Abstract
Purpose
The purpose of this study was to evaluate the diagnostic performance of dental students in detection of mandibular condyle fractures and the effectiveness of reference panoramic images.
Materials and Methods
Forty-six undergraduates evaluated 25 panoramic radiographs for condylar fractures and the data were analyzed through receiver operating characteristic (ROC) analysis. After a month, they were divided into two homogeneous groups based on the first results and re-evaluated the images with (group A) or without (group B) reference images. Eight reference images included indications showing either typical condylar fractures or anatomic structures which could be confused with fractures. Paired t-test was used for statistical analysis of the difference between the first and the second evaluations for each group, and student's t-test was used between the two groups in the second evaluation. The intra- and inter-observer agreements were evaluated with Kappa statistics.
Results
Intra- and inter-observer agreements were substantial (k=0.66) and moderate (k=0.53), respectively. The area under the ROC curve (Az) in the first evaluation was 0.802. In the second evaluation, it was increased to 0.823 for group A and 0.814 for group B. The difference between the first and second evaluations for group A was statistically significant (p<0.05), however there was no statistically significant difference between the two groups in the second evaluation.
Fractures of condylar process of mandible are common injuries that account for 20-62% of all mandibular fractures.1 The diagnosis of the mandibular condyle fractures is based on clinical and radiographic examinations. Clinical signs such as jaw deviation, mouth opening limitation, malocclusion, and edema of the preauricular region can be indicative of fractures of the condylar process.2 The accuracy of physical examination is only 68% of mandibular fractures,3 therefore radiographic evaluation is essential to confirm the presence and location of the mandibular fractures.
Computed tomography (CT) is considered as a gold standard for the radiographic evaluation of fractures of the mandibular condyle process.4,5 It reveals bony and soft tissue changes at the same time and allows multi-planar evaluation.6,7 However, the routine use of CT for mandibular fractures is not justified due to the high cost and increased radiation exposure.
Panoramic radiograph provides a good view of the entire mandible including the condylar region, therefore it is commonly used by many clinicians as an ideal screening view for mandibular fractures.8-10 Condylar region is one of the most difficult areas to detect fractures, especially for many clinicians who do not have much experience of interpreting mandibular fractures.11 The failure to recognize the presence of a condylar fracture, especially in children may lead to late complications including facial deformity and temporomandibular joint ankylosis.5,12 There were previous studies that the sensitivity of panoramic radiography in diagnosing mandibular condylar fractures ranged from 70 to 90%.5,11,13 Lee et al observed that clinicians with less experience tended to miss more fractures than those with more experience.11
The hypothesis was that providing reference images showing either typical condylar fractures or normal anatomic structures mimicking fractures might improve the diagnostic accuracy for the inexperienced.
The purpose of this study was to evaluate the diagnostic performance of dental students in detection of mandibular condyle fractures and the effectiveness of reference panoramic images.
From the Oral and Maxillofacial archives of Pusan National University Hospital, one oral and maxillofacial radiologist and one oral and maxillofacial surgeon with more than 10 years of experience reviewed CT and panoramic images of patients suspected of having uncomplicated mandibular condylar fractures.
A total of 25 panoramic radiographs were selected for this study. The inclusion criteria were as follows: 1. The 2 assessment panels were in complete agreement on the presence or absence of the condylar fracture. 2. All panoramic radiographs were of acceptable quality and had no other jaw disease.
The study population comprised 18 males and 7 females and the mean age was 35.2 (9-74 years old). Out of 25 panoramic radiographs, 16 radiographs showed unilateral condylar fracture, 6 bilateral fractures, and 3 no fracture. The data of the patients' gender, age, diagnosis, type of fracture, and displacement of the fracture were recorded. The classification of the fractures was determined using panoramic and CT images. The condylar fractures were grouped into head, neck, and subcondylar fractures by the location and also classified by the type of displacement as suggested by Yamaoka et al.14 The assessment panels' diagnosis was regarded as a gold standard for confirming condylar fractures.
Digital panoramic radiographs were taken using PM 2002 CC Proline (Planmeca Oy, Helsinki, Finland) with the standard panoramic program. The panoramic equipment was set at 62-64 kVp, 5-6 mA, and 18 seconds of exposure time.
All CT scans were performed with a multi-detector CT (Somatom Definition AS+, Siemens Medical Systems, Erlangen, Germany) and imaging parameters were as follows: 120 kVp, 230-250 mAs, 3 mm pitch, 0.5 mm interval and slice thickness 1.3-2.5 mm.
The panoramic radiographs were shown to 50 dental students in their final year. All images were directly interfaced onto a PACS system (M-view, Infinitt Healthcare, Seoul, Korea) on monitors (MFGD 5421, Barco, Kortrijk, Belgium) of 2,048×2,560 image matrices and 145.9-ft-lambert luminescence. All students were blind to the clinical information of the subjects imaged. Each assessor was asked to record the presence or absence of fracture by both a simple 'yes' or 'no' for sensitivity analysis and a 5-point scale for Receiver Operating Characteristic (ROC) analysis: 1-fracture definitely absent; 2-fracture probably absent; 3-unsure whether fracture is present; 4-fracture probably present; 5-fracture definitely present.
After the first assessment, the sensitivity and ROC area were calculated. ROC analysis was performed by MedCalc version 6.0 (MedCalc Software, Mariakerke, Belgium). Four students showing markedly deviated ROC area (>mean±2 SD) from other students were eliminated as outliers. Using the first assessment results, the assessors were divided into two homogenous groups having the same mean and SD, and each group was composed of 23 students.
A minimum of 4 weeks later, the students performed the second viewing session. For group A (reference group), Eight panoramic radiographs were provided as reference images during the second assessment. The images were indicated with arrows noting either typical condylar fracture or normal structures which could be confused with fractures. Figs. 1 and 2 show examples of reference images. Group B (no reference group) evaluated the images in random order in the same way as the first session. There was no additional training or education for both groups.
The difference between the first and the second evaluations within each group was analyzed by means of a paired t-test and the difference between the two groups in the second evaluation by student's t-test using SPSS 11.0 for Windows software (SPSS Inc, Chicago, IL). P-values less than 0.05 were considered statistically significant.
Kappa statistics were computed to assess the intra- and inter-observer agreement.15 For agreement within the observers, the data from the first and second assessments of group B were used, and for the agreement between the observers, the data from the first assessment of group A and B were used. Kappa statistics are commonly interpreted as <0.00, poor agreement; 0.00 to 0.20, slight agreement; 0.21 to 0.40, fair agreement; 0.41 to 0.60, moderate agreement; 0.61 to 0.80, substantial agreement; and 0.81 to 1.00, almost perfect agreement.
The distribution of the condylar fractures is listed in Table 1. There were 5 condylar head fractures, 14 neck fractures, and 9 subcondylar fractures. The overall sensitivity was 0.81. The sagittal splitting fracture of condylar head showed the lowest sensitivity. Kappa analysis showed substantial (k=0.66) agreement within observers and moderate (k=0.53) agreement among observers.
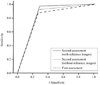
Table 2 and Fig. 3 show the area under ROC curve. Both groups showed higher diagnostic performance in the second assessment than in the first assessment. Statistically significant difference was shown in group A (reference group) and total assessors (p<0.05), however in group B (no reference group), there was no statistically significant difference. Also, the difference of the diagnostic performance between the groups in the second evaluation was not statistically significant.
Panoramic radiography is superior to other conventional radiography and it is adequate in evaluating mandibular fractures.8,9,16 With the growing use of the panoramic radiography, the occasions for general dentists to diagnose mandibular fractures have been increasing. It was reported that clinicians with no experience in the field of fracture showed a relatively low diagnostic performance in the detection of condylar fracture.11 This study was performed to explore the possibility of the use of reference images to increase the diagnostic ability.
In this study, the students in their last year of dental school, who have limited experience in this field participated as assessors. They had finished two hours of the lecture on facial trauma 4 months before, and no other additional education was given. Having been in the course of clinical patient care program over a year, they were familiar with panoramic radiograph.
The students showed the overall sensitivity of 80.9%. It was fairly good, considering the previous report that the sensitivity of the general dentists was 80% or under. It means that they had a considerable knowledge on the fracture interpretation. The mandibular condyle is considered as one of the most difficult regions to detect fractures,5,9,17,18 and this is especially true for the sagittal splitting fracture of the condylar head. This study showed that the sensitivity of the condylar fractures was different according to the location of the fractures. The sensitivity of the sagittal splitting fracture was only 50%, while that of condylar neck was over 90%. For the subcondyle, the shadow of the soft palate and pharyngeal wall was often mistaken as fractures, resulting in relatively low sensitivity. Lee et al stated that condylar fracture was the most common facial fracture in children, and if undiagnosed in a child, it might not become apparent until further growth.19 The undiagnosed and untreated condylar fractures in children might show facial growth disturbance and asymmetry.12,20 Temporomandibular joint disorders such as ankylosis and dysfunction and malocclusion might also occur.19,21 Therefore, Chacon et al recommended additional CT examination in the assessment of children suspected to have fractures of the mandibular condyle.5
The diagnostic accuracy of condylar fractures was measured by the area under the ROC curve. With or without the reference images, both groups showed improved the diagnostic performance in the second assessment. Statistically significant difference was shown in the reference group and in total assessors, however not in the group without the reference images. It is understandable that the supplementary reference images would contribute to identification of condylar fractures. However, contrary to expectations, there was no statistically significant difference between the groups in the second evaluation. Even though it was not high enough to show the statistically significant difference, no reference group also showed the increased diagnostic performance in the second evaluation compared with the first evaluation, and the difference between the groups became indistinct. The diagnostic outcome can be improved by training and education. It can be postulated that the first assessment session played as a self-education, and the diagnostic performance of the no reference group in the second assessment session showed improvement, however still not getting higher sensitivity than the reference group.
In conclusion, this study suggests that providing reference images to less experienced clinicians could improve the diagnostic ability in detecting condylar fracture, and along with it, it might be helpful to give a chance of additional education.
Figures and Tables
Fig. 1
Panoramic (A) and cone beam CT (B) images show sagittal splitting (white arrow) and condylar neck (black arrow) fracture.
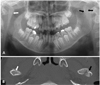
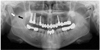
Fig. 2
Panoramic image shows soft palate (thick white arrow), subcondylar fracture (thick black arrow), spine of sphenoid bone (thin black arrow), and pharyngeal wall (thin white arrow).
References
1. Buchbinder D. Treatment of fractures of the edentulous mandible, 1943 to 1993: a review of the literature. J Oral Maxillofac Surg. 1993. 51:1174–1180.

3. Thai KN, Hummel RP 3rd, Kitzmiller WJ, Luchette FA. The role of computed tomographic scanning in the management of facial trauma. J Trauma. 1997. 43:214–218.

4. Roth FS, Kokoska MS, Awwad EE, Martin DS, Olson GT, Hollier LH, et al. The identification of mandible fractures by helical computed tomography and panorex tomography. J Craniofac Surg. 2005. 16:394–399.

5. Chacon GE, Dawson KH, Myall RW, Beirne OR. A comparative study of 2 imaging techniques for the diagnosis of condylar fractures in children. J Oral Maxillofac Surg. 2003. 61:668–673.

6. Raustia AM, Pyhtinen J, Virtanen KK. Examination of the temporomandibular joint by direct sagittal computed tomography. Clin Radiol. 1985. 36:291–296.

7. Christiansen EL, Thompson JR, Hasso AN. CT evaluation of trauma to the temporomandibular joint. J Oral Maxillofac Surg. 1987. 45:920–923.

8. Chayra GA, Meador LR, Laskin DM. Comparison of panoramic and standard radiographs for the diagnosis of mandibular fractures. J Oral Maxillofac Surg. 1986. 44:677–679.

10. Reiner SA, Schwartz DL, Clark KF, Markowitz NR. Diagnostic ability of panoramic radiography for mandibular fractures. Arch Otolaryngol Head Neck Surg. 1989. 115:1083–1085.
11. Lee JH, Jung YH, Cho BH, Hwang DS. Diagnostic ability of panoramic radiography for mandibular fractures. Korean J Oral Maxillofac Radiol. 2010. 40:33–38.
12. Zachariades N, Mezitis M, Mourouzis C, Papadakis D, Spanou A. Fractures of the mandibular condyle: a review of 466 cases. Literature review, reflections on treatment and proposals. J Craniomaxillofac Surg. 2006. 34:421–432.

13. Wilson IF, Lokeh A, Benjamin CI, Hilger PA, Hamlar DD, Ondrey FG, et al. Prospective comparison of panoramic tomography (zonography) and helical computed tomography in the diagnosis and operative management of mandibular fractures. Plast Reconstr Surg. 2001. 107:1369–1375.

14. Yamaoka M, Furusawa K, Iguchi K, Tanaka M, Okuda D. The assessment of fracture of the mandibular condyle by use of computerized tomography. Incidence of sagittal split fracture. Br J Oral Maxillofac Surg. 1994. 32:77–79.

16. Moilanen A. Primary radiographic diagnosis of fractures in the mandible. Int J Oral Surg. 1982. 11:299–303.

17. Wilson IF, Lokeh A, Benjamin CI, Hilger PA, Hamlar DD, Ondrey FG, et al. Contribution of conventional axial computed tomography (nonhelical), in conjunction with panoramic tomography (zonography), in evaluating mandibular fractures. Ann Plast Surg. 2000. 45:415–421.

18. Assael LA. Clinical aspects of imaging in maxillofacial trauma. Radiol Clin North Am. 1993. 31:209–220.

19. Lee CY, McCullon C 3rd, Blaustein DI, Mohammadi H. Sequelae of unrecognized, untreated mandibular condylar fractures in the pediatric patient. Ann Dent. 1993. 52:5–8.
20. Rowe NL. Fractures of the facial skeleton in children. J Oral Surg. 1968. 26:505–515.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download