This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
Dental trauma is frequently unpredictable. The initial assessment and urgent treatment are essential for dentists to save the patient's teeth. Mobile-phone-assisted teleconsultation and telediagnosis for dental trauma could be an aid when a dentist is not available. In the present in-vitro study, we evaluated the success rate and time to transfer images under various conditions.
Materials and Methods
We analyzed the image quality of cameras built into mobile phones based on their resolution, autofocus, white-balance, and anti-movement functions.
Results
The image quality of most built-in cameras was acceptable to perform the initial assessment, with the autofocus function being essential to obtain high-quality images. The transmission failure rate increased markedly when the image size exceeded 500 κB and the additional text messaging did not improve the success rate or the transmission time.
Conclusion
Our optimal protocol could be useful for emergency programs running on the mobile phones.
Keywords: Cellular Phone, Tooth Injuries, Emergencies, Remote Consultation
Introduction
It is well known that the correct initial assessment and urgent treatment are the most important factors to save the patient's teeth in dentoalveolar trauma.
1 Dental experts can assess the severity of the trauma in the dental clinic by performing a physical examination and a radiologic analysis, however this is not always possible for dental accidents that occur when dentists are not available due to the distance between the patient's location and a dental clinic.
1,
2
Many people, including children, now possess a mobile phone, and the use of mobile phones is expanding in telemedicine due to their convenience and connectivity. Teleconsultation with such a device can be effective in telemedicine.
3-
5 However, unlike other telemedicine fields, teledentistry with mobile phones is not popular due to the poor quality of the built-in cameras and successful transmission not being guaranteed.
4,
6-
8 The image quality is influenced by various factors such as the resolution of the camera and its autofocusing, anti-movement, white-balance, and external-flash functions. Moreover, obtaining images with the correct composition is difficult even when the photographer is a dental healthcare provider.
Another obstacle to using mobile phones in teleconsultation is the transmission time and success rate. Although high-quality images could aid correct diagnosis, the transmission failure could be more likely and the time for transmission would be longer than for a lower resolution image. These factors could be detrimental to emergency consultations for dental trauma. Therefore, the protocol for the optimal image size and transmission time for teleconsultation in dentoalveolar trauma needs to be determined.
This study investigated various conditions for teleconsultation in dental trauma in order to obtain the optimal protocol for teledentistry in emergency dental care.
Materials and Methods
Model and Acquisition Methods
A dentiform model mimicking dental hard and soft tissue (D85DP-500B.1, Nissin Dental, Kyoto, Japan) was used as an in-vitro model. Two mobile phones available in the Korean market were used in this study (IM-U310K, Sky, Seoul, Korea and iPhone 3GS, Apple, Cupertino, CA, USA).
In order to evaluate dental hard and soft tissue from two directions, photographs of frontal and occlusal views of the upper anterior teeth were taken (
Fig. 1). Each photograph showed six upper anterior teeth including four anterior incisors and two canines.
Image-Quality Variables: Availability for Clinical Diagnosis
We took two photographs with each setting of the following features of the built-in cameras: autofocusing, blurring, white balance, focal length, and resolution. The effect of blurring was produced by performing mild and moderate movements when taking the image. The effect of focal length was evaluated both for the rear- and front-facing cameras. The image quality was assessed by a single dentist as either "success" or "failure", with the former being concluded when all of the following conditions were acceptable: the presence of teeth, continuity of teeth and/or alveolar bone, shape of the teeth and their discoloration, and gingival texture, color, and shape.
Transmission Variables: Success Rate of Transmissions
We also investigated the transmission performance under various conditions. We first evaluated the success rate of transmission according to the number of image files transmitted, and then calculated the file size and correlated the assessment of success or failure with the total file size. A text message was sent in each test to validate the effect of sending text with images. Finally, we calculated the time and success rate of transmissions for various sending locations representing the patient's location including a parking lot, elevator, and subway.
Results
The image resolution of the cameras varied from 320×240 to 960×1600 pixels, with the corresponding file size varying from 30 to 985 kB. The image resolution and file size had no effect on whether images were assessed as "success" or "failure".
Table 1 and
Figure 2 indicate the distribution of image as "success" and "failure" assessments according to presence of autofocus and blurring. The autofocusing function was the most important factor for achieving an informative image. The worst results were obtained when the image was blurred by movements.
Table 2 lists the effects of focal length according to two types of built-in cameras. The rear-facing camera is on the back of the mobile phone and the camera for video calling is on the front. The optimal focal lengths for taking images of teeth were 3-7 and 13 cm for the front- and rear-facing cameras, respectively.
Table 3 indicates the effect of white balance. The use of automatic white balance produced the clearest and most-vivid images. The decision criteria of the number and alignment of teeth, shape of teeth, and gingival texture were not affected by white balance, while discoloration of teeth was severely affected by inappropriate white-balance conditions.
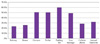
The effects of the number and total size of image files are demonstrated in
Table 4. The transmission time and success rate were affected more by the total file size than by the number of files.
The addition of text messages did not affect the success rate. However, when the file size exceeded 500 kB, the transmission time increased and the success rate was reduced to 70% (
Table 5).
In terms of the sending locations and reception conditions, the success rate of image transmission was lower in situations with poor wireless communication conditions such as the parking lot, elevator, and subway (
Fig. 3). The transmission time increased slightly when the receiver was using a mobile phone for calling or text messaging.
Discussion
The ability to transfer images to a specialist who is acquainted with dental trauma could improve the likelihood of preserving the patient's teeth in cases of dentoalveolar trauma. During teleconsultation, the available images are the most important factor affecting the success outcome, with image quality and transmission characteristics being crucial. Several types of camera systems can be used to capture images of oral tissue, such as a single-lens reflex camera, digital camera, camcorder, oral camera, and mobile phone.
8 The possibility of using mobile phones in dentoalveolar trauma has been suggested, however their quality and transmission performance have not been previously demonstrated under real conditions.
6-
8 One obstacle to capturing high-quality images of broken or damaged tooth structures is obstruction by the lips. This factor can be especially important in patients with vertical deficiency of the maxilla, who show less of their gums when laughing or smiling. Moreover, a patient will tend to move when retracting soft tissue due to fear, pain, and tenderness in the presence of trauma. Therefore, achieving acceptably good image quality requires the camera type and an optimized image-capture protocol to be specified.
We took frontal and occlusal images of six upper anterior teeth for the initial evaluation of dentoalveolar trauma. Most dental trauma occurs in the upper anterior teeth,
1,
2 that is, in two maxillary central incisors, two maxillary lateral incisors, and two maxillary canines. Evaluating traumatized teeth from two directions allows the dentist to tentatively diagnose the severity of dentoalveolar trauma. In the frontal view, our examiner checked the tooth structure, color of teeth, vertical level of teeth, gingival architecture, gingival bleeding, and adjacent soft tissues. In particular, a palatally deviated arrangement of teeth could be examined in the occlusal view. Increasing the number of images improved the ability of the dentist to perform a detailed and thorough analysis of the oral status, however this also increased the total file size and the number of files to be transmitted, which could adversely affect the image transmission due to failures or delays.
We investigated the effects of the camera functions on the image quality. The autofocusing was most significant for enhancing the image quality. Even in low-resolution images, having a definite outline of the dental tissue was crucial to the definitive diagnosis. The white-balance variable affected the color, and could be helpful in detecting the changes in tooth color and gingival bleeding. The automatic white-balance function could be most helpful for vivid image acquisition. The focal might could be another important factor. When a trauma incident would occur when a patient would be alone, the patient should take images of the teeth, during which the focal length might be important for ensuring appropriate focusing. Some mobile phones have two cameras: one for capturing distant objects and one for video calling; the latter camera would be more appropriate for urgent consultation due to the shorter focal length and ease of composition.
Image blurring is another important issue for quality assessment since making the correct diagnosis is impossible when the image is severely blurred. The shutter speed, optimal light source, and anti-movement function of camera would affect this parameter.
The image resolution affects both the image quality and transmission rate, since high-resolution images can facilitate diagnoses but are associated with larger files. Therefore, the optimal size of image file should be determined for successful transmission.
In conclusion, the possibility of using mobile phones in dentoalveolar trauma was introduced previously, however the optimal protocol for obtaining accurate diagnoses has not been proposed. This in-vitro study has revealed the following important protocol factors:
Both the frontal and occlusal images should be captured in order to show six upper anterior teeth.
The autofocusing and anti-movement functions of the in-built camera were useful for teledentistry for dentoalveolar trauma. Moreover, the automatic white-balance function was helpful for detecting the color changes.
The success rate and transfer times of transmissions depended on the total size of the image transfer, and not on the number of images or the addition of text messages.
The total image size should be limited to less than 500 kB to ensure rapid and successful image transfer.
These results were obtained in a limited in-vitro study. Further studies for more clinical protocols would be required to adopt the mobile phone in teleconsultations of real dentoalveolar trauma case.




 PDF
PDF ePub
ePub Citation
Citation Print
Print









 XML Download
XML Download