Abstract
Eosinophilic granuloma is a common expression of Langerhans cell histiocytosis and corresponds with typical bone lesions. The radiographic appearance of eosinophilic granuloma in the jaw is variable and not specific. It may resemble periodontitis, radicular cyst, or malignancies. The purpose of this report is to describe the characteristic radiographic features of eosinophilic granuloma of a 39-year-old male. The lesion in the anterior mandible was first diagnosed as radicular cyst because the radiographic findings were ovoid radiolucent lesion with well-defined border. However, careful interpretation revealed a non-corticated border and floating tooth appearance that were the characteristic radiographic features for the differential diagnosis. Early clinical signs of eosinophilic granuloma can occur in the jaw and a bony destructive lesion might be mistaken for periodontitis or an odontogenic cystic lesion; therefore, careful interpretation of radiographs should be emphasized.
Langerhans cell histiocytosis is a rare disease of unknown pathogenesis involving clonal proliferation of Langerhans cells.1 The term "Langerhans cell histiocytosis" was introduced by the Writing Group of the Histiocyte Society,2 replacing histiocytosis X, which had been proposed in 1953 by Lichtenstein3 and encompassed 3 disorders: eosinophilic granuloma, Hand-Schüller-Christian disease, and Letterer-Siwe disease.
Eosinophilic granuloma is the most benign and common form of Langerhans cell histiocytosis, and it involves localized lesions predominantly of the bones.4 It accounts for 60-70% of all cases of Langerhans cell histiocytosis and can be seen as solitary or multifocal bone defects.5,6 The radiographic appearance of eosinophilic granuloma in the jaw is quite variable and not specific7 although the lesions usually appear as radiolucent lesions with well-defined borders.5,8 The lesions might resemble periodontal diseases, odontogenic cysts, ameloblastoma, and malignancies.9
This case may serve to illustrate the various radiographic features of eosinophilic granuloma, and the importance and the difficulties of an early diagnosis by plain radiographs of the jaw. The radiographic features of this case mimicked radicular cyst. However, careful interpretation of the radiograph revealed the non-corticated border and floating tooth appearance suggesting a more aggressive lesion.
This mandibular lesion underwent multifocal dissemination, involving the femur after a one-year disease-free period. The purpose of this case report was to describe characteristic radiographic features of eosinophilic granuloma in an adult.
In May 2008, a 39-year-old man visited Wonkwang Dental Hospital in the city of Daejeon with pain in the anterior region of the mandible originating several months earlier. Intraoral examination revealed a slight gingival swelling and mobility of the mandibular anterior teeth. The past history of the patient was not contributory. There was no cervical or axillary lymphadenopathy. A panoramic radiograph showed an ovoid shaped, unilocular radiolucent lesion with a well-defined margin in the alveolar bone from the left lower lateral incisor to the right lower canine, with involvement of the apices of the mandibular incisors (Fig. 1A). An intraoral radiograph revealed that the border of the lesion was non-corticated with beveled edges. The distal part of the right lower lateral incisor showed a typical floating tooth appearance. However, there was no tooth displacement and no root resorption (Fig. 1B). The patient underwent root canal treatments of the mandibular left central incisor and right canine for his dental pain (Fig. 2). However, the pain did not subside, and the patient was referred to our department. We suspected an aggressive lesion rather than a cystic lesion due to the non-corticated border and floating tooth appearance. A biopsy of the mandibular anterior lesion was performed, and the patient was diagnosed with eosinophilic granuloma.
About one month later, Cone beam Computed Tomography (CBCT), magnetic resonance (MR) imaging, and whole body bone scintigraphy with a Tc-99m MDP were performed at the dental hospital of Wonkwang University and the medical hospital of Eulgi University in the city of Daejeon. An axial CT showed destruction of the buccal and lingual cortex and a focal bony destructive lesion in the anterior mandible (Fig. 3). An MR image showed a focal high signal intense lesion in the left femur trochanter with adjacent bone marrow edema (Fig. 4). Bone scintigraphy revealed that there was no uptake of radiotracer in the trochanteric portion of the left femur on the initial study (Fig. 5A); however, a new active bone lesion showing increased radiotracer uptake with a central photopenic finding in the left femur was detected in a one year follow-up study (Fig. 5B). A biopsy specimen from the left femur was also taken, and the result showed the same lesion, eosinophilic granuloma. Another examination and laboratory tests, consisting of blood and serum biochemical studies, were within normal ranges. The treatment of the femur was carried out by surgical curettage.
Two years later, the patient revisited our dental hospital for the treatment of eosinophilic granuloma in the anterior mandible. A panoramic radiograph showed a slight increase in the size of the lesion in the anterior part of the mandible (Fig. 6) compared with radiographs at the initial visit. The lesion was found to extend from the left lower first premolar to the right lower canine. Alveolar bone resection of the lesion was performed for complete removal of the lesion, and a biopsy specimen was taken.
Microscopically, the hematoxylin-eosin stained sample showed numerous Langerhans cells, eosinophils, and small lymphocytes. Immunohistochemically, these cells showed positivity for S-100 protein and CD1a protein (Fig. 7). Based on the clinical, radiological, and histopathological findings, the final diagnosis was an eosinophilic granuloma in the mandible and femur. The patient was periodically recalled for a follow-up check.
Eosinophilic granuloma, characterized by a proliferation of Langerhans cells, with eosinophils, histiocytes, neutrophils, and scattered plasma cells,10 is the common form of Langerhans cell histiocytosis and is mostly seen between the first and third decades.11 It is rarely seen in adults, and affects only 1-2/million people.12
The clinical presentation of eosinophilic granuloma is different in different age groups.13 Symptoms range from none to pain, swelling, loosening of teeth, and limitation of mouth opening. Adults are usually confined to a single organ and may be asymptomatic and spontaneously regress.13,14 In the present case, the patient, a male who was 39 years old, which is an unusual age for eosinophilic granuloma, presented with loosening teeth and gingival swelling.
Radiographically, eosinophilic granuloma appears as an osteolytic lesion with a well-demarcated border, but the borders are diffuse or poorly defined in some cases. If the lesions have invaded the alveolar crest, these cases may show the characteristic feature of a "scooped out" appearance.8,12,15 In many instances, the radiographic features showed selective destruction of the alveolar bone, causing the tooth to have a "floating tooth" appearance.8
The radiographic features vary widely with the phase of the disease.10 Poorly delimited borders at the initial stage and a more sharply delineated border in the middle phase are characteristic, whereas in the late phase a thick rind of sclerotic tissue occasionally presents. It is possible to observe an osteolytic process, usually located in the medullary cavity, but occasionally in the cortex,16 and the cortical bone may be perforated or periosteal bone formation may occur.16,17 In the present case, the mandibular lesion was observed in the medullary space, with a perforated buccal cortex but no periosteal bone formation was observed (Fig. 3).
The variable radiographic appearance makes the differential diagnosis of eosinophilic granuloma more difficult. The lesion may be mistaken for an odontogenic cyst, osteomyelitis, or a malignancy.8 Given its scooped out appearance, the differential diagnosis included the alternatives of Ewing's sarcoma, lymphoma, and metastatic disease.12 In this case, a radicular cyst was suspected in the differential diagnosis because the jaw lesion showed an oval radiolucency with a well-defined border at the periapical region (Fig. 1). According to Hartman,18 the monostotic form of eosinophilic granuloma is more prevalent than the polyostotic type. The bony sites most often affected by eosinophilic granuloma are the skull, femur, ribs, vertebrae, and mandible.8 When the jaws are affected, the mandible is a more common site than the maxilla.19 When multiple lesions occur, the new osseous lesions appear within 1-2 years.4 With the aid of skeletal scintigraphy, the additional lesion at the femur as well as the anterior mandible could be suspected on one year follow-up study (Fig. 5).
Routine diagnosis is usually made on the basis of histological examination, and the presence of S-1007,20 and CD1a6,21 by immunohistochemical examination could confirm eosinophilic granuloma.
Treatment includes surgery, radiotherapy, chemotherapy, and intra-lesional injection of corticosteroids.8 Surgery is the preferred method of treatment for a single and localized manifestation of the disease. Radiotherapy is suggested in cases of local recurrence or if surgical treatment is not possible.21 The patient in this case was treated with surgical resection of the mandible site and surgical curettage of the left femur.
Early clinical signs of eosinophilic granuloma can occur in the jaw and a bony destructive lesion might be mistaken for periodontitis or a cystic lesion. The radiolucent lesion in this case was first diagnosed as a radicular cyst because of the unilocular lesion with well-defined border. However, careful interpretation of the radiograph revealed its non-corticated border and floating tooth appearance, resulting in suspicion of a more aggressive lesion.
In conclusion, we insist on the fact that accurate radiographic differential diagnosis of eosinophilic granuloma is critical to both recognition and proper management of this condition.
Figures and Tables
Fig. 1
A. A panoramic radiograph shows a radiolucent lesion with a well-defined margin from the left lower lateral incisor to the right lower canine. B. A periapical radiograph reveals a radiolucent lesion with a non-corticated border and beveled edges. The distal part of the right lower lateral incisor shows a "floating tooth" appearance.
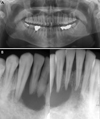
Fig. 2
A periapical radiograph shows root canal treatment of the mandibular left central incisor and right canine.

Fig. 3
An axial CT image shows a focal bony destructive lesion in the anterior mandible. Destruction of the buccal and lingual cortex is also observed.
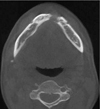
Fig. 4
Fat saturated coronal T2 weighted MR image (TR/TE: 3750/103 milliseconds) shows a focal high signal lesion (arrow) in the left femur tronchanter with adjacent bone marrow edema.
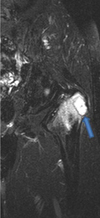
Fig. 5
Bone scintigraphy. A. The initial study shows normal uptake of the radiotracer in the trochanteric portion of the left femur. B. The one year follow-up study demonstrates an uptake lesion in the left femur.

Fig. 6
Panoramic radiograph (2 years later) shows a slight increase in the lesion size in the anterior part of the mandible compared with the initial radiographs.

Fig. 7
A. Numerous Langerhans cells, recognized by their grooved, folded, or indented nuclei with fine chromatin, inconspicuous nucleoli, and thin nuclear membranes, with a few scattered eosinophils and small lymphocytes are seen (H&E stain, 400×). The tumor cells are strongly immunoreactive for S-100 protein (B, 200×) and CD1a (C, 200×) in the cytoplasm.

References
2. Chu T, D'Angio GJ, Favara BE, Ladisch S, Nesbit M, Pritchard J. Histiocytosis syndromes in children. Lancet. 1987. 2:41–42.
3. Lichtenstein L. Histiocytosis X: integration of eosinophilic granuloma of bone, Letterer-Siwe disease, and Schüller-Christian disease as related manifestations of a single nosologic entity. AMA Arch Pathol. 1953. 56:84–102.
4. Parihar A, Newaskar V. Management of polyostotic eosinophilic granuloma. Dent Res J (Isfahan). 2012. 9:821–825.
5. Esen A, Dolanmaz D, Kalayci A, Günhan O, Avunduk MC. Treatment of localized Langerhans' cell histiocytosis of the mandible with intralesional steroid injection: report of a case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010. 109:e53–e58.

6. Key SJ, O'Brien CJ, Silvester KC, Crean SJ. Eosinophilic granuloma: resolution of maxillofacial bony lesions following minimal intervention. Report of three cases and a review of the literature. J Craniomaxillofac Surg. 2004. 32:170–175.

7. Holzhauer AM, Abdelsayed RA, Sutley SH. Eosinophilic granuloma: a case report with pathologic fracture. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999. 87:756–759.
8. Ardekian L, Peled M, Rosen D, Rachmiel A, Abu el-Naaj I, Laufer D. Clinical and radiographic features of eosinophilic granuloma in the jaws: review of 41 lesions treated by surgery and low-dose radiotherapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999. 87:238–242.
9. Jones LR, Toth BB, Cangir A. Treatment for solitary eosinophilic granuloma of the mandible by steroid injection: report of a case. J Oral Maxillofac Surg. 1989. 47:306–309.

10. Piattelli A, Paolantonio M. Eosinophilic granuloma of the mandible involving the periodontal tissues. A case report. J Periodontol. 1995. 66:731–736.

11. Uckan S, Gurol M, Durmus E. Recurrent multifocal Langerhans cell eosinophilic granuloma of the jaws: report of a case. J Oral Maxillofac Surg. 1996. 54:906–909.

12. Rees J, Paterson AW. Langerhans cell histiocytosis in an adult. Br J Oral Maxillofac Surg. 2009. 47:52–53.

13. Broadbent V, Egeler RM, Nesbit ME Jr. Langerhans cell histiocytosis - clinical and epidemiological aspects. Br J Cancer Suppl. 1994. 23:S11–S16.
14. Leavey P, Varughese M, Breatnach F, O'Meara A. Langerhans cell histiocytosis - a 31 year review. Ir J Med Sci. 1991. 160:271–274.

15. dos Anjos Pontual ML, da Silveira MM, de Assis Silva Lima F, Filho FW. Eosinophilic granuloma in the jaws. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007. 104:e47–e51.

16. Fechner RE, Mills SE. Tumors of the bones and joints. Atlas of tumor pathology. 3rd series. 1993. Washington: Armed Forces Institute of Pathology;211–215.
17. Mirra JM. Bone tumors: clinical, radiologic, and pathologic correlations. 1989. Philadelphia: Lea and Febiger;1023–1045.
18. Hartman KS. Histiocytosis X: a review of 114 cases with oral involvement. Oral Surg Oral Med Oral Pathol. 1980. 49:38–54.

19. Dagenais M, Pharoah MJ, Sikorski PA. The radiographic characteristics of histiocytosis X. A study of 29 cases that involve the jaws. Oral Surg Oral Med Oral Pathol. 1992. 74:230–236.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download