Abstract
Purpose
Diagnosis of osteoarthritis most commonly depends on clinical and radiographic findings. The present study attempted to observe the bony changes in temporomandibular joint (TMJ) patients from all age groups.
Materials and Methods
The first-visit clinical records and cone beam computed tomography (CBCT) data of 440 TMJs from 220 consecutive TMJ patients were reviewed retrospectively.
Results
The most frequent condylar bony change observed was sclerosis (133 joints, 30.2%) followed by surface erosion (129 joints, 29.3%), flattening of the articular surface (112 joints, 25.5%), and deviation in form (58 joints, 13.2%), which included 33 TMJs in a cane-shape, 16 with a lateral or medial pole depression, 6 with posterior condylar surface flattening, and 3 with a bifid-shaped condyle. Fifty-three joints (12.0%) showed hypoplastic condyles but only 1 joint showed hyperplasia. Osteophyte was found in 35 joints (8.0%) and subcortical cyst in 24 joints (5.5%), 5 of which had surface erosion as well. One hundred nineteen joints (27.0%) had only one kind of condylar bony change, 66 joints (15.0%) had two, 52 joints (11.8%) had three, 12 joints (5.0%) had four, and 6 joints (1.4%) had five kinds of condylar bony changes at the same time. Eighty-five (65.9%) of 129 joints with surface erosion had pain recorded at the chief complaint.
Osteoarthritis is thought by some to be unavoidable; almost everyone older than 50 years of age is affected to some extent. Although the temporomandibular joint (TMJ) is less affected by osteoarthritis than are heavy weight-bearing joints, TMJ osteoarthritis is found in 40% of older adults at microscopic and 14% at radiographic levels.1 However, although osteoarthritis is definitely an aging phenomenon, recent research has identified osteoarthritis in a majority of young patients referred to a TMJ clinic for joint pain and dysfunction.1 An autopsy study2 indicated that the signs of degenerative changes on the TMJ articular surfaces were found in 28% of the younger group (16 to 39 years of age) and in 50% of the older group (55 to 78 years of age). Zhao et al3 showed that radiographic TMJ osteoarthritic changes were common in adolescent and young adult patients younger than 30 years of age, especially in women, and the occurrence increased sharply between the ages of 11 to 19 years.
Diagnosis of osteoarthritis most commonly depends on the findings from clinical and radiographic examinations. The autopsy specimen study of Westesson et al4 found computed tomography (CT) to have a sensitivity of 0.75 and a specificity of 1.00 in diagnoses of bone changes with a positive predictive value of 1.0 and negative predictive value of 0.78. CT was superior to MRI in detection of osseous abnormalities. Guidelines from the RDC/TMD validation project5 recommend CT for use in both clinical and research settings. The relatively new technique of using CBCT has now become available. The advantage of this technique is the lower radiation dose to the patient compared with conventional CT. Hintze et al6 compared cone beam computed tomography (CBCT) with conventional tomography in detection of morphological TMJ changes, and in general, no significant differences in diagnostic accuracy were found between the two techniques. Since no evidence that conventional or CBCT is inferior to CT has been presented, the choice of imaging technique must depend on the available equipment.7
The osseous component analysis criteria for the condylar head of the validation project was gross hypoplasia or hyperplasia, flattening of the articular surface, subcortical sclerosis or cysts, surface erosion, osteophytes, generalized sclerosis, loose joint bodies, and deviation in form. In the present study, an attempt was made to check the distribution of these bony changes observed in TMJ patients from all age groups.
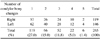
The first-visit clinical records and CBCT radiographic data of 440 TMJs from 220 consecutive TMJ patients (male 64, female 156 from 11 to 78 years, mean 29±16 years, Table 1) referred from a temporomandibular disorder clinic in the author's department were reviewed retrospectively. The condylar head was checked for hypoplasia or hyperplasia, flattening of the articular surface, subcortical sclerosis or cysts, surface erosion, osteophytes, generalized sclerosis, loose joint bodies, and deviation in form, and also condylar position was recorded following the guidelines from the RDC/TMD Validation Project.5 The chief complaints, including pain and/or noise, were reviewed to find any relationship with the radiographic changes. The CBCT images were taken by a Pax-Zenith 3D (Vatech Co., Hwaseong, Korea). The routine radiographic TMJ examination included 10-12 axial and coronal skull views showing the condylar heads, scout views of the midsagittal, and coronal views of each condyle, and 9 corrected sagittal and 4 coronal images for both sides. All images were directly interfaced with a PACS system (M-view, Infinitt Healthcare, Seoul, Korea) on a high resolution monochromatic monitor (MFGD 5421, Barco, Kortrijk, Belguim) of 2,048×2,560 image matrices and 145.9 ft-lambert luminescence.
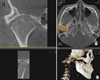
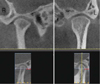
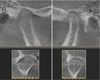
The most frequent change observed was the posterior position of the condyle in the sagittal plane (299 joints, 68.0%), followed by sclerosis (133 joints, 30.2%), including 15 joints showing totally generalized sclerosis (Fig. 1). Surface erosion was seen in 129 joints (29.3%), 5 of which had a subcortical cyst as well (Fig. 2). Flattening of the articular surface was observed in 112 joints (25.5%). Deviation in form were observed in 58 joints (13.2%), which included 33 cane-shapes (Fig. 3), 16 medial or lateral pole depressions (Figs. 4 and 5), 6 cases of posterior condylar surface flattening (Fig. 6), and 3 bifid-shaped condyles. Fifty-three joints (12.0%) showed hypoplastic condyles, but only 1 joint showed hyperplasia. Osteophytes were found in 35 joints (8.0%) and subcortical cysts in 24 joints (5.5%), 5 of which had surface erosion as well.
One hundred nineteen joints (27.0%) had only one condylar bony change, 66 joints (15.0%) had two, 52 joints (11.8%) had three, 12 joints (5.0%) had four, and 6 joints (1.4%) had 5 kinds of condylar bony changes at the same time (Table 2).
As for the clinical relationship with the radiographic changes of TMJ, 85 (65.9%) of the 129 joints with surface erosion had pain recorded as the chief complaint.
Osteoarthritis is considered a synonyms of osteoarthrosis, which is a non-inflammatory focal degenerative disorder of the synovial joints, primarily affecting the articular cartilage and sub-condylar bone and initiated by the deterioration of the articular soft-tissue cover and exposure of bone.8 This is a common degenerative and destructive alteration of joints that has been considered to be an inevitable result of simple wear and tear on aging anatomic structures until recently. It is now known to have a strong inflammatory component as well, especially in small joints, such as the TMJ, where there appears to be little association with the aging process.1 Larheim and Westesson8 commented that cases with evident inflammatory signs on MRI could be characterized as osteoarthritis, whereas joints without such signs could be characterized as osteoarthrosis.
Osteoarthritis seems like a deformation of bone since it shows subcortical cysts, surface erosion, osteophytes, and/or generalized sclerosis. However, more specific or detailed guidelines of diagnosis for osteoarthritis are now needed with the widespread use of CBCT.
The present study attempted to list as many types of bone change as possible in TMJ patients of all age groups. Although sclerosis was the most frequent condylar bony change in this study, it was not easy to identify definitively since it is usually a gradual bone-forming process. Sclerosis was, therefore, decided in this study when sclerotic change was clearly noticeable on the CBCT images. As for flattening, this study included only the flattening of the articular surface. However, flattening of the posterior, medial and lateral, and superior surfaces was also seen in the patients. The posterior surface of the condyles frequently showed flattening and even depression and erosion (Fig. 7) together with medial and lateral surfaces (Figs. 4 and 5). These changes were included in "deviation in form" in this study. In the case of the flattening of the superior surface of condyles, it was not apparently detected on the sagittal images even though it was detected easily on the coronal images (Fig. 8).
The prevalence of condylar bony changes in this study was lower than that found by Cevidanes et al.9 They observed condylar flattening in 60%, and osteoarthritic surface irregularities such as erosions and osteophytes in 40% of condyles in a painful TMJ osteoarthritis group. They also found that individual local morphologic variation in the left condyles revealed statistically significant positive correlation between the extent of resorption on certain condylar surfaces and pain intensity and duration. In this study, 85 (65.9%) of 129 joints with surface erosion had the records of pain as the patients' chief complaint.
Kurita et al10 found radiographic evidence of resorption in the lateral part of the mandibular condyle in 57 (32.0%) of 178 joints and reported that 22 of these had pain on digital palpation. Their study included bony surface erosion, concavity, or even flattening at the upper corner of the lateral part of the condyle. In the present study, 16 joints were observed to have medial (4) or lateral (12) pole depressions but if flattening were to be counted, the ratio would have increased, since there were many cases of flattening observed at these sites. Liu et al11 reported in their study that 63.0% of joints underwent disc perforation at the lateral part of the articular disc and explained that the likely cause was weakness of the lateral capsular attachment, whereas the medial capsular attachment was stronger and reinforced by the insertions of the lateral pteryoid muscle. On the other hand, Palconet et al12 reported that there was a poor correlation between condylar changes (as observed on CBCT images), pain, and other clinical signs and symptoms in TMJ osteoarthritis.
In conclusion, with more widespread use of CBCT, more specific or detailed guidelines for osteoarthritis are needed.
Figures and Tables
References
1. Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and maxillofacial pathology. 2002. 2nd ed. Philadelphia: Saunders;755.
2. Pereira FJ Jr, Lundh H, Westesson PL. Morphologic changes in the temporomandibular joint in different age groups. An autopsy investigation. Oral Surg Oral Med Oral Pathol. 1994. 78:279–287.
3. Zhao YP, Zhang ZY, Wu YT, Zhang WL, Ma XC. Investigation of the clinical and radiographic features of osteoarthrosis of the temporomandibular joints in adolescents and young adults. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011. 111:e27–e34.

4. Westesson PL, Katzberg RW, Tallents RH, Sanchez-Woodworth RE, Svensson SA. CT and MR of the temporomandibular joint: comparison with autopsy specimens. AJR Am J Roentgenol. 1987. 148:1165–1171.

5. Ahmad M, Hollender L, Anderson Q, Kartha K, Ohrbach R, Truelove EL, et al. Research diagnostic criteria for temporomandibular disorders (RDC/TMD): development of image analysis criteria and examiner reliability for image analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009. 107:844–860.

6. Hintze H, Wiese M, Wenzel A. Cone beam CT and conventional tomography for the detection of morphological temporomandibular joint changes. Dentomaxillofac Radiol. 2007. 36:192–197.

7. Petersson A. What you can and cannot see in TMJ imaging - an overview related to the RDC/TMD diagnostic system. J Oral Rehabil. 2010. 37:771–778.

8. Larheim TA, Westesson PL. Maxillofacial imaging. 2006. Berlin Heidelberg: Springer-Verlag;149.
9. Cevidanes LH, Hajati AK, Paniagua B, Lim PF, Walker DG, Palconet G, et al. Quantification of condylar resorption in temporomandibular joint osteoarthritis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010. 110:110–117.

10. Kurita H, Kojima Y, Nakatsuka A, Koike T, Kobayashi H, Kurashina K. Relationship between temporomandibular joint (TMJ)-related pain and morphological changes of the TMJ condyle in patients with temporomandibular disorders. Dentomaxillofac Radiol. 2004. 33:329–333.





 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download