Abstract
Osteoma is a benign osteogenic tumor composed of cancellous or compact bone, classified as peripheral, central, or extraskeletal. Peripheral osteomas are uncommon. Excluding the maxillary sinuses, the maxilla is a rare site for osteomas. The purpose of this report was to describe clinicopathological and radiological features of two peripheral osteomas occurring in the jaws, one located in the mandible and another in the edentulous maxillary alveolar ridge. The tumors were asymptomatic and were fully excised without any complications or recurrence. The lesions were submitted to histopathological analysis and diagnosed as peripheral osteoma, compact type.
Osteomas are benign osteogenic tumors characterized by the proliferation of compact and/or cancellous bone.1-3 They are essentially tumors of the craniofacial bones, rarely affecting the extragnathic skeleton.4 The osteomas may be central, peripheral, or extraskeletal. The central type arises from the endosteum, the peripheral counterpart from the periosteum, and the extraskeletal soft tissue osteomas usually develop within muscles.4-6
The reported age at onset ranges from 14 to 58 years, with a mean of 29 years of age, and males are affected more frequently than females in a ratio of approximately 2 : 1. They mainly affect the frontal bone, mandible, or paranasal sinuses.1 Excluding the maxillary sinuses and those cases associated with Gardner syndrome, maxillary osteomas are rare.3 Recently, Nah7 reported 18 cases of craniofacial osteomas and only 1 case occurred in the maxilla. To the best of our knowledge, only 17 well-documented cases of maxillary osteomas have been previously described in the English-language literature, 13 peripheral and 4 central (Table 1).1,3,7-17 Thus, this report described the clinicopathological and radiological features of two solitary peripheral osteomas of the jaws, one located on the mandible and the other on the edentulous maxillary alveolar ridge.
A 33-year-old female patient presented to the Oral Surgery Clinic, complaining of a painless mandibular swelling with approximately 5 years of evolution. The medical history was not contributory. On extraoral examination, a nodule with a lobulated surface, of bony consistency, fixed, extending 2.5 cm, and located on the mandibular angle was observed. The entire tumor was covered by normal skin. Intraorally, no alteration was observed. The computed tomography (CT) scan showed a well-circumscribed, bone-like, hyperdense image (Fig. 1A) with a lobulated surface located on the left mandible angle (Fig. 1B). Peripheral osteoma was the clinicoradiographic diagnosis. Under general anesthesia, the lesion was fully excised, and histopathological analysis showed compact, mature bone, with scarce lacunae and marrow spaces filled by connective tissue within the compact bone (Fig. 2). Based upon the clinical and laboratory findings, a definitive diagnosis of peripheral osteoma, compact type, was established. The patient did not present postoperative complications nor clinical or imaging signs of recurrence after 8 months of follow up.
A 53-year-old male patient was referred to the Oral Medicine Unit for evaluation of a mass in the posterior maxilla originating about 10 years earlier. The patient had good general health with no history of contributory medical factors. Intraoral examination revealed a painless, well-circumscribed, submucosal mass on the right edentulous posterior maxillary alveolar ridge, covered by regular and normally colored mucosa, measuring approximately 1.0 cm in diameter. The lesion presented a hard consistency on palpation, and it was located on the buccal aspect of the maxilla, in the transition line between the attached mucosa and the mobile alveolar mucosa. The nodule presented close proximity to the maxillary tuberosity. No swelling or abnormality was observed in the palatal region. Despite being edentulous, the patient did not use a dental prosthesis. Radiographically, a well-delimited, ovoid, and radiopaque lesion was observed on the edentulous alveolar ridge (Fig. 3). The main hypothesis of diagnosis was peripheral osteoma. Under local anesthesia, an excisional biopsy was performed and the specimen sent for histopathological analysis. Microscopically, in addition to the features described in case 1, a fibrous capsule around the lesion was noted (Fig. 4). The definitive diagnosis of peripheral osteoma, compact type, was established. The patient did not present postoperative complications and has been disease free after 1 year of treatment.
The pathogenesis of osteomas is unclear. Some investigators considered it a true neoplasm, while others classified it as a developmental anomaly.1,10,18 Osteomas exhibit continuous growth rather than growth cessation at adulthood, and this characteristic is the major feature distinguishing them from other bony exostoses,3,5 supporting a neoplastic origin. In addition, the possibility of a reactive mechanism, triggered by trauma or infection has also been suggested.5,18
Mandibular peripheral osteomas occur predominantly in the angle or condyle, followed by the molar area and ramus, as occurred in case 1. Intraoral cases occur frequently in the lingual molar-premolar area.19 In contrast, apart from the maxillary sinus and those cases associated with Gardner syndrome, maxillary osteomas are rare.1,3,7-17 Case 2 seemed to be the eighteenth case of maxillary osteoma published in the English-language literature (Table 1).
Clinically, they appear circumscribed, usually rounded and protuberant,3,5 and are characterized by very slow and continuous growth.10 Peripheral osteoma presents as a unilateral, sessile, or pedunculated mass ranging from 1 to 4 cm in diameter,1,4,6 as observed in both cases. Osteomas, usually asymptomatic, often remain undetected unless incidentally found on a routine radiographic survey or until they cause facial asymmetry or functional impairment.2,4 However, depending upon the location, occlusal dysfunction, facial asymmetry, headaches, facial pain, and limited mandibular movements may occur,2 mainly in condylar osteomas.1,4 Although most peripheral maxillary osteomas (80%) are located on the alveolar process,3,13 as observed in case 2, they rarely cause difficulties in mastication.3
Radiographically, the presence of an oval, radiopaque, well-circumscribed mass attached by a broad base or pedicle to the affected cortical bone is a hallmark of peripheral osteomas.1,19 The differential diagnosis includes exostoses and several pathologic processes including inflammatory and neoplastic lesions such as a sclerotic pattern of chronic osteomyelitis, peripheral ossifying fibroma, periosteal osteoblastoma, osteoid osteoma, and parosteal osteosarcoma.1,4 Distinguishing between exostosis and osteoma may be difficult. The clinical features are essential in determining the final diagnosis since both the conditions present similar histopathological features. Exostoses are usually multiple and located in areas of attached gingival mucosa. Solitary exostoses are rare and occur frequently associated with a local trauma or in regions that received gingival or cutaneous graft.20,21 In the present cases, none of these features were observed.
On the other hand, central osteomas may cause more difficulty in diagnosis. Fibrous dysplasia, central ossifying fibroma, odontoma, osteoblastoma, chondroma, cementoblastoma, Paget's disease, and central osteosarcoma should be added to the differential diagnosis of central osteomas.1,4,10 Moreover, pain is an important symptom in 30% of central osteomas.10
Histological classification differentiates among compact or ivory (dense, compact bone), cancellous (soft, spongy bone), and mixed-type osteomas.1,5,19 The compact osteoma comprises dense, compact bone with few marrow spaces, as observed in our cases. The cancellous osteoma is characterized by bony trabeculae and fibro-fatty marrow enclosing osteoblasts, with architecture resembling mature bone.1 In the jaw, the compact osteoma is the most common histological subtype,22 similar to the current cases.
In patients with multiple maxillofacial osteomas, Gardner syndrome should be considered as a possible diagnosis. In addition to multiple osteomas, cutaneous sebaceous cysts, multiple supernumerary teeth, and colorectal polyposis might be also observed.1,23 In our cases, the lesions were solitaries, there were no teeth abnormalities, and no intestinal complaints were reported.
The optimal treatment is surgical, recurrence is rare, and there has been no report of malignant transformation.1 The postoperative follow-up should include periodic clinical and radiographic studies.
In summary, osteomas occur predominantly in the maxillofacial region, appearing as slow growing and well-circumscribed, lobulated masses. However, maxillary osteomas are extremely rare lesions and located mainly on the alveolar ridge. The ideal treatment is conservative surgical removal and recurrence is uncommon.
Figures and Tables
Fig. 1
A. Computed tomography (CT) scan reveals a well-circumscribed, bone-like, hyperdense image located on the left mandibular angle. B. CT image shows a lesion with a lobulated surface.

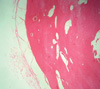
Fig. 2
Histopathological examination shows compact and mature bone, with scarce lacunae and marrow spaces filled by a connective tissue (H&E stain, ×100).

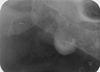
Fig. 3
Periapical radiograph shows a well delimited, ovoid, and radiopaque lesion observed on the edentulous alveolar ridge.
References
1. Sayan NB, Uçok C, Karasu HA, Günhan O. Peripheral osteoma of the oral and maxillofacial region: a study of 35 new cases. J Oral Maxillofac Surg. 2002. 60:1299–1301.

2. Aghabeigi B, Evans AW, Crean SJ, Hopper C. Simultaneous repair of an orbital floor fracture and removal of an ethmoid osteoma: case report and review of the literature. Int J Oral Maxillofac Surg. 2003. 32:94–96.

3. Durighetto AF Jr, de Moraes Ramos FM, Rocha MA, da Cruz Perez DE. Peripheral osteoma of the maxilla: report of a case. Dentomaxillofac Radiol. 2007. 36:308–310.

4. Longo F, Califano L, De Maria G, Ciccarelli R. Solitary osteoma of the mandibular ramus: report of a case. J Oral Maxillofac Surg. 2001. 59:698–700.

5. Kaplan I, Calderon S, Buchner A. Peripheral osteoma of the mandible: a study of 10 new cases and analysis of the literature. J Oral Maxillofac Surg. 1994. 52:467–470.

6. Bodner L, Gatot A, Sion-Vardy N, Fliss DM. Peripheral osteoma of the mandibular ascending ramus. J Oral Maxillofac Surg. 1998. 56:1446–1449.

8. Seward MH. An osteoma of the maxilla. Br Dent J. 1965. 118:27–30.
9. Rajayogeswaran V, Eveson JW. Endosteal (central) osteoma of the maxilla. Br Dent J. 1981. 150:162–163.

10. Kaplan I, Nicolaou Z, Hatuel D, Calderon S. Solitary central osteoma of the jaws: a diagnostic dilemma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008. 106:e22–e29.

11. Dalambiras S, Boutsioukis C, Tilaveridis I. Peripheral osteoma of the maxilla: report of an unusual case. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005. 100:e19–e24.

12. Woldenberg Y, Nash M, Bodner L. Peripheral osteoma of the maxillofacial region. Diagnosis and management: a study of 14 cases. Med Oral Patol Oral Cir Bucal. 2005. 10:E139–E142.
13. Iatrou IA, Leventis MD, Dais PE, Tosios KI. Peripheral osteoma of the maxillary alveolar process. J Craniofac Surg. 2007. 18:1169–1173.

14. Chaudhry J, Rawal SY, Anderson KM, Rawal YB. Cancellous osteoma of the maxillary tuberosity: case report. Gen Dent. 2009. 57:427–429.
15. Wong RC, Peck RH. Enlargement of the right maxilla - report of an unusual peripheral osteoma. Ann Acad Med Singapore. 2010. 39:576–577.
16. de Santana Santos T, Frota R, Martins-Filho PR, Melo AR, de Souza Andrade ES, de Oliveira e Silva ED, et al. Central osteoma of the maxilla with involvement of paranasal sinus. J Craniofac Surg. 2011. 22:589–591.
17. Sah K, Kale A, Seema H, Kotrashetti V, Pramod BJ. Peripheral osteoma of the maxilla: a rare case report. Contemp Clin Dent. 2011. 2:49–52.

18. Cutilli BJ, Quinn PD. Traumatically induced peripheral osteoma. Report of a case. Oral Surg Oral Med Oral Pathol. 1992. 73:667–669.
19. Kashima K, Rahman OI, Sakoda S, Shiba R. Unusual peripheral osteoma of the mandible: report of 2 cases. J Oral Maxillofac Surg. 2000. 58:911–913.

20. Neville B, Damm DD, Allen CM, Bouquot J. Oral and maxillofacial pathology. 2009. 3rd ed. St. Louis: Saunders;19–22.
21. Verweij KE, Engelkens HJ, Bertheux CA, Dees A. Multiple lesions in upper jaw. Multiple buccal exostoses. Neth J Med. 2011. 69:347–350.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download