1. Osteoporosis prevention, diagnosis and therapy. NIH Consensus Statement. 2000. 17:p. 1–45.
2. Johnell O, Kanis JA. An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos Int. 2004; 15:897–902.

3. Horner K, Devlin H. The relationship between mandibular bone mineral density and panoramic radiographic measurements. J Dent. 1998; 26:337–343.

4. Klemetti E, Kolmakov S, Kröger H. Pantomography in assessment of the osteoporosis risk group. Scand J Dent Res. 1994; 102:68–72.

5. Hildebolt CF. Osteoporosis and oral bone loss. Dentomaxillofac Radiol. 1997; 26:3–15.

6. White SC, Rudolph DJ. Alterations of the trabecular pattern of the jaws in patients with osteoporosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999; 88:628–635.

7. White SC, Taguchi A, Kao D, Wu S, Service SK, Yoon D, et al. Clinical and panoramic predictors of femur bone mineral density. Osteoporos Int. 2005; 16:339–346.

8. Devlin H, Karayianni K, Mitsea A, Jacobs R, Lindh C, van der Stelt P, et al. Diagnosing osteoporosis by using dental panoramic radiographs: the OSTEODENT project. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007; 104:821–828.

9. Arifin AZ, Asano A, Taguchi A, Nakamoto T, Ohtsuka M, Tsuda M, et al. Computer-aided system for measuring the mandibular cortical width on dental panoramic radiographs in identifying postmenopausal women with low bone mineral density. Osteoporos Int. 2006; 17:753–759.

10. Devlin H, Allen PD, Graham J, Jacobs R, Karayianni K, Lindh C, et al. Automated osteoporosis risk assessment by dentists: a new pathway to diagnosis. Bone. 2007; 40:835–842.

11. Allen PD, Graham J, Farnell DJ, Harrison EJ, Jacobs R, Nicopolou-Karayianni K, et al. Detecting reduced bone mineral density from dental radiographs using statistical shape models. IEEE Trans Inf Technol Biomed. 2007; 11:601–610.

12. Roberts M, Yuan J, Graham J, Jacobs R, Devlin H. Changes in mandibular cortical width measurements with age in men and women. Osteoporos Int. 2011; 22:1915–1925.

13. Kavitha MS, Samopa F, Asano A, Taguchi A, Sanada M. Computer-aided measurement of mandibular cortical width on dental panoramic radiographs for identifying osteoporosis. J Investig Clin Dent. 2012; 3:36–44.

14. Nakamoto T, Taguchi A, Ohtsuka M, Suei Y, Fujita M, Tanimoto K, et al. Dental panoramic radiograph as a tool to detect postmenopausal women with low bone mineral density: untrained general dental practitioners' diagnostic performance. Osteoporos Int. 2003; 14:659–664.
15. Lee K, Taguchi A, Ishii K, Suei Y, Fujita M, Nakamoto T, et al. Visual assessment of the mandibular cortex on panoramic radiographs to identify postmenopausal women with low bone mineral densities. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005; 100:226–231.

16. Taguchi A, Asano A, Ohtsuka M, Nakamoto T, Suei Y, Tsuda M, et al. Observer performance in diagnosing osteoporosis by dental panoramic radiographs: results from the osteoporosis screening project in dentistry (OSPD). Bone. 2008; 43:209–213.

17. World Health Organization. Assessment of fracture risk and its application to screening for postmenopausal women osteoporosis. Geneva: World Health Organization;1994.
18. Fujiwara S, Kasagi F, Masunari N, Naito K, Suzuki G, Fukunaga M. Fracture prediction from bone mineral density in Japanese men and women. J Bone Miner Res. 2003; 18:1547–1553.

19. Orimo H, Hayashi Y, Fukunaga M, Sone T, Fujiwara S, Shiraki M, et al. Diagnostic criteria for primary osteoporosis: year 2000 revision. J Bone Miner Metab. 2001; 19:331–337.

20. Gonzalez RC, Woods RE. Digital image processing. Englewood Cliffs: Addison-Wesley Pub;1992.
21. Ketchen DJ, Shook CL. The application of cluster analysis in strategic management research: an analysis and critique. Strat Mgmt J. 1996; 17:441–458.
22. Manning CD, Raghavan P, Schütze H. Introduction to information retrieval. New York: Cambridge University Press;2008.
23. Hartigan JA. Clustering algorithms: probability & mathematical statistics. New York: Wiley;1975.
24. Wee LJ, Tan TW, Ranganathan S. SVM-based prediction of caspase substrate cleavage sites. BMC Bioinformatics. 2006; 7:Suppl 5. S14.

25. Burges CJ. A tutorial on support vector machines for pattern recognition. Data Min Knowl Discov. 1998; 2:121–167.
26. Vapnik VN. The nature of statistical learning theory. New York: Springer;1995.
27. Vapnik VN. Statistical learning theory. New York: Wiley;1998.
28. Ciesielski K, Sacha JP, Cios K. Synthesis of feedforward networks in supremum error bound. IEEE Trans Neural Netw. 2000; 11:1213–1227.
29. Back AD, Chen T. Universal approximation of multiple nonlinear operators by neural networks. Neural Comput. 2002; 14:2561–2566.

30. Aleksander I, Morton H. An introduction to neural computing. London: Chapman and Hall;1990.
31. Schölkopf B, Smola AJ. Learning with kernels. Cambridge: MIT Press;2002.
32. Haykin S. Neural networks: a comprehensive foundation. 2nd ed. Englewood Cliffs: Prentice Hall;1999.
33. Karayianni K, Horner K, Mitsea A, Berkas L, Mastoris M, Jacobs R, et al. Accuracy in osteoporosis diagnosis of a combination of mandibular cortical width measurement on dental panoramic radiographs and a clinical risk index (OSIRIS): the OSTEODENT project. Bone. 2007; 40:223–229.

34. Tuceryan M, Jain AK. Texture analysis. In : Chen CH, Pau LF, Wang PS, editors. The handbook of pattern recognition and computer vision. Singapore: World Scientific Publishing Co.;1998. p. 207–248.
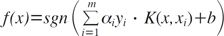
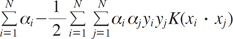
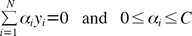
35. Kavitha MS, Asano A, Taguchi A, Kurita T, Sanada M. Diagnosis of osteoporosis from dental panoramic radiographs using the support vector machine method in a computer-aided system. BMC Med Imaging. 2012; 12:1.

36. Muramatsu C, Matsumoto T, Hayashi T, Hara T, Katsumata A, Zhou X, et al. Automated measurement of mandibular cortical width on dental panoramic radiographs. Int J Comput Assist Radiol Surg. 2000; (in press).

37. Yosue T, Brooks SL. The appearance of the mental foramina on panoramic and periapical radiographs. II. Experimental evaluation. Oral Surg Oral Med Oral Pathol. 1989; 68:488–492.




 PDF
PDF ePub
ePub Citation
Citation Print
Print











 XML Download
XML Download