Abstract
Adenomatoid odontogenic tumor (AOT) usually presents as a unilocular, pericoronal radiolucency in the maxillary anterior region in adolescent females. Very few conditions occur in such a narrow age range and at such a restrictive site. Rarely, these tumors present with varied clinical features. A case of AOT of the mandible is reported with unusual features such as large size, multilocular appearance, and aggressive behavior. The role of radiology in diagnosis of atypical AOT is extremely important. The unique radiological manifestations of the lesion helped in the diagnosis, and it was managed conservatively with no evidence of recurrence.
Adenomatoid odontogenic tumor (AOT) is an uncommon nonaggressive tumor of the odontogenic epithelium.1 Although this tumor has been believed to be a hamartoma rather than a neoplasm, the lesion may rarely exhibit aggressive behavior such as becoming unusually large or spreading into the intracranial space.2,3 AOT occurs in intraosseous and peripheral forms. The intrabony variants comprise the follicular and extrafollicular types. Radiographically, the central lesions appear as well demarcated unilocular radiolucencies often associated with an impacted tooth. Two thirds of the intrabony cases have scattered radiopacities within the radiolucency.4 It has also been found that intraoral radiographs rather than panoramic radiographs are better suited for displaying the discrete calcific deposits.5 A case of adenomatoid odontogenic tumor with unusual manifestations is presented highlighting the role of radiology, particularly computed tomography, in the diagnosis of such lesions.
A 17-year-old female patient visited the Department of Oral Medicine and Radiology with a complaint of swelling in the lower jaw that had begun 5-6 months earlier. The lesion had progressively increased in size and been painful beginning two months earlier. There was no anesthesia or paresthesia of the lower lip, chin, or jaw, and there was no history of trauma.
On extraoral examination, the swelling in the mandibular anterior region measured about 8 cm×5 cm extending about 4 cm from the midline bilaterally (Fig. 1A). Superoinferiorly, it extended from the lower lip to the lower border of the mandible. The skin over the swelling and the surrounding area appeared normal and the margins were diffuse. On palpation, there was no local rise in temperature, but the swelling was tender, especially in the anterior region. Intraoral examination revealed swelling 7 cm×5 cm obliterating the buccal and lingual vestibule extending bilaterally to the buccal sulcus of the first permanent left mandibular molar and first permanent right mandibular molar and measuring about 3.5 cm from the midline bilaterally (Fig. 1B). The expansion of the lingual cortex in the midline region was remarkable. The swelling was bony hard in consistency. The crowns of the mandibular anterior teeth were tipped mesially. The left lateral incisor, right central incisor, and right lateral incisor were grade 2 mobile. Grade 1 mobility was present in the permanent first molar in the left mandibular region and the permanent central incisor in the left mandibular region was clinically missing. The teeth were nontender on percussion. The teeth associated with the swelling - the incisors, canines, premolars and first molars of the left and right side of the mandible - gave a negative response to a vitality test. Since the expansile lesion with clinically aggressive behavior was associated with a missing tooth, a working diagnosis of ameloblastoma was considered. Other odontogenic cysts and tumors including dentigerous cyst and odontogenic keratocyst were considered in the differential diagnosis.
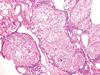
The patient was subjected to radiographic examination including panoramic and intraoral radiographs. The panoramic radiograph revealed a large radiolucent lesion of the mandible extending from the roots of the permanent first molar in the right mandibular region to the permanent first molar in the left mandibular region with well-defined corticated borders (Fig. 2A). The lesion was associated with an impacted permanent central incisor in the left mandibular region, which appeared to be displaced towards the inferior cortex of the mandible. A few radiopaque flecks of about 1-2 mm were noted. The roots of the premolars and molars in the right and left mandibular region showed resorption and all the roots of teeth associated with the lesion showed loss of the lamina dura and widening of the periodontal ligament space. The roots were tipped distally. The lower border of the cortex showed endosteal resorption. The mandibular occlusal radiograph revealed a striking cortical expansion, especially that of the lingual cortex with dense septae in the lingual region giving a multilocular appearance (Fig. 2B). Several radiopaque foci of about 1-2 mm were seen scattered, which were less evident in the panoramic radiograph. Cortical thinning and resorption were evident.
The patient was further subjected to a computed tomography (CT) examination, which demonstrated a large expansile radiolucent lesion with multiple flecks of calcification of varying sizes, which were predominantly peripherally distributed and impacted the permanent central incisor (Fig. 3A). The remarkable lingual and buccal expansion, perforation of the lingual cortex, and dense septae in the lingual region were evident in the CT. The soft tissue density at the periphery suggestive of a capsule was also appreciable (Fig. 3B). The dimensions of the lesion measured 5.82 cm×3.28 cm×3.25 cm (Fig. 3C). A multiplanar three-dimensional reconstructed image showed a multilocular appearance with thick lingual septae and the position of the impacted tooth (Fig. 4).
A radiographic diagnosis of adenomatoid odontogenic tumor (AOT) was arrived at considering the multiple scattered radiopaque flecks in the lesion associated with an unerupted impacted tooth and a soft tissue capsule. However, a multilocular appearance and large size in an AOT is unusual. Hence, a differential diagnosis of other multilocular mixed lesions such as calcifying odontogenic cyst and calcifying epithelial odontogenic tumor was also considered.
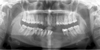
The lesion was surgically enucleated. Macroscopically, the mass was well encapsulated with cystic areas along with an embedded permanent mandibular central incisor in the tumor mass. Histopathological examination revealed sheets, ducts, and whorls of darkly staining ovoid to round epithelial cells suggestive of odontogenic epithelial cells (Fig. 5). The duct-like structures were lined by columnar cells. A few basophilic calcifications were also observed. Small cystic areas containing degenerated cell debris were noted in the focal areas. The supporting connective tissue stroma was loose and less cellular in nature. Based on these findings, a histopathologic diagnosis of adenomatoid odontogenic tumor was made.
The patient was under follow-up and had not shown any signs of recurrence six months after surgery (Fig. 6).
Our reported case had typical presentations of AOT in that it occurred in a 17-year-old female patient in the anterior mandible and presented as a perifollicular radiolucency with radiopaque flecks. However, the lesion had some unusual manifestations, which included its large size, multilocularity, lingual cortical expansion, root resorption, and cortical perforation.
AOT generally does not exceed 1-3 cm in diameter.6 Most cases of large AOTs described in the literature have been observed in the maxilla.7,8 In a recent analysis of AOTs, the large size of the lesions has been attributed to a higher growth rate in younger patients and a delay in seeking treatment.8
A radiolucent lesion containing septae is said to be septated or multilocular.9 Dense septae were evident in the lingual aspect of the tumor, which was a very unusual finding in an AOT. A recent case report describes a multilocular radiolucency associated with two AOTs in the anterior maxilla.10
Discontinuity and thinning of the buccal and lingual cortical plate and calcifications within the lesion, appearing as flecks towards the periphery, were more pronounced in the CT scans. Compared to conventional radiographs, CT may be more beneficial in depicting such calcifications and hence facilitate diagnosis. The presence of calcification excludes the diagnosis of ameloblastoma. One unique feature of AOT that has been described is a well-defined radiolucent band that surrounds the periphery of the lesion. This band is referred to as the capsular space.9 The capsule is clearly evident in the CT images.
Intraosseous AOT may cause displacement of the neighboring teeth. Root resorption is a very rare finding. To the best of our knowledge, about five cases of AOT with root resorption have been reported.10-14
Conservative surgical excision is the treatment of choice for AOTs. However, recurrences have been reported after conservative treatment.14 Hence, careful follow-up should be conducted. Follow-up is of immense importance, especially in our case, considering the rather unusual and aggressive presentation of the tumor. The patient has been asymptomatic and has not shown any signs of recurrence six months after surgery.
In conclusion, a rare case of AOT of the mandible with a multilocular mixed radiolucent, radiopaque appearance and root resorption was reported. Although histopathology can provide a confirmation of diagnosis, plain radiographs and especially CT can guide the diagnosis of such lesions.
Figures and Tables
 | Fig. 1A. An extraoral photograph shows swelling of the mandible. B. Intraoral photograph shows swelling in the anterior mandible. |
 | Fig. 2A. A panoramic radiograph shows the large radiolucent lesion of the mandible with the impacted and displaced left mandibular incisor and root resorption. B. A mandibular cross-sectional occlusal radiograph reveals buccolingual expansion, thinning, and erosion of the cortices, multiple scattered radio-opaque foci, and dense septae. |
 | Fig. 3A. An axial CT image shows the expansile radiolucent lesion with multiple radiopaque flecks towards the periphery. B. An axial CT image of the bone window shows the thinning and discontinuity of the lingual and buccal cortices. C. A coronal CT image shows a large expansile lesion and the soft tissue capsule at the periphery. |
 | Fig. 4A. A three-dimensional CT image (anterior view) depicts the lesion in the mandible and the position of the impacted tooth. B. A three-dimensional CT image (occlusal view) reveals the dense lingual septae and multilocular appearance. |
References
1. White SC, Pharoah MJ. Oral radiology: principles and interpretation. 2004. 5th ed. St. Louis: Mosby.
2. Raubenheimer EJ, Seeliger JE, van Heerden WF, Dreyer AF. Adenomatoid odontogenic tumour: a report of two large lesions. Dentomaxillofac Radiol. 1991. 20:43–45.

3. Takigami M, Uede T, Imaizumi T, Ohtaki M, Tanabe S, Hashi K. A case of adenomatoid odontogenic tumor with intracranial extension. No Shinkei Geka. 1988. 16:775–779.
4. Philipsen HP, Reichart PA. Adenomatoid odontogenic tumour: facts and figures. Oral Oncol. 1999. 35:125–131.

5. Dare A, Yamaguchi A, Yoshiki S, Okano T. Limitation of panoramic radiography in diagnosing adenomatoid odontogenic tumors. Oral Surg Oral Med Oral Pathol. 1994. 77:662–668.

6. Philipsen HP, Reichart PA, Zhang KH, Nikai H, Yu QX. Adenomatoid odontogenic tumor: biological profile based on 499 cases. J Oral Pathol Med. 1991. 20:149–158.
7. Takahashi K, Yoshino T, Hashimoto S. Unusually large cystic adenomatoid odontogenic tumour of the maxilla: case report. Int J Oral Maxillofac Surg. 2001. 30:173–175.

8. Mohamed A, Singh AS, Raubenheimer EJ, Bouckaert MM. Adenomatoid odontogenic tumour: review of the literature and an analysis of 33 cases from South Africa. Int J Oral Maxillofac Surg. 2010. 39:843–846.

9. Langlais RP, Langland OE, Nortje CJ. Diagnostic imaging of the jaws. 1995. Baltimore: Williams & Wilkins;25.
10. Bartake AR, Punnya VA, Sudeendra P, Rekha K. Two adenomatoid odontogenic tumours of the maxilla: a case report. Br J Oral Maxillofac Surg. 2009. 47:638–640.

11. Dayi E, Gurbuz G, Bilge OM, Ciftcioglu MA. Adenomatoid odontogenic tumour (adenoameloblastoma). Case report and review of the literature. Aust Dent J. 1997. 42:315–318.

12. Nomura M, Tanimoto K, Takata T, Shimosato T. Mandibular adenomatoid odontogenic tumor with unusual clinicopathologic features. J Oral Maxillofac Surg. 1992. 50:282–285.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download