/wisdomteethguidance.pdf.
4. Stathopoulos P, Mezitis M, Kappatos C, Titsinides S, Stylogianni E. Cysts and tumors associated with impacted third molars: is prophylactic removal justified? J Oral Maxillofac Surg. 2011; 69:405–408.

5. Susarla SM, Blaeser BF, Magalnick D. Third molar surgery and associated complications. Oral Maxillofac Surg Clin North Am. 2003; 15:177–186.

6. Centers for Disease Control and Prevention (CDC). Trends in aging - United States and worldwide. MMWR Morb Mortal Wkly Rep. 2003; 52:101–106.
7. Kaminishi RM, Lam PS, Kaminishi KS, Marshall MW, Hochwald DA. A 10-year comparative study of the incidence of third molar removal in the aging population. J Oral Maxillofac Surg. 2006; 64:173–174.

8. Renton T, Al-Haboubi M, Pau A, Shepherd J, Gallagher JE. What has been the United Kingdom's experience with retention of third molars? J Oral Maxillofac Surg. 2012; 70:S48–S57.

9. Ventä I. How often do asymptomatic, disease-free third molars need to be removed? J Oral Maxillofac Surg. 2012; 70:S41–S47.

10. Hashemipour MA, Tahmasbi-Arashlow M, Fahimi-Hanzaei F. Incidence of impacted mandibular and maxillary third molars: a radiographic study in a Southeast Iran population. Med Oral Patol Oral Cir Bucal. 2013; 18:e140–e145.
11. Almendros-Marqués N, Berini-Aytés L, Gay-Escoda C. Influence of lower third molar position on the incidence of preoperative complications. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006; 102:725–732.

12. Lima CJ, Silva LC, Melo MR, Santos JA, Santos TS. Evaluation of the agreement by examiners according to classifications of third molars. Med Oral Patol Oral Cir Bucal. 2012; 17:e281–e286.
13. Kinard BE, Dodson TB. Most patients with asymptomatic, disease-free third molars elect extraction over retention as their preferred treatment. J Oral Maxillofac Surg. 2010; 68:2935–2942.

14. Carvalho RW, do Egito Vasconcelos BC. Assessment of factors associated with surgical difficulty during removal of impacted lower third molars. J Oral Maxillofac Surg. 2011; 69:2714–2721.

15. Renton T, Smeeton N, McGurk M. Factors predictive of difficulty of mandibular third molar surgery. Br Dent J. 2001; 190:607–610.

16. American Association of Oral and Maxillofacial Surgeons. AAOMS white paper on third molar data [Internet]. Rosemont, IL: AAOMS;2007. cited 2012 September 12. Available from: http://www.aaoms.org/docs/third_molar_white_paper.pdf.
17. McArdle LW, Renton TF. Distal cervical caries in the mandibular second molar: an indication for the prophylactic removal of the third molar? Br J Oral Maxillofac Surg. 2006; 44:42–45.

18. Chang SW, Shin SY, Kum KY, Hong J. Correlation study between distal caries in the mandibular second molar and the eruption status of the mandibular third molar in the Korean population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 108:838–843.

19. Chu FC, Li TK, Lui VK, Newsome PR, Chow RL, Cheung LK. Prevalence of impacted teeth and associated pathologies -a radiographic study of the Hong Kong Chinese population. Hong Kong Med J. 2003; 9:158–163.
20. Polat HB, Ozan F, Kara I, Ozdemir H, Ay S. Prevalence of commonly found pathoses associated with mandibular impacted third molars based on panoramic radiographs in Turkish population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008; 105:e41–e47.

21. Punwutikorn J, Waikakul A, Ochareon P. Symptoms of unerupted mandibular third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999; 87:305–310.

22. Knutsson K, Brehmer B, Lysell L, Rohlin M. Asymptomatic mandibular third molars: oral surgeons' judgment of the need for extraction. J Oral Maxillofac Surg. 1992; 50:329–333.

23. Al-Khateeb TH, Bataineh AB. Pathology associated with impacted mandibular third molars in a group of Jordanians. J Oral Maxillofac Surg. 2006; 64:1598–1602.

24. Mercier P, Precious D. Risks and benefits of removal of impacted third molars. A critical review of the literature. Int J Oral Maxillofac Surg. 1992; 21:17–27.
25. Allen RT, Witherow H, Collyer J, Roper-Hall R, Nazir MA, Mathew G. The mesioangular third molar - to extract or not to extract? Analysis of 776 consecutive third molars. Br Dent J. 2009; 206:E23. discussion 586-7.

26. Falci SG, de Castro CR, Santos RC, de Souza Lima LD, Ramos-Jorge ML, Botelho AM, et al. Association between the presence of a partially erupted mandibular third molar and the existence of caries in the distal of the second molars. Int J Oral Maxillofac Surg. 2012; 41:1270–1274.

27. Eliasson S, Heimdahl A, Nordenram A. Pathological changes related to long-term impaction of third molars. A radiographic study. Int J Oral Maxillofac Surg. 1989; 18:210–212.
28. Chuang SK, Perrott DH, Susarla SM, Dodson TB. Age as a risk factor for third molar surgery complications. J Oral Maxillofac Surg. 2007; 65:1685–1692.

29. Phillips C, White RP Jr, Shugars DA, Zhou X. Risk factors associated with prolonged recovery and delayed healing after third molar surgery. J Oral Maxillofac Surg. 2003; 61:1436–1448.

30. Garcia RI, Chauncey HH. The eruption of third molars in adults: a 10-year longitudinal study. Oral Surg Oral Med Oral Pathol. 1989; 68:9–13.

31. Nance PE, White RP Jr, Offenbacher S, Phillips C, Blakey GH, Haug RH. Change in third molar angulation and position in young adults and follow-up periodontal pathology. J Oral Maxillofac Surg. 2006; 64:424–428.

32. Kahl B, Gerlach KL, Hilgers RD. A long-term, follow-up, radiographic evaluation of asymptomatic impacted third molars in orthodontically treated patients. Int J Oral Maxillofac Surg. 1994; 23:279–285.





 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download