Abstract
Radicular cyst is the most common odontogenic cyst occurring in the jaws. The cyst is commonly found in relation to the maxillary anterior teeth in the third and fifth decade of life. Although multiple radicular cysts are not uncommon in the jaws, bilaterally symmetrical representation of these cysts is rare. Radiographs prior to extraction help in diagnosis of these cysts and thereby prevent further morbidities. We report a case of 16-year-old male patient who presented bilateral radicular cysts symmetrically in the mandible.
Jaw bones are host to a wide variety of cysts and neoplasms due in large part to the tissues involved in tooth formation.1 Cysts can present as functional disturbances caused by bone remodeling and weakening or after a secondary infection.2 Cysts in the jaws, of both odontogenic and non-odontogenic origin, can exhibit a biologically aggressive course and can be diagnostically difficult. Radicular cysts are common inflammatory odontogenic cysts of the jaws comprising of 52-68% of all cysts of the jaws and arising in the periodontal ligament space from the epithelial residues following pulpal necrosis.3 Differentiating radicular cysts from other lesions could be challenging if the clinical presentation and radiographic appearance is unusual thereby making differential diagnosis important. Even though radicular cysts are one of the common lesions in the jaws, multiple radicular lesions are relatively rare. Multiple cystic lesions in the jaws should be considered as keratocystic odontogenic tumor. Here, we report multiple cystic lesions that occurred bilaterally in the mandible.
A 16-year-old male patient reported to our department with a chief complaint of swelling in the right posterior region in the mandible for the previous two months. The patient reported a history of a huge swelling in the same region associated with fever and pain of a pricking intermittent type around two months earlier. The patient had consulted his doctor, who had prescribed him antibiotic and analgesic medication and an incision and drainage procedure had been performed emergently. Subsequently, the patient had been recalled for extraction of the offending tooth, however he did not continue with any more treatment.
The patient had swelling without any fever and occasional pain just from touching the region. He did not take any medication, and had no functional difficulties or paresthesia associated with the swelling. On extraoral examination, a diffuse swelling was present on the right side of his face, measuring approximately 2 cm×2 cm, and the skin over the swelling appeared normal with no secondary changes. On palpation, there was mild local heat and swelling, which was bony hard, non-tender with expansion of the buccal cortical plate bilaterally (Fig. 1). Intraorally, a small well-defined swelling was present on the alveolar mucosa corresponding to the periapical region of the right mandibular first molar measuring 1 cm×1 cm, with pus discharge (Fig. 2). The swelling was tender and soft in consistency. Based on the clinical history and examinations, the provisional diagnosis was chronic periapical abscess in relation to the root stump of the mandibular first molar. Adjacent teeth were found to be vital on electric pulp testing.
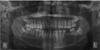
An intraoral periapical radiograph revealed a large well-defined radiolucency whose entire extent was not visible on the radiograph, therefore a panoramic radiograph was taken subsequently, which revealed a large unilocular radiolucency bilaterally in relation to the mandibular first molar and the retained root of the left mandibular first molar. Both the radiolucencies were well corticated and showed no internal trabeculae. There was displacement of the adjacent teeth and the involved teeth showed slight root resorption (Fig. 3). A mandibular cross sectional occlusal radiograph revealed buccal cortical expansion bilaterally along with trabeculation present at the periphery of the lesion (Fig. 4).
Based on the radiographic findings, the differential diagnoses of radicular cyst, multiple odontogenic keratocyst associated with nevoid basal cell carcinoma syndrome, bilateral central giant cell granuloma, brown's tumor associated with hyperparathyroidism, and unicystic ameloblastoma were considered.
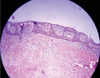
On surgical enucleation and extraction of the tooth, the specimen was subjected to histopathological examination, which revealed non-keratinizing epithelium of variable thickness exhibiting an arcading pattern and connective tissue wall consisting of moderately collagenous with dense inflammatory infiltrate predominantly plasma cells and lymphocytes. These findings were suggestive of radicular cyst (Fig. 5).
Radicular cyst commonly occurs in the maxillary anterior region in the third to fifth decade of life, more commonly in men.3 There may be a slow growing bony swelling or it may be asymptomatic, and this lesion can be discovered unexpectedly on periapical radiographs as in the present case. As the cyst increases in size, the covering bone becomes very thin despite subperiosteal bone deposition and the swelling then exhibits 'springiness' and when the cyst has completely eroded the bone, there will be fluctuation.4 In our case, there was no fluctuation, but only expansion at the lower border of the mandible which excluded the diagnosis of a cyst. A main feature in the diagnosis of a radicular cyst is the related presence of a tooth with non-vital pulp and sometimes a sinus may lead from the cyst cavity, which was seen in the present case.4 Though radicular cysts are considered a sequel to periapical granuloma only a small fraction of the periapical granulomas advance to become cysts.5 Radicular cysts appear as round or pear-shaped unilocular radiolucent lesions surrounded by a thin radiopaque margin, extending from the lamina dura of the involved tooth and may displace adjacent teeth or cause mild root resorption. A lesion larger than 2 cm is more likely to be a cyst than a granuloma.4,6,7
Keratocystic odontogenic tumors are most commonly located in the mandibular ramus and body.8 These lesions are typically found in young adults in the second to fourth decades of life and represent 5-17% of all jaw cysts similar to our case.9 Approximately 5% of patients with odontogenic keratocyst have multiple jaw cysts not associated with any syndrome. The presence of multiple keratocystic odontogenic tumors, however, should suggest the possibility of basal cell nevus syndrome (i.e., Gorlin-Goltz syndrome).8 The other features of this autosomal-dominant disorder include midface hypoplasia, frontal bossing, mental retardation, calcification of the falx cerebri and dura, bifid ribs, and multiple basal cell carcinomas of the skin, none of which were found in this case.10 Radiographically, keratocystic odontogenic tumors may be unilocular or multilocular and they typically extend into the marrow cavity with smooth border contributing to mild bulging of the cortex but without significant cortical expansion as seen similarly in the present case. Keratocystic odontogenic tumors can show a more aggressive growth pattern including cortical expansion, tooth and mandibular canal displacement, and root resorption as seen this case, although other features like extrusion of erupted teeth and perforation of the cortical bone were not present.11
Central giant cell granuloma is believed to be a single lesion in a spectrum of altered vascular and reactive responses within bone.10 The lesion most frequently occurs in girls and young women during the second and third decades of life and is found in the anterior mandible.10 Bilateral central giant cell lesions are also associated with Noonan syndrome characterized by congenital heart defects, short stature, broad or webbed neck, hypertelorism, downward slanting eyes, coarse curly hair, pectus excavatum (depressed sternum), and so on. Since our patient was apparently normal, no association with of any kind of syndrome could be made.12 Radiographically, initially, a giant cell reparative cyst manifests as a small, unilocular radiolucent lesion, however, later, with development, the lesion becomes multilocular, along with expansion of the jaw, root resorption, and erosion. The lesion may cross the midline of the mandible which was not seen in the present case.10 Since non-syndromic type bilateral occurrence of a giant cell lesion was also reported, this lesion was still considered under differential diagnosis.13
Brown tumor of hyperparathyroidism is also a central giant cell lesion caused by long-standing primary or secondary hyperparathyroidism and has no neoplastic potential.12,14 The lesion develops as a result of intra-osseous bleeding and tissue degeneration, and the presence of hemosiderin within the cystic spaces leads to the brownish color, which is responsible for the name. These bony tumors are most commonly found in the trabecular portion of the long bones, pelvis, ribs, and jaw, although the mandible is also a common site for occurrence of multiple brown tumors. However, other associated changes such as decreased density of the jaw, granular texture of the bony trabeculae, and loss of the lamina dura along with biochemical parameters such a lack of hypercalcemia, hypophosphatemia, and elevated parathyroid hormone in blood levels excluded any endocrine abnormalities associated with the lesion.12,15
Ameloblastoma is a benign but locally aggressive epithelial odontogenic tumor. It can be grouped into four main forms; multicystic, unicystic, extraosseous or peripheral, and desmoplastic.16 Approximately 5% of unilocular ameloblastomas arise from the epithelial lining of dentigerous cysts, and bilateral occurrence of non-syndromic type of dentigerous cyst has also been reported which led us to consider this tumor in our differential diagnoses.13,17 Unicystic ameloblastoma and dentigerous cyst commonly occur in a younger age group.18 Common radiographic findings of the unicystic variant include a unilocular, well-corticated radiolucent lesion often associated with the crown of an unerupted or impacted tooth. The presence of solid components, including internal bony septa, would be helpful for differential diagnosis between ameloblastoma and dentigerous cyst.19 Since there was no impacted tooth in the present case, an occurrence of unicystic bilateral ameloblastoma was ruled out.
This report highlighted the occurrence of symmetrical radiolucent lesions in the jaw, showing the importance of radiographic differential diagnosis and reinforceing the role of radiographs prior to the extraction of teeth. Moreover, untreated radicular cysts could lead to a great deal of morbidity including ameloblastoma or squamous cell carcinoma.2,20
Figures and Tables
 | Fig. 3Mandibular occlusal radiograph shows bilateral cortical expansion along with trabeculation seen at the periphery of the lesion. |
References
1. Regezi JA. Odontogenic cysts, odontogenic tumors, fibroosseous, and giant cell lesions of the jaws. Mod Pathol. 2002. 15:331–341.

2. Devenney-Cakir B, Subramaniam RM, Reddy SM, Imsande H, Gohel A, Sakai O. Cystic and cystic-appearing lesions of the mandible: review. AJR Am J Roentgenol. 2011. 196:WS66–WS77.
3. Joshi NS, Sujan SG, Rachappa MM. An unusual case report of bilateral mandibular radicular cysts. Contemp Clin Dent. 2011. 2:59–62.

4. Shear M, Speight PM. Cysts of the oral and maxillofacial regions. 2007. 4th ed. Oxford: Blackwell;123–141.
5. Bhaskar SN. Oral surgery - oral pathology conference No. 17, Walter Reed Army Medical Center. Periapical lesions - types, incidence, and clinical features. Oral Surg Oral Med Oral Pathol. 1966. 21:657–671.
6. Syrjänen S, Tammisalo E, Lilja R, Syrjänen K. Radiological interpretation of the periapical cysts and granulomas. Dentomaxillofac Radiol. 1982. 11:89–92.

7. Regezi JA, Sciubba JJ, Jordan RC. Oral Pathology: clinical pathologic correlations. 2003. 4th ed. St Louis: WB Saunders;241–254.
8. González-Alva P, Tanaka A, Oku Y, Yoshizawa D, Itoh S, Sakashita H, et al. Keratocystic odontogenic tumor: a retrospective study of 183 cases. J Oral Sci. 2008. 50:205–212.

9. Theodorou SJ, Theodorou DJ, Sartoris DJ. Imaging characteristics of neoplasms and other lesions of the jawbones: part 1. Odontogenic tumors and tumorlike lesions. Clin Imaging. 2007. 31:114–119.
10. Dunfee BL, Sakai O, Pistey R, Gohel A. Radiologic and pathologic characteristics of benign and malignant lesions of the mandible. Radiographics. 2006. 26:1751–1768.

11. Hegde S, Shetty SR. Radiological features of familial Gorlin-Goltz syndrome. Imaging Sci Dent. 2012. 42:55–60.

12. Edwards PC, Fox J, Fantasia JE, Goldberg J, Kelsch RD. Bilateral central giant cell granulomas of the mandible in an 8-year-old girl with Noonan syndrome (Noonan-like/multiple giant cell lesion syndrome). Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005. 99:334–340.

13. Ofluoglu D, Ertas B, Basarer N, Ergun S, Bilgic B, Tanyeri H. OC1 Bilateral central giant cell granuloma of the mandible: a case report. Oral Dis. 2006. 12:10.

14. Neyaz Z, Gadodia A, Gamanagatti S, Mukhopadhyay S. Radiographical approach to jaw lesions. Singapore Med J. 2008. 49:165–177.
15. Jebasingh F, Jacob JJ, Shah A, Paul TV, Seshadri MS. Bilateral maxillary brown tumours as the first presentation of primary hyperparathyroidism. Oral Maxillofac Surg. 2008. 12:97–100.

16. Sham E, Leong J, Maher R, Schenberg M, Leung M, Mansour AK. Mandibular ameloblastoma: clinical experience and literature review. ANZ J Surg. 2009. 79:739–744.

17. Freitas DQ, Tempest LM, Sicoli E, Lopes-Neto FC. Bilateral dentigerous cysts: review of the literature and report of an unusual case. Dentomaxillofac Radiol. 2006. 35:464–468.

18. Gardner DG. Plexiform unicystic ameloblastoma: a diagnostic problem in dentigerous cysts. Cancer. 1981. 47:1358–1363.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download