Abstract
Arteriovenous malformations are extremely rare conditions in that can result from abnormalities in the structure of blood vessels, which may be potentially fatal. A 30-year-old female patient visited our hospital with a complaint of swelling on the right maxillary posterior gingiva along with the large port-wine stain on right side of face. On clinical examination, the swelling was compressible and pulsatile. Radiographic examination revealed a lytic lesion of maxilla. Diagnostic angiography revealed a high-flow arteriovenous malformation of maxilla which was treated by selective transarterial embolization of maxillary artery using polyvinyl alcohol particles.
Vascular anomalies are soft tissue lesions of congenitally aberrant blood vessel growth that affect up to 10% of newborns.1 Vascular anomalies are divided into two main categories: vascular tumors and vascular malformations.1,2
The vascular tumors mainly include hemangiomas. They are made up of rapidly proliferating endothelial cells. The blood vessel architecture is incomplete and surrounded by hyperplastic cells in these tumors. Clinically, hemangiomas usually appear in early infancy, grow rapidly during the first 18-24 months of life and slowly involute over the next 5 or 6 years. In contrast, vascular malformations consist of progressively enlarging aberrant and ectatic vessels of particular vascular architecture such as arteries, veins, lymphatic vessels.
The vascular malformations are further subdivided into low-(slow) and high-(fast) flow lesions based upon the velocity of fluid motion through their system. Capillary, venous, and lymphatic malformations are considered low-flow malformations while arteriovenous malformations (AVMs) have fast-flow characteristics. Unlike hemangiomas, vascular malformations are uncommon, rarely regress, continue to expand, and have high rates of recurrence following intervention.3-5
Approximately 51% of vascular malformations occur in the head and neck region, and the male-to-female ratio is 1 : 1.5.3 Extracranial AVMs of the head and neck (extracranial) are high-flow lesions and among the most serious of the vascular malformations because they are difficult to diagnose, treat, and cure. They grow throughout life with frequent, dramatic, and aggressive growth spurts under various environmental influences. AVMs are very destructive, infiltrative and often life-threatening secondary to massive bleeding. Most common areas of occurrence are the cheek, lips, neck, scalp, neck, ear, tongue, and mandible.1 Signs and symptoms reported are commonly soft tissue swelling, pain of variable intensity, teeth mobility and migration, discoloration of overlying skin and intraoral mucosal surface, paresthesia, facial asymmetry, local pulsations, bruits, erythematous gingivae and bleeding around the teeth, and bone resorption with palpable thrill as well as resorption of the roots in the affected area with no evidence of related cause or periapical pathoses.6
Various treatment modalities have been discussed for the management of AVM.7,8 Many studies have reported the use of selective transarterial embolization of AVM with various substances.6,9,10 This may be followed by surgical resection or sclerotherapy. Here we report a case in which high flow AVM of maxilla was imaged using angiography. The angiogram revealed the feeder vessel which was branch of internal maxillary artery. Selective transarterial embolization of the feeder artery was performed using polyvinyl alcohol particles.
A 30-year-old female patient reported to the outpatient department of Vasantdada Patil Dental College and Hospital, Sangli with a chief complaint of gingival swelling on the right maxillary posterior region. The patient noticed a painless swelling 6 months ago, which was small in size initially, started growing gradually and reached the present size. The patient revealed a history of similar swelling in the same region 2 years ago. Surgical removal of the mass had been attempted, however it had been unsuccessful due to heavy bleeding from the site. The bleeding had been controlled by cauterization.
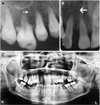
On general examination, the patient showed unilateral port-wine stain on the right side of her face extending from the superior border of the upper lip to the bridge of the nose superoinferiorly and from the midline to the preauricular region anteroposteriorly since her birth. On clinical examination, the patient revealed about 3×3 cm sized solitary extraoral swelling on the right maxilla extending from the midline to the midpupilary line anteroposteriorly and from the superior border of the upper lip to the base of the nose superoinferiorly. The swelling was roughly ovoid in shape with diffuse borders. The overlying skin was erythematous. There was a local increase in temperature of the overlying skin. The swelling was soft in consistency and non-tender on palpation. Intraorally, about 3×6 cm sized solitary swelling, reddish pink in color was found extending from the right central incisor to the third molar on the buccal and palatal gingivae of the maxilla. The swelling involved marginal, papillary, and attached gingivae, and had smooth surface. It was soft in consistency, non-tender on palpation, compressible, pulsatile and blanched on pressure. No bleeding on palpation was noted. The right maxillary first and second premolars showed grade II mobility. The right maxillary lateral incisor was displaced laterally (Fig. 1). A provisional diagnosis of vascular lesion was given and the patient was subjected to radiographic examination. Intraoral periapical radiographs showed coarse bony trabeculae and enlarged marrow spaces on the right maxillary anterior and posterior regions. Alveolar bone loss was revealed on the maxillary central and lateral incisor regions. Widening of periodontal ligament space was seen with lateral incisor, first and second premolar and the first molar was supraerupted (Figs. 2A and B). Panoramic radiograph showed ill-defined, irregular area of bone destruction extending from the mesial surface of the left maxillary central incisor upto the mesial surface of the right maxillary canine. The maxillary central and lateral incisors showed marked displacement (Fig. 2C).
The patient was referred to The Wanless Hospital, Miraj. The ultrasound examination showed a high-flow arteriovenous malformation. Admission laboratory tests showed hemoglobin (Hb) of 7.3 g/dL, a platelet count of 63,000 per mm3, prothrombin time of 17 seconds, activated partial thromboplastin time of 35 sec, and international normalized ratio of 1.3. The patient was then given blood and platelet transfusions after which the blood investigations showed hemoglobin of 13.3 g/dL, platelet count of 1,96,000, prothrombin time 15 seconds, activated partial thromboplastin time of 28 seconds and international normalized ratio of 1.1. Diagnostic angiography was performed after gaining access from the right femoral artery. Selective catheterization of the right external carotid artery was performed under fluoroscopic guidance. The diagnostic angiogram showed a high-flow vascular malformation supplied principally by the alveolar branch of the internal maxillary artery. Surgical treatment of such lesion required extensive resection of the maxilla and might result in the dysfunction and disfigurement. Ligation of the external carotid artery was not advisable, since many anastomoses promoted the rapid appearance of a collateral circulation. Therefore, embolization which consisted of occlusion of the vessels which contributed to the lesion was considered. Further selective catheterization of the maxillary artery was performed. Embolization was performed using polyvinyl alcohol (PVA) particles (Fig. 3). The patient tolerated the procedure well and had an unremarkable postoperative course. One week postoperatively the patient showed complete regression of the palatal lesion (Fig. 4). One year follow-up revealed a significant reduction of clinical symptoms and signs of the lesion without any further complications.
AVMs are extremely rare conditions that can be fatal if left untreated.6 They are caused by disturbances in the late stages of angiogenesis, mainly abnormal differentiation of vascular system.10 Vascular malformations can be subdivided further into high-flow and low-flow lesions.1,2 In the present case, angiography was performed which demonstrated a high-flow AVM.
The diagnosis of AVMs can be made clinically in conjunction with imaging studies. Most AVMs have a history that includes the presence of a vascular blush in the overlying skin in the childhood, which begins to expand more rapidly as the patient enters puberty or undergoes other hormonal changes. They may also reveal a history of trauma to the involved area prior to the notification of the lesion. Bleeding, pain, and tissue destruction are often subsequent signs in AVM.1,6 On physical examination, early AVMs may have an overlying vascular blush in the skin similar to an early port-wine stain. The mucosa is usually thickened and vascular, and pulsation is usually present. The teeth may be loose or may exhibit pumping movement when pressure is applied and released.1,3,4,6 AVMs can invade the skin where ulcerations and bleeding are common.1,11 Some "high-flow" lesions may result in consumption coagulopathy, requiring transfusion therapy.12,13
Multiple imaging modalities should be used to evaluate characteristics of AVMs such as size, flow velocity, flow direction, relation to the surrounding structures and lesion contents.2 There are no pathognomonic radiographic features to distinguish AVMs on plain radiographs. They may appear as bone erosion, sclerotic change, periosteal reaction or a cyst like radiolucent lesion. A sunburst effect, created by spicules radiating from the center, is often present.2,14 The lesions most often have a multiloculated appearance due to residual bone trapped around vessels. Small radiolucent locules may resemble enlarged marrow spaces surrounded by coarse, dense, and well defined trabeculae. They may have a honey comb or soap-bubble pattern that is well demarcated from adjacent bone. The roots of the teeth in proximity of the lesion may show displacement or resorption. High-flow lesions tend to result in more destructive skeletal changes, appearing as moth-eaten and poorly defined areas of radiolucency.12 The radiographic differential diagnosis of these lesions include ameloblastoma, ameloblastic fiboma, odontogenic myxoma, central giant cell granuloma and metastatic malignant tumors.6
Color Doppler ultrasound examination can provide information about the flow velocity. Contrast enhanced CT can be useful in assessing the AVMs. The drawbacks of CT are considerable exposure to ionizing radiation and limited information about blood flow.2 Angiography and MR imaging are the preferred imaging modalities.2,6,10,15 MRI depicts the anatomic relation of the vascular lesion with adjacent organs and the flow velocity of lesions. It is useful for evaluating the lesions postoperatively.2 Angiography is currently the gold standard for the determination of location and flow characteristics of vascular lesions. Angiography is useful to determine blood vessels supplying blood to the lesion, and the relative venous out-flow characteristics, and the presence or absence of arteriovenous shunts.3 According to Orbach, the angiographic features of AVMs include dilatation and lengthening of afferent arteries, early and preferential filling of shunts, delayed filling of associated normal arteries, early opacification of draining veins and rapid flow to collateral vessels.16
Intentional transarterial embolization was originally described in 1969 by Lalli and coworkers.17 Treatment of vascular malformation with selective embolization procedure is currently highly recommended and often used. The purpose of the selective embolization is to abruptly cut off the blood supply of the lesion, reducing the risk of potentially massive and lethal blood loss after its rupture, enabling a more focused and selective surgical procedure with less morbidity and with maximal preservation of important structures.18 Various materials can be used for embolization. They can be classified as either temporary or permanent. Temporary materials include autologous clot or muscle, Gelfoam19,20 and microfibrillar collagen. Permanent agents include silicone spheres, lyophilized dura, PVA, isobutyl cyanoacrylate and stainless steel or platinum coils. The most commonly used materials are Gelfoam and PVA. PVA was used in present case as it is nonabsorbable and denser than Gelfoam.9
To conclude, vascular malformations represent some of the most difficult lesions to diagnose and treat. Interventional radiography plays an essential role in diagnosis and management of such lesions. With the use of this technique, extensive surgical procedures can be avoided so as to avoid facial disfigurement and functional compromise.
Figures and Tables
Fig. 1
A. Extraoral photograph shows port-wine stain and extraoral swelling. B. Intraoral photograph shows the extent of the lesion from buccal aspect. C. Intraoral photograph shows the palatal extent of lesion.

Fig. 2
Intraoral periapical radiographs show coarse bony trabeculae and enlarged marrow spaces. A. Right maxillary posterior portion. B. Right maxillary anterior portion. C: Panoramic radiograph shows an ill-defined irregular area of bone destruction in right maxillary anterior region.
Acknowledgements
The authors are thankful to Dr. Rahul Kumar for his great help during preparation of manuscript. The authors would like to thank Dr. Avinash Kshar, Dr. Nivedita Bajantri, Dr, Alka Hazari, Dr. Praveen Kumar, Dr. Amit Mathur and Dr. Arati Oka for their co-operation.
References
1. Buckmiller LM, Richter GT, Suen JY. Diagnosis and management of hemangiomas and vascular malformations of the head and neck. Oral Dis. 2010. 16:405–418.

2. Hyodoh H, Hori M, Akiba H, Tamakawa M, Hyodoh K, Hareyama M. Peripheral vascular malformations: imaging, treatment approaches, and therapeutic issues. Radiographics. 2005. 25:Suppl 1. S159–S171.

3. Nekooei S, Hosseini M, Nazemi S, Talaei-Khoei M. Embolisation of arteriovenous malformation of the maxilla. Dentomaxillofac Radiol. 2006. 35:451–455.

4. Lei ZM, Huang XX, Sun ZJ, Zhang WF, Zhao YF. Surgery of lymphatic malformations in oral and cervicofacial regions in children. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007. 104:338–344.

5. Bai Y, Jia J, Huang XX, Alsharif MJ, Zhao JH, Zhao YF. Sclerotherapy of microcystic lymphatic malformations in oral and facial regions. J Oral Maxillofac Surg. 2009. 67:251–256.

6. Mohammadi H, Said-Al-Naief NA, Heffez LB. Arteriovenous malformation of the mandible: report of a case with a note on the differential diagnosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997. 84:286–289.
7. Larsen PE, Peterson LJ. A systematic approach to management of high-flow vascular malformations of the mandible. J Oral Maxillofac Surg. 1993. 51:62–69.

8. Noreau N, Landry P, Morais D. Arteriovenous malformation of the mandible: review of literature and case history. J Can Dent Assoc. 2001. 67:646–651.
9. Caiazzo A, Mehra P, Papageorge MB. The use of preoperative percutaneous transcatheter vascular occlusive therapy in the management of Sturge-Weber syndrome: report of a case. J Oral Maxillofac Surg. 1998. 56:775–778.

10. Lai QG, Li GJ, Yuan KF, Xu X, Wang YZ, Li YL, et al. Transarterial embolization of a high-flow maxillary arteriovenous malformation fed by multiple arteries. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009. 108:e17–e21.

11. Donnelly LF, Adams DM, Bisset GS 3rd. Vascular malformations and hemangiomas: a practical approach in a multidisciplinary clinic. AJR Am J Roentgenol. 2000. 174:597–608.
12. Kademani D, Costello BJ, Ditty D, Quinn P. An alternative approach to maxillofacial arteriovenous malformations with transosseous direct puncture embolization. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004. 97:701–706.

13. Speer AL, Panossian A, Arkader A, Stanley P, Anselmo DM. Vascular surgery for arteriovenous malformations. eMedicine from WebMD. Updated Aug 9, 2010. Available at http://emedicine.medscape.com/article/459927-diagnosis.
14. Johnson LM, Cook H, Friedlander A. Central arteriovenous malformations of the maxillofacial skeleton: case report. J Oral Maxillofac Surg. 1991. 49:759–763.

15. Woods NK, Goaz PW. Differential diagnosis of oral lesions. 1991. 4th ed. St. Louis: CV Mosby Co;285.
16. Orbach S. Congenital arteriovenous malformations of the face. Report of a case. Oral Surg Oral Med Oral Pathol. 1976. 42:2–13.
17. Lalli AF, Peterson N, Bookstein JJ. Roentgen-guided infarctions of kidneys and lungs. A potential therapeutic technic. Radiology. 1969. 93:434–435.
18. Nagler RM, Braun J, Daitzchman M, Peled M, Laufer D. Selective embolization for head and neck vasculopathies. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002. 93:127–131.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download