INTRODUCTION
Holmium laser enucleation of the prostate (HoLEP) makes it possible to remove an entire enlarged adenoma confidently in the natural-tissue plane of the surgical capsule. A recent study reported that HoLEP is a safe and effective treatment for benign prostatic hyperplasia (BPH) among the elderly [
1]. Compared with younger patients, patients aged ≥80 years had similar overall morbidity and 6-month functional outcomes after HoLEP [
1]. Thus, HoLEP is considered a safe and effective treatment modality for bladder outlet obstruction (BOO) related to BPH, and has been reported to have lower morbidity rates than other modalities [
2]. Comparisons with conventional treatment modalities have shown that HoLEP has excellent hemostatic properties and causes less electrolyte deterioration [
345]. Furthermore, in view of its effectiveness, it has been suggested that HoLEP offers a possible alternative to open prostatectomy [
67].
Since the first clinical report on HoLEP was published by Gilling et al [
8] in 1996, several randomized controlled trials have been conducted. HoLEP produces clinical outcomes that are similar to those of transurethral resection of the prostate (TURP) and open prostatectomy, but has lower postoperative complication rates and shorter hospital stays [
5691011]. In addition, HoLEP appears to be a true endourological alternative to open prostatectomy, because it can treat very large prostates more effectively [
1213].
Although the technique has been refined and its popularity has increased, HoLEP faces major impediments to its widespread application. In particular, the endoscopic technique is challenging and appears to be difficult to learn, meaning that HoLEP has a steep learning curve. Furthermore, these difficulties have delayed its adoption by the urological community [
14].
Several reports have investigated the learning curve of HoLEP [
361415]. Some authors have argued that a surgeon needs experience with between 20 and 30 cases to attain competency [
36], while others have argued that up to 50 cases are needed [
1415]. These discrepancies are mainly caused by the absence of an accurate means of evaluating the operative learning curve, that is, the lack of a proper parameter for estimating the operator's enucleation skills.
To date, researchers have attempted to identify parameters that can be used to determine how many cases are needed to attain competency. However, the most important consideration is which parameter is more sensitive for the evaluation of enucleation skills. Enucleation efficacy [
141516] and enucleation ratio (ER) efficacy (ERE) [
17] have been used to plot the learning curve, but both focus on time and do not consider energy, although operators simultaneously consume both time and energy during HoLEP.
Therefore, the present study was undertaken to develop a new parameter suitable for estimating the operator's enucleation skills that includes a consideration of energy consumption.
Go to :

MATERIALS AND METHODS
1. Ethics statement
The present study protocol was reviewed and approved by the Institutional Review Board of Gachon University Gil Medical Center, Incheon, Republic of Korea (approval number: GAIRB2015-85). Informed consent was submitted by all subjects when they were enrolled.
2. Subject
One hundred consecutive patients who underwent HoLEP for BPH from April 2012 to April 2014 were enrolled. All patients were treated by a single surgeon. Perioperatively, the enucleation time and consumed energy were recorded and the enucleated weight was measured. The perioperative clinical variables, including ER (=enucleated weight/transitional zone volume [TZV]), ERE (=ER/enucleation time), enucleation time-efficacy (ETE=enucleated weight/enucleation time), enucleation energy-efficacy (EEE=enucleated weight/consumed energy), and enucleation time-energy-efficacy (ETEE=enucleated weight/enucleation time/consumed energy) were analyzed.
An 80-W OmniPulse MAX® (Trimedyne Inc., Irvine, CA, USA) was used for HoLEP, which was performed as described by Gilling et al [
18]. With the patient placed in the lithotomy position under spinal anesthesia (spinal anesthesia was usually preferred), the urethra was dilated with a 30-Fr metal catheter, and a working sheath was introduced. The energy source consisted of an 80-W holmium: yttrium aluminium garnet laser with a 550-µm end-firing laser fiber (FlexMAX®; Trimedyne Inc.). A 26-Fr resectoscope (Karl Storz™) with a laser bridge was used, and normal saline irrigation was performed continuously. The enucleated prostatic tissue was removed by transurethral morcellation using a mechanical morcellator (Richard Wolf, Knittlingen, Germany) that was introduced through an offset rigid nephroscope. The bladder was maintained in a distended condition during morcellation. Lubricants were applied to the scope intermittently throughout the procedure. At the end of surgery, a 22-Fr 3-way urethral Foley catheter was placed
in situ for continuous postoperative irrigation. In general, the flow of irrigation fluid was reduced gradually and cut off the morning after surgery. The urethral catheter was removed after confirming the cessation of hematuria.
3. Statistical analysis
Basic data were expressed using descriptive statistics. Groups of 10 consecutive cases were used to analyze enucleation efficiency. Statistical analyses were performed by one-way analysis of variance (ANOVA) with the post hoc Tukey test. To estimate the sensitiveness of the different parameters for assessing enucleation efficiency, we calculated the coefficient of variation (CV=standard deviation [SD]/mean×100 [%]), which provides a standardized measure of a probability or frequency distribution. Analyses were performed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA), and differences were considered statistically significant when p-values were less than 0.05.
Go to :

RESULTS
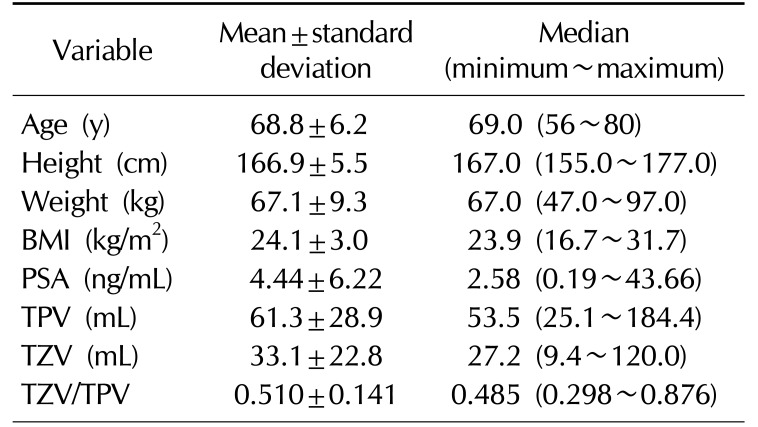
The mean patient age and preoperative prostate specific antigen level were 68.8±6.2 years and 4.44±6.22 ng/mL, respectively (
Table 1). The mean total prostate volume and TZV were 61.3±28.9 mL and 33.1±22.8 mL, respectively (
Table 1).
Table 1
Characteristics of the study population (n=100)
|
Variable |
Mean±standard deviation |
Median (minimum~maximum) |
|
Age (y) |
68.8±6.2 |
69.0 (56~80) |
|
Height (cm) |
166.9±5.5 |
167.0 (155.0~177.0) |
|
Weight (kg) |
67.1±9.3 |
67.0 (47.0~97.0) |
|
BMI (kg/m2) |
24.1±3.0 |
23.9 (16.7~31.7) |
|
PSA (ng/mL) |
4.44±6.22 |
2.58 (0.19~43.66) |
|
TPV (mL) |
61.3±28.9 |
53.5 (25.1~184.4) |
|
TZV (mL) |
33.1±22.8 |
27.2 (9.4~120.0) |
|
TZV/TPV |
0.510±0.141 |
0.485 (0.298~0.876) |

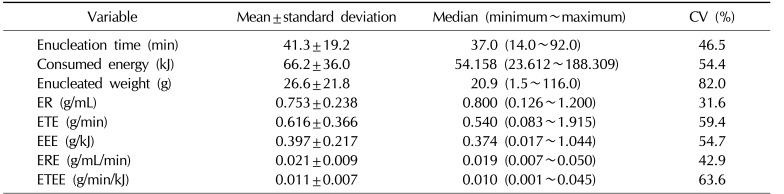
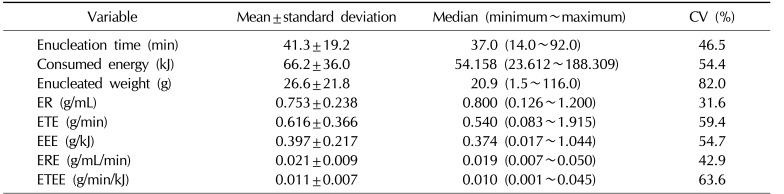
The mean enucleation time and consumed energy were 41.3±19.2 minutes and 66.2±36.0 kJ, respectively (
Table 2). The mean enucleated weight and ER were 26.6±21.8 g and 0.753±0.238 g/mL, respectively (
Table 2). The mean ETE and EEE were 0.616±0.366 g/min and 0.397±0.217 g/kJ, respectively (
Table 2). The mean ERE and ETEE were 0.021±0.009 g/mL/min and 0.011±0.007 g/min/kJ, respectively (
Table 2).
Table 2
Enucleation-associated variables
|
Variable |
Mean±standard deviation |
Median (minimum~maximum) |
CV (%) |
|
Enucleation time (min) |
41.3±19.2 |
37.0 (14.0~92.0) |
46.5 |
|
Consumed energy (kJ) |
66.2±36.0 |
54.158 (23.612~188.309) |
54.4 |
|
Enucleated weight (g) |
26.6±21.8 |
20.9 (1.5~116.0) |
82.0 |
|
ER (g/mL) |
0.753±0.238 |
0.800 (0.126~1.200) |
31.6 |
|
ETE (g/min) |
0.616±0.366 |
0.540 (0.083~1.915) |
59.4 |
|
EEE (g/kJ) |
0.397±0.217 |
0.374 (0.017~1.044) |
54.7 |
|
ERE (g/mL/min) |
0.021±0.009 |
0.019 (0.007~0.050) |
42.9 |
|
ETEE (g/min/kJ) |
0.011±0.007 |
0.010 (0.001~0.045) |
63.6 |

The CVs of enucleated weight and ER were 82.0% and 31.6%, respectively (
Table 2), and the CVs of ETE and EEE were 59.4% and 54.7%, respectively (
Table 2). The CVs of ERE and ETEE were 42.9% and 63.6%, respectively (
Table 2).
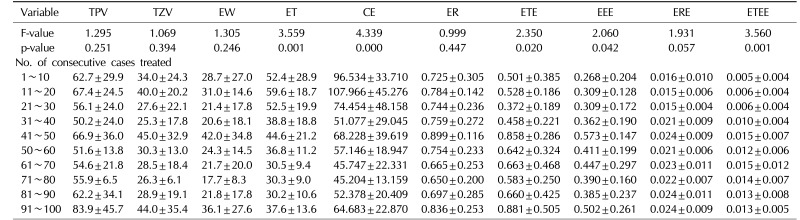
In the present study, the 100 patients were divided into 10 groups of 10 consecutive cases. The groups were named as follows: cases 1~10 as groups 1, cases 11~20 as group 2, cases 21~30 as group 3, cases 31~40 as group 4, cases 41~50 as group 5, cases 51~60 as group 6, cases 61~70 as group 7, cases 71~80 as group 8, cases 81~90 as group 9, and cases 91~100 as group 10.
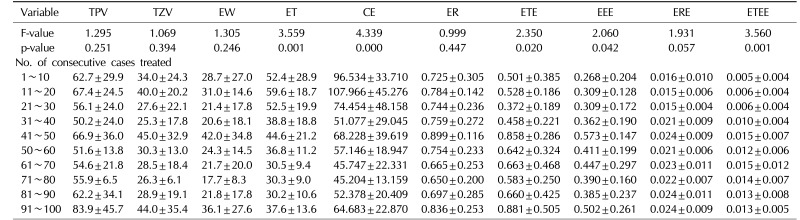
Table 3 summarizes the changes in operative parameters for these 10 groups of 10 consecutive cases. ANOVA showed that the group mean values of ETE (F=2.350, p=0.020), EEE (F=2.060, p=0.042), and ETEE (F=3.560, p=0.001) were significantly different, but that those of ER (F=0.999, p=0.447) and ERE (F=1.931, p=0.057) were not (
Table 3).
Table 3
Learning curve-related operative parameters according to the number of consecutive cases treated (analysis of variance)
|
Variable |
TPV |
TZV |
EW |
ET |
CE |
ER |
ETE |
EEE |
ERE |
ETEE |
|
F-value |
1.295 |
1.069 |
1.305 |
3.559 |
4.339 |
0.999 |
2.350 |
2.060 |
1.931 |
3.560 |
|
p-value |
0.251 |
0.394 |
0.246 |
0.001 |
0.000 |
0.447 |
0.020 |
0.042 |
0.057 |
0.001 |
|
No. of consecutive cases treated |
|
1~10 |
62.7±29.9 |
34.0±24.3 |
28.7±27.0 |
52.4±28.9 |
96.534±33.710 |
0.725±0.305 |
0.501±0.385 |
0.268±0.204 |
0.016±0.010 |
0.005±0.004 |
|
11~20 |
67.4±24.5 |
40.0±20.2 |
31.0±14.6 |
59.6±18.7 |
107.966±45.276 |
0.784±0.142 |
0.528±0.186 |
0.309±0.128 |
0.015±0.006 |
0.006±0.004 |
|
21~30 |
56.1±24.0 |
27.6±22.1 |
21.4±17.8 |
52.5±19.9 |
74.454±48.158 |
0.744±0.236 |
0.372±0.189 |
0.309±0.172 |
0.015±0.004 |
0.006±0.004 |
|
31~40 |
50.2±24.0 |
25.3±17.8 |
20.6±18.1 |
38.8±18.8 |
51.077±29.045 |
0.759±0.272 |
0.458±0.221 |
0.362±0.190 |
0.021±0.009 |
0.010±0.004 |
|
41~50 |
66.9±36.0 |
45.0±32.9 |
42.0±34.8 |
44.6±21.2 |
68.228±39.619 |
0.899±0.116 |
0.858±0.286 |
0.573±0.147 |
0.024±0.009 |
0.015±0.007 |
|
50~60 |
51.6±13.8 |
30.3±13.0 |
24.3±14.5 |
36.8±11.2 |
57.146±18.947 |
0.754±0.233 |
0.642±0.324 |
0.411±0.199 |
0.021±0.006 |
0.012±0.006 |
|
61~70 |
54.6±21.8 |
28.5±18.4 |
21.7±20.0 |
30.5±9.4 |
45.747±22.331 |
0.665±0.253 |
0.663±0.468 |
0.447±0.297 |
0.023±0.011 |
0.015±0.012 |
|
71~80 |
55.9±6.5 |
26.3±6.1 |
17.7±8.3 |
30.3±9.0 |
45.204±13.159 |
0.650±0.200 |
0.583±0.250 |
0.390±0.160 |
0.022±0.007 |
0.014±0.007 |
|
81~90 |
62.2±34.1 |
28.9±19.1 |
21.8±17.8 |
30.2±10.6 |
52.378±20.409 |
0.697±0.285 |
0.660±0.425 |
0.385±0.237 |
0.024±0.011 |
0.013±0.008 |
|
91~100 |
83.9±45.7 |
44.0±35.4 |
36.1±27.6 |
37.6±13.6 |
64.683±22.870 |
0.836±0.253 |
0.881±0.505 |
0.502±0.261 |
0.024±0.009 |
0.013±0.005 |

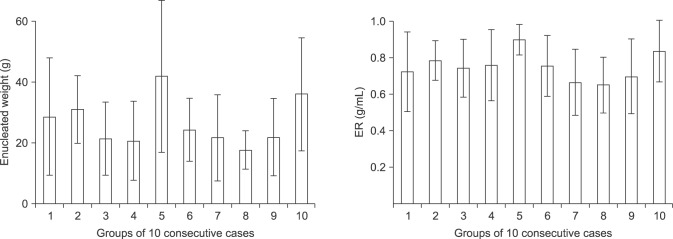
ER had a smaller SD than enucleated weight because ER was designed to reduce the distribution spread caused by different enucleated weights. In particular, in cases 41~50 (group 5), the SD of ER was much smaller than that of enucleated weight (
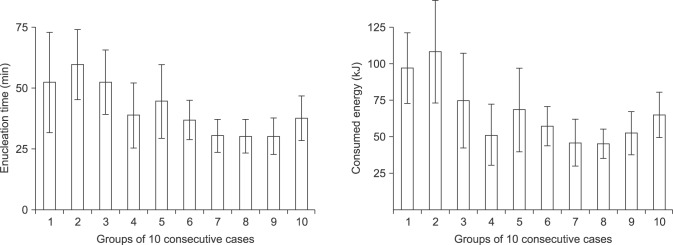
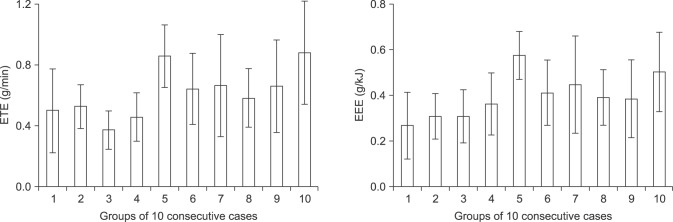
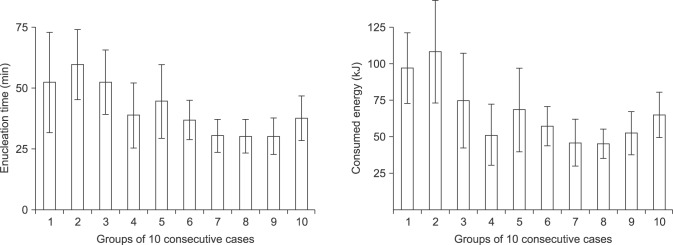
Fig. 1). Gradual decreases in both enucleation time and consumed energy were observed with increasing case numbers. Like enucleation time, consumed energy also tended to decrease after 20 cases (group 2) and plateaued at 61~70 cases (group 7) (
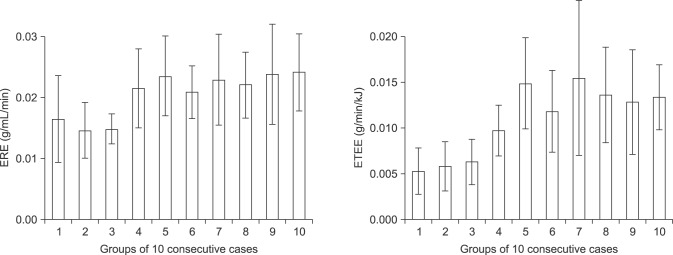
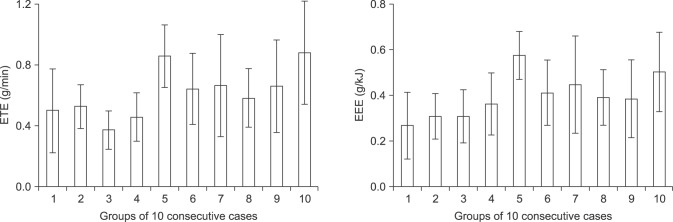
Fig. 2). Gradual improvements were observed in both ETE and EEE. Like ETE, EEE also tended to increase (
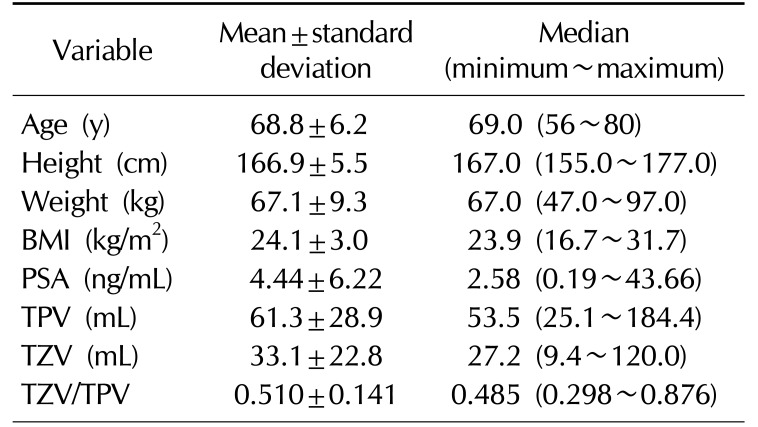
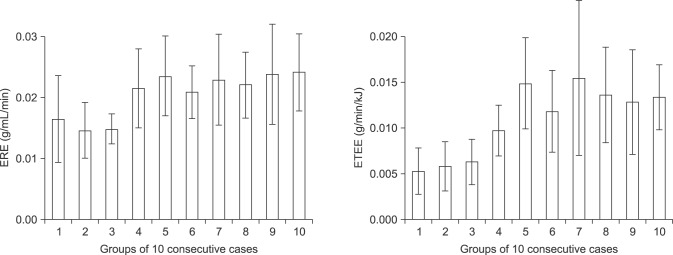
Fig. 3). The curve of ERE plateaued after 30 cases (group 3), but that of ETEE increased after 30 cases (group 3) and plateaued at 61~70 cases (group 7), which indicates that the operator's enucleation skills continued to increase even after 30 cases (group 3) (
Fig. 4).
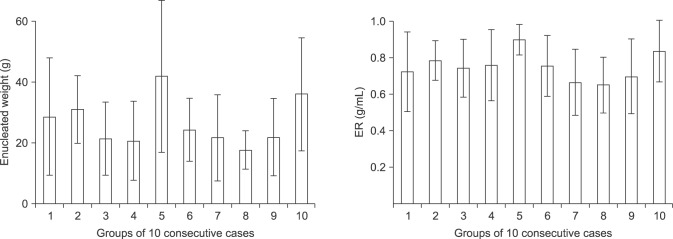 | Fig. 1Enucleated weight and enucleation ratio (ER). ER had a lower standard deviation (SD) than enucleated weight, because ER was designed to reduce the variance shown by enucleated weight. In particular, in cases 41~50 (group 5), the SD of ER was much smaller than that of enucleated weight. The 100 patients were divided into 10 groups of 10 consecutive cases, as follows: cases 1~10 as groups 1, cases 11~20 as group 2, cases 21~30 as group 3, cases 31~40 as group 4, cases 41~50 as group 5, cases 51~60 as group 6, cases 61~70 as group 7, cases 71~80 as group 8, cases 81~90 as group 9, and cases 91~100 as group 10.
|
 | Fig. 2Enucleation time and consumed energy. Gradual decreases in both enucleation time and consumed energy were observed. Like enucleation time, consumed energy also showed a decreasing trend even after 20 cases (group 2) and plateaued at 61~70 cases (group 7).
|
 | Fig. 3Enucleation time-efficacy (ETE) and enucleation energy-efficacy (EEE). Gradual improvements in ETE and EEE were observed. Like ETE, EEE also tended to increase.
|
 | Fig. 4Enucleation ratio efficacy (ERE) and enucleation time-energy-efficacy (ETEE). ERE plateaued after 30 cases (group 3). However, ETEE continued to increase even after 30 cases (group 3) and plateaued at 61~70 cases (group 7). This means that even after 30 cases (group 3), the operator's enucleation skills continued to increase.
|
Go to :

DISCUSSION
BPH is very common in elderly men. In the Baltimore Longitudinal Study of Aging, almost 60% of 60-year-olds had some degree of clinical BPH [
19]. TURP has been considered the gold standard surgical treatment for BPH [
20]. Recently, surgical techniques using lasers, such as photoselective vaporization of the prostate, HoLEP and thulium laser enucleation of the prostate have been increasingly adopted, with a number of reports documenting their merits.
Laser prostatectomy has continuously evolved since Gilling et al [
21] first described HoLEP in 1995. In 1998, the concept of morcellation was adopted and the technique was applied to patients with BOO [
18]. However, the steep operative learning curve of HoLEP has hindered its widespread use, despite its advantages.
Researchers have tried to identify parameters that show how many cases of experience are needed to attain competency. However, the sensitivity of a parameter with respect to the evaluation of enucleation skills is probably more important. To date, enucleation efficacy [
141516] and ERE [
17] have been used as parameters for the HoLEP learning curve, but they focus on time alone, although operators simultaneously consume time and energy during HoLEP.
The present study is the first to confirm that like enucleation time, energy consumption also decreases as the enucleation technique of a single surgeon develops (
Fig. 2). In the present study, we sought to identify a parameter that considers both time and energy. Our results demonstrate that even after 30 cases (group 3), enucleation skills continued to improve (
Fig. 4). In addition, we found that ETEE provided a more sensitive means of evaluating enucleation skills than ERE. In other words, rather than simply assessing the efficiency of the enucleation technique in terms of enucleation time, as in previous studies about the HoLEP learning curve, it is better to assess the efficiency of the enucleation technique with ETEE, which is a parameter that combines time and energy usage (
Fig. 4).
The CV provides a standardized measure of the dispersion of a probability distribution or frequency distribution, and is calculated by dividing the SD by the mean. The CV is useful because the SD of data must be understood in the context of the mean value. For comparisons between data sets with different units or widely different means, one should use the CV instead of the SD.
In the present study, we used the CV as the scale to assess the sensitivity of each parameter for enucleation efficiency. In fact, ER was designed to reduce the variance caused by enucleated weight [
17], and thus, ER had a lower CV than enucleated weight (31.6%
vs. 82.0%) (
Table 2,
Fig. 1). Similarly, ERE (42.9%), which is derived from ER, had a lower CV than ETE (59.4%), EEE (54.7%), and ETEE (63.6%) (
Table 2), which means that ETEE had a much wider distribution than ERE, and thus, ETEE was more sensitive than ERE for evaluating enucleation skills.
In the present study, ANOVA showed that mean ETEE values changed significantly with time; that is, they were significantly different across the 10 groups of 10 consecutive cases (p=0.001), whereas no significant changes were found for ERE (p=0.057) (
Table 3). This means that ETEE is more suitable than ERE for showing improvements in enucleation skills.
ER is defined as the ratio of the enucleated weight to the TZV. Thus, ER seems to be a fixed constant value, and it did not increase as enucleation skills improved. ER could increase depending on the improvement of device (morcellator) performance, allowing it to retrieve the enucleated prostate tissue without loss. Therefore, we think that ERE, which is derived from ER, does not provide a sensitive evaluation of the surgeon's enucleation skills, as ER is designed to reduce the variance of enucleated weight [
17].
In the present study, ERE plateaued after 30 cases (group 3), which is similar to the study by Jeong et al [
17]. However, ETEE continued to increase even after 30 cases (group 3) and plateaued at 61~70 cases (group 7) (
Fig. 4). This indicates that for cases 31~40 (group 4), the plateau of ERE did not indicate a real attainment of competency in enucleation skills. Therefore, we think that ETEE, which considers enucleation time and consumed energy simultaneously, is more sensitive for evaluating enucleation skills than previous parameters (including ETE and ERE) that only consider enucleation time.
The present study has several limitations. First, it is intrinsically limited by its retrospective design, despite the enrollment of consecutive patients to avoid potential selection bias. Second, the study was conducted on patients operated on by a single surgeon. Accordingly, we suggest that ETEE should be evaluated in group of several surgeons in the future, to determine if it is generally acceptable. Third, we did not investigate whether energy usage varied according to patients' bleeding tendency and vascular distribution except for prostate size, although the amount of laser energy used may vary depending on those factors, as well as prostate volume and TZV. Although no accurate information was available regarding patients' bleeding tendency, in the early stages of HoLEP surgery, surgeons generally perform surgery on patients who are not likely to bleed because of their deficient surgical technique. As the surgeon's technique gradually develops, patients with bleeding tendencies can be operated on. However, as shown in
Fig. 2 of this study, energy consumption decreased as the technique developed. This means that less energy is used as the surgeon's enucleation skill develops. Therefore, we think that this clearly shows that in the HoLEP learning curve, the development of the enucleation technique can be evaluated not only by time, but also by energy usage (
Fig. 3) and that ETEE is more sensitive for evaluating the enucleation skills than previous parameters (including ETE and ERE) (
Fig. 4). Furthermore, in clinical settings after the surgeon's enucleation skill has fully developed, we believe that ETEE can quantitatively measure the difficulty of enucleation due to the patient's bleeding tendency and vascular distribution.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download