Abstract
Purpose
This study was performed to evaluate and compare the radiopacity of dentin, enamel, and 8 restorative composites on conventional radiograph and digital images with different resolutions.
Materials and Methods
Specimens were fabricated from 8 materials and human molars were longitudinally sectioned 1.0 mm thick to include both enamel and dentin. The specimens and tooth sections were imaged by conventional radiograph using #4 sized intraoral film and digital images were taken in high speed and high resolution modes using a phosphor storage plate. Densitometric evaluation of the enamel, dentin, restorative materials, a lead sheet, and an aluminum step wedge was performed on the radiographic images. For the evaluation, the Al equivalent (mm) for each material was calculated. The data were analyzed using one-way ANOVA and Tukey's test (p<0.05), considering the material factor and then the radiographic method factor, individually.
Results
The high speed mode allowed the highest radiopacity, while the high resolution mode generated the lowest values. Furthermore, the high resolution mode was the most efficient method for radiographic differentiation between restorative composites and dentin. The conventional radiograph was the most effective in enabling differentiation between enamel and composites. The high speed mode was the least effective in enabling radiographic differentiation between the dental tissues and restorative composites.
Conclusion
The high speed mode of digital imaging was not effective for differentiation between enamel and composites. This made it less effective than the high resolution mode and conventional radiographs. All of the composites evaluated showed radiopacity values that fit the ISO 4049 recommendations.
The radiographic exam in the dental field is essential for accurate diagnosis and it is useful in assessing and monitoring the longevity of a restoration.1 Radiopacity is one of the important properties of dental restorative materials since it allows clinicians to assess the integrity of restorations and the development of secondary caries lesions, and to evaluate the interface between the restoration and tooth structure. From this point of view, the radiopacity of the restorative materials should be different than dental substances including enamel and dentin in order to distinguish between them.2 Likewise, materials with a low radiopacity value could lead to an incorrect diagnosis.3
Conventional and digital radiographs are frequently used to evaluate the radiopacity of dental materials. In a conventional radiograph, the radiopacity is based on the measurement of optical density on the radiographic film, and with digital images, special software is used for subsequent measurement of the density values.4 The software in the digital system can change the image resolution to enhance the images according to the clinician's needs.1,5,6
Digital radiography has the advantage of substantially reducing the X-ray exposure time due to the greater sensitivity of the image detectors compared with conventional radiography.7 In addition, digital radiographic systems have the practical utility of needing no darkroom processing step. The image manipulation and enhancement through basic and advanced techniques available in software allows for dynamic analysis of the generated images, adding another advantage to using a digital system. All of these features can contribute to the diagnostic process and alleviate the need for repeated exposures that are unnecessary to the patient.8 Nevertheless, image manipulation such as changes in image resolution might lead to erroneous interpretation due to image degradation.9
Digital systems are widely used to evaluate the radiopacity of restorative composites, but only a few studies have compared their use with conventional radiographs.10 In addition, no study comparing the radiopacity of materials in digital images of different resolutions has been published. Therefore, this study was performed to evaluate the radiopacity of eight composites as well as tooth substances, specifically enamel and dentin, using conventional radiographs and digital images using phosphor storage plates, and compared them. Also, a comparison among digital images at different resolutions was performed.
This study was conducted according to stipulations of the Helsinki Declaration (2000) and previously approved by the Research Ethics Committee of the Federal University of Paraíba in Brazil under protocol number 0134/2009.
This study evaluated 8 kinds of composites. Their respective brand names, chemical compositions, and manufacturers are presented in Table 1. All of the composites were the same color (A2).
As recommended by ISO 4049:2009, stainless steel circular molds with a 10-mm internal diameter and 1-mm height were used to prepare the specimens.11 Under a controlled temperature (26±1℃), the mold was positioned on a glass plate and the resin composites were inserted until the mold was completely filled. Next, a polyester strip was positioned on the upper surface and another glass plate was placed over the strip to flatten the surfaces. Then, the upper glass plate was removed and photo cured by a halogen light device (Optilux Plus, Gnatus Ltda, São Paulo, SP, Brazil; 400 mW/cm2 light intensity) for 40 seconds. Five specimens for each composite were prepared. Before preparation of the specimens of each group, the light output was checked by a radiometer (Model 100 Curing Radiometer, Demetron Research Corporation, Danbury, CT, USA) and had to be equal to or greater than 400 mW/cm2. The light-curing unit was positioned on both sides of the specimen for an additional 20 seconds after removing the strips and glass slabs. The specimens were removed from the metallic molds, polished using Sof-Lex discs (3M ESPE, St. Paul, MN, USA) with decreasing grit to create a flat surface, and measured with a digital caliper to verify the thickness. The specimens were stored in 37℃ distilled water for 24 hours to complete their polymerization. Radiographs of all of the specimens were taken, and the specimens with radiographically heterogeneous images were eliminated and replaced.
The present study also used 5 sound human permanent third molars that had been recently extracted. Patients were informed that their teeth were to be extracted for orthodontic reasons and informed consent was obtained from each patient. The teeth were cleaned and the roots were removed 2 mm below the cemento-enamel junction. Slices of molar teeth were prepared using a diamond disk mounted on a handpiece under water cooling. The most central portion of the tooth in the bucco-lingual direction was used, and the buccal and lingual portions were discarded (Fig. 1). These slices were polished under water cooling down to 1200-grade sandpaper to regularize the occlusal surface and 2-mm thick specimens were obtained. The slices were maintained in distilled water until use.
An aluminum step wedge, made of 99.5% pure aluminum with seven 1-mm thickness incremental steps, was used as an internal standard for each radiographic exposure, which allowed the radiopacity of each material to be calculated in terms of aluminum thickness and controlled any variation in exposure and processing.
One specimen of each material, a tooth slice comprised of both dentin and enamel, the aluminum step wedge, and a lead plate were positioned side by side on a #4 sized piece of conventional intraoral radiographic film (Insight, Eastman Kodak Co, Rochester, NY, USA) (Fig. 2). The conventional radiographs were obtained with a dental X-ray unit (X Timex 70C, Gnatus, São Paulo, SP, Brazil), with 2-mm aluminum equivalent total filtration, at 70 kVp, 7 mA, and 0.5 seconds using a standardized focus-to-film distance of 40 cm. The films were manually developed in a darkroom according to the time and temperature recommendations of the manufacturer (Kodak, Manaus, AM, Brazil) (Fig. 3).
Digital radiographic images were obtained with 2 modes of different resolution, "high speed" and "high resolution" modes, which were possible with the digital radiographic equipment. The digital images were acquired using a #4 sized storage phosphor plate (CR 7400, Kodak, Rochester, NY, USA). The digital images were acquired using the same dental X-ray unit with 0.32 seconds of exposure time.
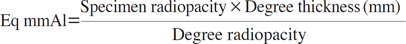
Gross radiographic densities (GRD) of the radiographic sets (specimen, aluminum wedge, and unexposed part of the conventional film) were measured using a digital densitometer (MRA, Ribeirão Preto, SP, Brazil). For each specimen, three readings were taken, and the mean GRD values were calculated. The net optical density (NOD) was derived from the following equation: NOD=GRD-(base+fog). Here, "(base+fog)" was the radiographic density of the part of the film where the lead sheet had been. The NOD values were converted to equivalent mmAl (Eq mmAl) values by the following equation.12
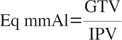
The storage phosphor plates were scanned in either the high speed or high resolution mode in the scanner using the manufacturers' software. The files were exported and saved in the tagged image file format (TIFF). The scores for the gray tones were measured using Digora Software (ver. 2.5 for Windows, Soredex Co., Tuusula, Finland). The transformation of the gray tones values (GTV) in mmAl was performed according to the following equation:
Inverse pixel value (IPV) was calculated by the following equation:7
The data were evaluated using one-way analysis of variance (ANOVA) and Tukey's test to make pairwise comparisons. The data was considered individually for comparison with the material factor and then the radiographic system factor (conventional radiographs, digital images of high speed/high resolution modes). The level of significance was set at p<0.05.
On the conventional radiographs, the most radiopaque material was Natural Flow®, which was the only material as radiopaque as enamel (p>0.05). On the other hand, Natural Flow®, Opallis®, and Fill Magic Flow® were not different from dentin (p>0.05). All of the other materials showed lower radiopacity compared with dentin, but they showed no statistical difference (Table 2).
The digital images in the high speed mode showed that all evaluated restorative composites presented similar radiopacity compared with enamel (p>0.05). However, Fill Magic®, TPH® Spectrum® and Esthet X® showed mean values of radiopacity significantly higher than dentin (p<0.05, Table 2).
In the evaluation of radiopacity on the digital images in the high resolution mode, Esthet X®, Fill Magic®, TPH Spectrum®, Filtek Z350®, and Filtek Z250® had the highest radiopacity values, even greater than the enamel (p<0,05). Fill Magic Flow®, Natural Flow®, and Opallis® were not statistically different than enamel (p>0.05). Dentin had the lowest radiopacity (Table 2).
In general, the digital images in the high speed mode were the most effective among the three types of images in obtaining the highest radiopacity values. On the other hand, they were the least effective in differentiating the composites from the dental tissue.
The digital images in the high resolution mode were the least useful for registering higher radiopacity values (Table 2). On the other hand, the images in this mode were the only ones that showed a lower mean radiopacity value for dentin (p<0.05) than all of the restorative composite types except Natural Flow® (p>0.05). Moreover, the conventional radiographs were the most effective in the differentiation between enamel and restorative composites.
Several studies have evaluated the radiopacity of restorative composites by the digital method.7,10,13 However, only a few studies have compared this method with the conventional radiograph.5 To our knowledge, this was the first study to evaluate the radiopacity of composite resins by using digital images of different resolutions and comparing them with conventional radiographs. The difference in the resolution of radiographic images could interfere with dental diagnoses.
The radiopacity values of materials for restorative composites are suggested by international norms such as ISO 4049,11 which indicates an adequate radiopacity similar to the same thickness of pure aluminum. The American Dental Association has recommended that these materials should have a radiopacity around 1 mmAl, and this value should be approximately equal to the dental tissues' radiopacity.14 In this study, the conventional radiograph showed that all materials presented the mean radiopacity values according to the ISO 4049 norm.11
In the present study, two flowable resins were evaluated. There is considerable variance in the radiopacity of flowable composites, and care must be taken when selecting an appropriate material to enable secondary caries detection under posterior composite restorations.13 In the current study, Natural Flow® was similar to enamel and dentin, showing a radiopacity higher than the other composites, and this result was similar to other studies that evaluated low-viscosity resins.13,15
In our study, the mean radiopacity of dentin was higher than that of the first aluminum step on the conventional radiograph. This might have originated from the chemical processing of the radiographs, a critical procedure, and there could also have been interference from the operator, room temperature variations, and differences in developing solutions. However, we used the time/temperature method, ready to use solutions, a standardized temperature of 25℃, and a single operator to develop the radiographs. Another study showed that the focus-to-film distance and radiographic exposure time also had influenced radiopacity values,16 although these factors were not considered in our study.
Aiming to resolve limitations inherent in conventional radiographic systems, digital systems were designed. There are two main types of technology used in digital radiographic imaging for dentistry: the image detectors using CCD/CMOS sensors and those using storage phosphor plates. This study used a storage phosphor plate system. This system may be considered one of the most appropriate commercially available substitutes for conventional radiography. It offers all the image processing features possible for digital radiographs as well as high diagnostic accuracy and a wide dynamic range provided by low radiation doses.9 However, there is an important limitation that must be overcome to establish its use in clinical practice: the relatively higher cost compared with conventional radiography.10
In this study, digital images in two modes, including high speed and high resolution modes with different resolutions, were used to evaluate the radiopacity of restorative composites by phosphor storage plates. The results showed that the high speed mode (relatively low resolution) led to the highest radiopacity values when compared with the other methods analyzed. The mean radiopacity values of all of the composites, when evaluated in the high speed and high resolution digital systems, were in accordance with the ISO 4049 recommendations.11
Several authors have recommended that the restorative composites be required to have higher radiopacity than dental tissues, especially in posterior restorations, in order to improve the detection of the tooth-restoration interface.15,17 Our results have showed that the mean radiographic density of dentin was statistically different from the majority of the composites on the digital images in the high resolution mode and conventional radiographs. Only Natural Flow® presented similar radiopacity values to dentin on all the images in this study. This might indicate that the indication of this material to fill areas with undermined enamel, one of the purposes recommended by the manufacturer, is inadvisable. The impossibility of radiographic differentiation at the dentin-resin flow interface could lead to an inadequate diagnosis of dental caries. On the other hand, when a high resolution was employed with the digital system, the Fill Magic Flow® showed an average value of radiopacity significantly greater than dentin.
The digital image in the high speed mode was less efficient in enabling radiographic differentiation between dental tissues and restorative composites. In this study, when the high speed mode was employed for the digital images, there was no statistically significant difference between the mean radiopacities of enamel, dentin, and the majority of the composites. Only Esthet X®, Fill Magic®, and TPH® Spectrum showed a significantly higher radiopacity than dentin (p<0.05), but they were not different from the enamel (p>0.05). Therefore, the digital images in the high speed mode were not effective for radiographic differentiation between dental tissues and restorative composites, and they were worse than both the digital images in the high resolution mode and conventional radiographs.
In this study, the radiographic density of composites was higher than that of enamel on the digital images of both modes, but not on conventional radiographs. In clinical practice, in which conventional radiographs are used most of the time, this can lead to the need for repeated radiographs or even lead to a false-positive diagnosis of secondary caries. On both occasions, more time and clinical materials will be spent, increasing the dental interventions' costs. In terms of public health, these increased costs can make it difficult for the population to access dental services. This would also increase the population's radiation exposure.
The digital systems are able to provide high image quality with significantly reduced radiation doses compared with conventional radiographs. These systems are especially indicated for professionals who take few radiographs (e.g., dentists in private practice) due to the inconvenience of developing a small number of films.9 However, the use of digital systems may also be promising for public clinics, increasing the diagnostic accuracy and the correct implementation of treatment planning. This would reduce the number of procedures performed based on false-positive diagnoses, therefore reducing service costs. Thus, the relatively higher cost of the digital systems in comparison with conventional radiography18 can be expected to be made up for by the cost-effectiveness of the digital system.
In conclusion, the high speed mode (low resolution) digital images were not effective. The digital images in the high resolution mode allowed the most efficient radiographic differentiation between restorative composites and dentin. The conventional radiograph allowed the most efficient radiographic differentiation between enamel and composites. In all of the radiographic systems in this study, the restorative composites showed appropriate radiopacity values according to the ISO 4049 recommendations.
Figures and Tables
 | Fig. 2The aluminum step wedge (a), specimens of each material (b), a tooth slice comprised of both dentin and enamel (c), and a lead plate (d) are positioned side-by-side on a #4 sized piece of intraoral conventional radiographic film for irradiation procedures. |
References
1. Rasimick BJ, Gu S, Deutsch AS, Musikant BL. Measuring the radiopacity of luting cements, dowels, and core build-up materials with a digital radiography system using a CCD sensor. J Prosthodont. 2007; 16:357–364.

2. Attar N, Tam LE, McComb D. Flow, strength, stiffness and radiopacity of flowable resin composites. J Can Dent Assoc. 2003; 69:516–521.
3. Tsuge T. Radiopacity of conventional, resin-modified glass ionomer, and resin-based luting materials. J Oral Sci. 2009; 51:223–230.

4. Tagger M, Katz A. Radiopacity of endodontic sealers: development of a new method for direct measurement. J Endod. 2003; 29:751–755.

5. Sabbagh J, Vreven J, Leloup G. Radiopacity of resin-based materials measured in film radiographs and storage phosphor plate (Digora). Oper Dent. 2004; 29:677–684.
6. Wadhwani C, Hess T, Faber T, Piñeyro A, Chen CS. A descriptive study of the radiographic density of implant restorative cements. J Prosthet Dent. 2010; 103:295–302.

7. Dukic W, Delija B, Derossi D, Dadic I. Radiopacity of composite dental materials using a digital X-ray system. Dent Mater J. 2012; 31:47–53.

8. Nomoto R, Mishima A, Kobayashi K, McCabe JF, Darvell BW, Watts DC, et al. Quantitative determination of radio-opacity: equivalence of digital and film X-ray systems. Dent Mater. 2008; 24:141–147.

9. Zdesar U, Fortuna T, Valantic B, Skrk D. Is digital better in dental radiography? Radiat Prot Dosimetry. 2008; 129:138–139.

10. Oliveira AE, de Almeida SM, Paganini GA, Haiter Neto F, Bóscolo FN. Comparative study of two digital radiographic storage phosphor systems. Braz Dent J. 2000; 11:111–116.
11. International Organization for Standardization. ISO 4049: 2009. Dentistry-Polymer based restorative materials. 4th ed. Geneva: ISO;2009.
12. Tanomaru-Filho M, Laitano SC, Gonçalves M, Tanomaru JM. Evaluation of the radiopacity of root-end filling materials by digitization of radiographic images. Braz J Oral Sci. 2006; 5:1018–1021.
13. Ergücü Z, Türkün LS, Onem E, Güneri P. Comparative radiopacity of six flowable resin composites. Oper Dent. 2010; 35:436–440.

14. The desirability of using radiopaque plastics in dentistry: a status report. Council on Dental Materials, Instruments, and Equipment. J Am Dent Assoc. 1981; 102:347–349.
15. Imperiano MT, Khoury HJ, Pontual ML, Montes MA, Silveira MM. Comparative radiopacity of four low-viscosity composites. Braz J Oral Sci. 2007; 6:1278–1282.
16. Poorsattar Bejeh Mir A, Poorsattar Bejeh Mir M. Assessment of radiopacity of restorative composite resins with various target distances and exposure times and a modified aluminum step wedge. Imaging Sci Dent. 2012; 42:163–167.

17. Murchison DF, Charlton DG, Moore WS. Comparative radiopacity of flowable resin composites. Quintessence Int. 1999; 30:179–184.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download