Abstract
Purpose
Field of view and voxel resolution of cone beam computed tomography (CBCT) might affect the diagnostic capability. This study was performed to compare between the standard and HiRes zoom modes in the diagnosis of external root resorption (ERR) using CBCT.
Materials and Methods
Sixty three small cavities (0.25 mm depth and 0.5 mm diameter) were simulated on the buccal, lingual, and proximal surfaces at three different levels of 16 roots of teeth. After covering the root with nail varnish, the roots were inserted in the sockets and the model was placed in a water-containing lacuna. CBCT scans were taken in both standard and HiRes zoom modes using NewTom VG (QR srl Company, Verona, Italy). Then, an observer assessed the images to determine the presence or absence of the cavities. This process was repeated by increasing the size and depth of cavities to 0.5 mm depth and 1 mm diameter. Data were analyzed by McNemar test. The sensitivity, specificity, positive predictive value, negative predictive value, and likelihood ratio in evaluation of the simulated cavities were calculated.
Results
There was a significant difference between the two imaging modes in diagnosing the shallow cavities (p=0.02).The sensitivity of the standard zoom in detecting the shallow cavities was lower than that of the HiRes zoom. The likelihood ratio of the HiRes zoom was higher in the diagnosis of both cavity types.
Resorption is defined as the physiological or pathological resorption of dental tissue and substances secreted. Root resorption (RR) often results from chronic, long-term inflammation and sometimes it is a self-limiting process.1 External root resorption (ERR) is often diagnosed incidentally on check-up radiographs. Early diagnosis and treatment of RR may lead to prevention of the extensive loss of tooth structure and the resulting loss of the tooth.
Intraoral conventional radiographs is not considered as a reliable method for early diagnosis of ERR.2,3 In the evaluation of ERR, large irregular shape of radiolucency may be found on radiographs. The root canal is often visible with no breaks in continuity.1 In the diagnosis of RR, 51.9% of false-negative and 15.3% of false positive were estimated for conventional radiographs.4
Digital techniques such as a charge couple device (CCD) or photostimuable storage plate (PSP) are more reliable methods for detection of ERR in comparison with conventional radiographs.2,5 However, the accuracy of digital subtraction radiography (DSR) is controversial. Various studies proved its superior role,6,7 while others did not concur.4
Despite the usefulness of intraoral digital techniques, these techniques do not provide an accurate detection and localization of ERR especially when it occurs at buccal or lingual surface.4 Accurate diagnosis of the location and size of ERR would be the most important in designing treatment plan and predicting the prognosis of the treatment.
The diagnostic ability of computed tomography (CT) in evaluation of ERR was reported to show high sensitivity and specificity.8 However, CT should be cautiously used only for the limited cases of buccally or labially located ERR.8,9
New imaging systems such as cone-beam computed tomography (CBCT) have been introduced to the field of endodontics recently. There were several studies which confirmed the superiority and accuracy of CBCT in evaluating RR.10-14 Liedke et al reported that using a 0.3mm voxel resolution would be the best approach in diagnosing RR using CBCT with lower X-ray exposure.10
Few in vitro studies have been conducted on the effect of the field of view (FOV) and voxel size of CBCT in the diagnosis of RR. Accordingly, in this study, the experimental variables were including the ERR size and location, as well as the FOV and voxel resolution. Reducing the patient exposure and having the ability to detect ERR at an early stage were other advantageous achievements of this study.
In this study, a dry mandible with 13 remaining teeth or 16 roots of teeth was selected. After performing a hemisection of the mandibular molars, 16 roots were extracted from the dry mandible without causing significant injury to roots or bony sockets.
After extraction of the roots, 63 round cavities of 0.25 mm depth and 0.05 mm diameter were simulated in random distribution on the root surfaces while 21 cavities on each buccal, lingual, and proximal surfaces. The cavities were drilled by an endodontist, a co-investigator, using a high-speed round diamond bur. The numbers of cavities on each root were not the same but in random manner. A total of 21 cavities on each surface were also distributed evenly as seven cavities at three different levels, cervical, middle, and apical portions. The cavities on the root surface were randomly distributed. The root surface was covered by two layers of nail varnish. The roots were replanted into their sockets. The coronal portion of hemisection molars was fixed by melted wax. Then the digital radiographs using a PSP storage sensor (Digora Optime, Sordex, Helsinki, Finland) with exposure parameters of 70 kVp, 7 mA, 0.12 sec were taken from the different teeth to verify that the simulated cavities were not easily detectable. To reconstruct a soft tissue shadow and to avoid the disparities in density or image artifact, the model with a U-shaped water-containing lacuna fixed on a plexy plate was designed. In the center of the model, the mandible was fixed on the plate by wax layers. This complex was then set on the desk of NewTom VG (QR srl Company, Verona, Italy) CBCT equipment (Figs. 1A and B). Depending on the voxel resolution and FOV size, volumetric images were acquired using both HiRes (6-inch FOV, 0.125-0.150 mm voxel size) and standard (4-inch FOV, 0.200-0.240 mm voxel size) zoom modes.
Exposure parameters for the HiRes zoom mode were 110 kVp, 0.7 mA and 5.4 seconds. At first, two scout images, i.e. lateral and posterior-anterior views taken in accordance with the sample position were initially prepared and then a 360° scan was acquired. The total scan time was 18-20 seconds and the reconstruction time of the volumetric images was approximately four minutes. The above mentioned steps were repeated by the standard zoom with an exposure parameter of 110 kVp, 0.5 mA, and 3.6 seconds.
In order to reconstruct the study images taken from the volumetric ones, the plane was selected as it was parallel to the occlusal plan. Axial images with a thickness and an interval of 0.4 mm were prepared. Cross-sectional images with a thickness of 0.25 mm and an interval of 0.5 mm perpendicular to the mesio-distal and/or bucco-lingual axes (Fig. 2) were also prepared for each root. A maxillofacial radiologist, who was familiar with CBCT and had more than 10 years of professional work experience, participated in this study as an observer. This observer determined the absence or presence of cavities and their locations (i.e on the root surface and/or in the radicular third). The observer who was unaware of the study design and the distribution pattern of cavities evaluated both modes of CBCT images in separate sessions every two weeks to avoid the memory effect of repeated viewing. Overall in the first phase of the study, 126 cavities and 144 locations were evaluated. At the second stage, the roots were removed from their sockets and the previously applied nail varnish was cleaned from their surfaces. The depth and diameter of cavities were increased to a 0.5 mm depth and a 1 mm diameter. All of the previous steps were repeated.
The answers were considered as true only if the observer detected both the presence and the location correctly. Overall, 252 simulated cavities that included 126 shallow cavities and 126 deep cavities were evaluated. Relative frequencies of true answers results of the two imaging modes for the two kinds of cavities to be examined were reported. Two image modes (standard and HiRes zoom) were analyzed independently for determining cavity sizes (small and large) and detecting the location by the McNemar test. Overall, the McNemar test was used to compare the diagnostic ability of two different modes of CBCT for the detection of ERR cavities. The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and likelihood ratio (LR) were calculated. These diagnostic parameters were expressed with a 95% confidence interval (CI). The significance was determined at p<0.05. All statistical analyses were performed using SPSS for Windows (ver. 16.0, SPSS Inc., Chicago, IL, USA).
In this experimental study, 74.6% and 63.5% of the cavities were correctly identified in the HiRes mode and standard zoom, respectively. As well, the percentages of correct diagnoses of large cavities were 85.7% in the HiRes mode and 92.1% for standard zoom. Table 1 shows the ability of the two CBCT modes with their ability to recognize the size and location of ERR cavities accurately.
Table 2 shows the frequencies of making a correct identification in whether the ERR cavities are present or absent in both the standard and HiRes zoom imaging modes. There was a significant difference between these two imaging modes for the small cavities detection (p=0.02) but no significant difference for large cavities (p=0.25).
The McNemar test result showed that there was an association between the identification of two kinds of ERR cavities in each imaging mode (p<0.01 for standard zoom, p=0.3 for HiRes zoom).
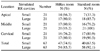
The diagnostic capability of CBCT scans to detect simulated root resorption was also tested. Table 3 shows the sensitivity and specificity, positive and negative predictive values (PPV and NPV respectively) as well as their LRs. Table 4 shows the sensitivity and specificity of CBCT for detection of ERR on different root surfaces and in each radicular third.
The comparison between both CBCT imaging modes used for identifying the ERR cavities located in the different radicular thirds and root surfaces is shown in Table 5.
This study evaluated two modes of CBCT with different voxel sizes, FOVs, image pixel sizes, and exposure parameters in the detection of simulated ERR. The prognosis of RR would depend on the location, size, and root surface involved. Early diagnosis would be advantageous to make a decision of appropriate time to start treatment and improve the success rate of treatment. Conventional radiography used in diagnosing RR, especially when small defects occur on buccal and lingual surfaces, has limitations and is not reliable.4,15,16
Previous studies9-14 showed that CBCT was very useful for the diagnosis of RR and it provided the possibility of proper management of ERR. In CBCT, the evaluation of root surface from different perspectives i.e. axial and cross-sectional views provides distinctive advantages of being able to determine the stage of RR more accurately, so that it can be possible to restore, arrest, and predict prognosis.
Esterla et al reported that internal RR was detected in all the cases using CBCT images; moreover, the extensions of the lesions were greater than 1-4 mm in 95.8% of their cases.14 The voxel resolution was 0.2 mm in their study. In our investigation, large ERR cavities were detected in 92.1% using the standard zoom mode and 85.7% using the HiRes zoom, respectively. Our study also concurred with the conclusions of previous investigations8-10,14 regarding the efficacy of CBCT in diagnosing RR.
The frequencies of correct diagnoses at the apical third in each mode and in each cavity size were higher than those of a study by da Silveira et al.8 The accuracy of determining a correct diagnosis in the middle and cervical thirds analyzed in our study was similar to their results.8 On the other hand, for the small cavities located in apical third, both of the chosen CBCT modes were more efficient than the multislice CT scan. It must be considered that RR cavities are difficult to diagnose.
The sensitivity in the detection of simulated ERR cavities located in the middle and cervical third was higher than that located in the apical third, similar to the da Silveira et al's study.8 The small diameter of the apical third in comparison with that of the middle and cervical thirds is described in our previously mentioned results.
The sensitivity of two different CBCT modes in the detection of simulated RR on the buccal surface was higher than that on the proximal portion and it was the same for the two types of the cavities. There was statistically significant difference between the standard and HiRes zoom modes in the detection of simulated RR at the apical third and on the lingual surface. Thus the HiRes zoom mode is suggested for detection of the most common RR site, the apical portion.
There was a significant difference in identifying the RR cavities between the two modes in terms of the association of resorption size with the radicular third. This finding was similar to the results by da Silveira et al.8
Imaging modes in our study was a high voxel resolution in both standard (0.2-0.24) and HiRes zoom modes (0.125-0.15). The voxel resolution in the Esterla et al's study14 was 0.2 mm while Liedke et al chose 0.2, 0.3, and 0.4mm voxel resolutions.10 In our study, the results of diagnostic performance tests revealed the similar values of the sensitivity and specificity among the cavities examined that had different voxel resolutions. However, the LR value of the HiRes zoom was higher than that of the standard zoom. This finding, in agreement with previous studies,10,14 confirmed the greater probability of correctly detecting cavities when the image was acquired by higher voxel resolutions. The difference between the exposure factors of two modes could be an effective factor on the image quality in addition to a voxel resolution.
In conclusion, two different modes of CBCT with various voxel sizes and fields of view showed high diagnostic accuracy. The HiRes zoom was more effective when it was used for small ERR cavities located in the apical third and on lingual surfaces.
Figures and Tables
Fig. 1
The photographs present the mandible that mounted in U-shaped water-containing lacuna fixed on a plexy plate and the setting of this complex onto the desk of CBCT device.

Fig. 2
Mesio-distal cross-sectional images reveal small external root resorption cavities on the right mandibular premolars and first molar tooth in the different locations in the HiRes zoom (arrows).

Acknowledgements
We are grateful to Julie Monti Safari for her assistance in editing the text. In addition, we would like to thank Mahtab Janzadeh for her assistance in gathering the sample data.
References
1. Hülsmann M, Schäfer E. Problems in endodontics; etiology, diagnosis and treatment. 2009. London: Quintessence;421–434.
2. Borg E, Källqvist A, Gröndahl K, Gröndahl HG. Film and digital radiography for detection of simulated root resorption cavities. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998. 86:110–114.

3. Chapnick L. External root resorption: an experimental radiographic evaluation. Oral Surg Oral Med Oral Pathol. 1989. 67:578–582.

4. Nance RS, Tyndall D, Levin LG, Trope M. Diagnosis of external root resorption using TACT (tuned-aperture computed tomography). Endod Dent Traumatol. 2000. 16:24–28.

5. Westphalen VP, Gomes de Moraes I, Westphalen FH, Martins WD, Souza PH. Conventional and digital radiographic methods in the detection of simulated external root resorption: a comparative study. Dentomaxillofac Radiol. 2004. 33:233–235.
6. Kravitz LH, Tyndall DA, Bagnell CP, Dove SB. Assessment of external root resorption using digital subtraction radiography. J Endod. 1992. 18:275–284.

7. Hintze H, Wenzel A, Andreasen FM, Sewerin I. Digital subtraction radiography for assessment of simulated root resorption cavities. Performance of conventional and reverse contrast modes. Endod Dent Traumatol. 1992. 8:149–154.

8. da Silveira HL, Silveira HE, Liedke GS, Lermen CA, Dos Santos RB, de Figueiredo JA. Diagnostic ability of computed tomography to evaluate external root resorption in vitro. Dentomaxillofac Radiol. 2007. 36:393–396.
9. Kim E, Kim KD, Roh BD, Cho YS, Lee SJ. Computed tomography as a diagnostic aid for extracanal invasive resorption. J Endod. 2003. 29:463–465.

10. Liedke GS, da Silveira HE, Silveira HL, Dutra V, de Figueiredo JA. Influence of voxel size in the diagnostic ability of cone beam tomography to evaluate simulated external root resorption. J Endod. 2009. 35:233–235.

11. Patel S, Dawood A, Wilson R, Horner K, Mannocci F. The detection and management of root resorption lesions using intraoral radiography and cone beam computed tomography - an in vivo investigation. Int Endod J. 2009. 42:831–838.
12. Hahn W, Fricke-Zech S, Fricke J, Gruber RM, Dullin C, Zapf A, et al. Detection and size differentiation of simulated tooth root defects using flat-panel volume computerized tomography (fpVCT). Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009. 107:272–278.

13. Nakata K, Naitoh M, Izumi M, Ariji E, Nakamura H. Evaluation of correspondence of dental Computed Tomography imaging to anatomic observation of external root resorption. J Endod. 2009. 35:1594–1597.

14. Estrela C, Bueno MR, De Alencar AH, Mattar R, Valladares Neto J, Azevedo BC, et al. Method to evaluate inflammatory root resorption by using cone beam computed tomography. J Endod. 2009. 35:1491–1497.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download