This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
De novo erectile dysfunction (ED) is a known complication after urethroplasty. Incidence and natural history of de novo ED after urethroplasty is underreported. We assessed the incidence of de novo ED after urethroplasty.
Materials and Methods
Consecutive consenting urethroplasty (n=48) patients aged 21 to 50 years from February 2014 to July 2016 with normal preoperative erectile function as determined by an International Index of Erectile Function-5 (IIEF-5) score ≥22 were included and interviewed at 3, 6, and 12 months.
Results
In patients with anterior stricture (n=40), substitution urethroplasty (SU) was performed in 22 patients (55.0%) and end-to-end anastomotic urethroplasty (EEAU) in 18 patients (45.0%). Their mean IIEF-5 score was 24.15±0.8 preoperatively, 20.10±4.2 at 3 months (p<0.001), 22.70±2.3 at 6 months (p=0.0012), and 23.70±1.7 at 12 months (p=0.03), showing a recovery of erectile function with time. All 8 patients with pelvic fracture urethral injury (PFUI) underwent progressive perineal urethroplasty. Their mean IIEF score was 24.0±1.2 preoperatively, 18.8±5.4 at 3 months (p=0.002), 20.9±3.5 at 6 months (p=0.37), and 22.0±1.5 at 12 months (p=0.427). The incidence of ED was similar at 1 year postoperatively between patients with anterior stricture and PFUI and between patients who underwent EEAU or SU for anterior stricture.
Conclusions
Incidence of ED at 1 year after PFUI is similar to that after surgery for anterior stricture in patients with normal preoperative erectile function. Among the cases of anterior stricture, recovery was better with SU at 3 months and was similar between SU and EEAU at 1 year.
Go to :

Keywords: Erectile dysfunction, Urethral stricture
INTRODUCTION
Urethral stricture disease (USD) affects the quality of life of the patient and his partner. Urethral reconstructive surgery provides good long-term results in most patients. Endoscopic management is minimally invasive, but is associated with a higher chance of recurrence. The cost-effectiveness of definitive repair makes urethral reconstruction a more attractive option for USD [
1]. Urethroplasty is hence the gold standard for the treatment of USD [
2]. It involves dissection near the neurovascular structures responsible for normal erectile function [
3].
De novo erectile dysfunction (ED) is a known complication after urethroplasty. The outcomes of urethral reconstructive surgery have traditionally focused on parameters such as urinary flow rate, lower urinary tract symptom (LUTS) score, or recurrent USD requiring further treatment. Mundy [
4] was the first urologist to report the incidence of ED after urethroplasty in 1993. The incidence of
de novo ED after urethroplasty is largely underreported. We assessed the incidence and clinical course of
de novo ED after urethroplasty at Institute of Nephro Urology.
Go to :

MATERIALS AND METHODS
This was a hospital-based, prospective, observational study carried out among patients undergoing urethroplasty at the Department of Urology of a tertiary care referral-based urology center in south India. After obtaining approval from the Institute Research Council and Ethics Committee, the study was conducted from February 2014 to July 2016.
1. Study population
Consecutive consenting patients undergoing urethroplasty, aged 21 to 50 years, belonging to the American Society of Anesthesiologists class I and II, and with normal preoperative erectile function as assessed by International Index of Erectile Function (IIEF-5) were eligible for the study after providing written informed consent [
5]. The exclusion criteria were inability to understand the IIEF-5 score, diabetes mellitus, ischemic heart disease, preexisting ED, prior endoscopic internal urethrotomy, substitution urethroplasty (SU) using a technique other than a dorsal-onlay buccal mucosal graft, not engaging in sexual intercourse before or after surgery, recurrent USD, and patients with complications in the postoperative period such as a surgical site infection, failure to void at the end of 3 weeks after per urethral catheter (PUC) removal, or the development of recurrent LUTS or urinary tract infections within the first 3 months after a successful urethroplasty.
2. Brief procedure and surgical technique
Consecutive consenting patients conforming to the inclusion criteria were administered the IIEF-5 questionnaire, and those with a preoperative IIEF-5 score ≥22 (no ED) were included in the study. The operative technique was selected based on the length and location of the stricture, as well as the age and general health of the patient. Patients with inflammatory strictures in the bulbar urethra underwent end-to-end anastomotic urethroplasty (EEAU) for dense short-segment strictures (<1.5 cm). Longer-segment bulbar and penile urethral strictures underwent dorsal-onlay buccal mucosal graft SU. Patients with pelvic fracture urethral injury (PFUI) underwent a progressive perineal urethroplasty (PPU). All urethroplasties were performed with a 16-Fr silicone PUC in place. The PUC was removed after performing a pericatheter urethrogram at 3 weeks from the date of surgery. Successful urethroplasty was defined as the patient being able to void with a good urinary stream (Qmax >15 mL/s on uroflowmetry). Patients were advised to engage in sexual activity starting 2 weeks after PUC removal. Patients who developed a surgical site infection within the first month after surgery, failure to void at the end of 3 weeks after PUC removal, or recurrent LUTS or urinary tract infections within the first 3 months after a successful urethroplasty were excluded. The IIEF questionnaire was administered again postoperatively at 3, 6, and 12 months. Patients with an IIEF-5 score of 17 to 21 were considered to have mild ED, while a score of 12 to 16 constituted mild to moderate ED, a score of 8 to 11 constituted moderate ED, and a score of <7 constituted severe ED [
6].
3. Statistical analysis
Statistical analysis was performed using IBM SPSS ver. 20 for Windows (IBM Co., Armonk, NY, USA). The normality of the data was assessed using a stem-and-leaf plot. The variables were summarized using mean values with standard deviation, median, interquartile range, or percentages based on the characteristics of the variables. Repeated-measures analysis of variance was done to assess the changes from the preoperative IIEF-5 scores to those at 3, 6, and 12 months, postoperatively. The chi-square test was used to compare the proportions of various categories of ED based on IIEF-5 scores at different time intervals. p-values <0.05 were considered to indicate statistical significance.
Go to :

RESULTS
From February 2014 to January 2015, total of 102 men underwent urethroplasty at our institution, and follow-up was completed in July 2016. A total of 48 patients were eligible for the final analysis.
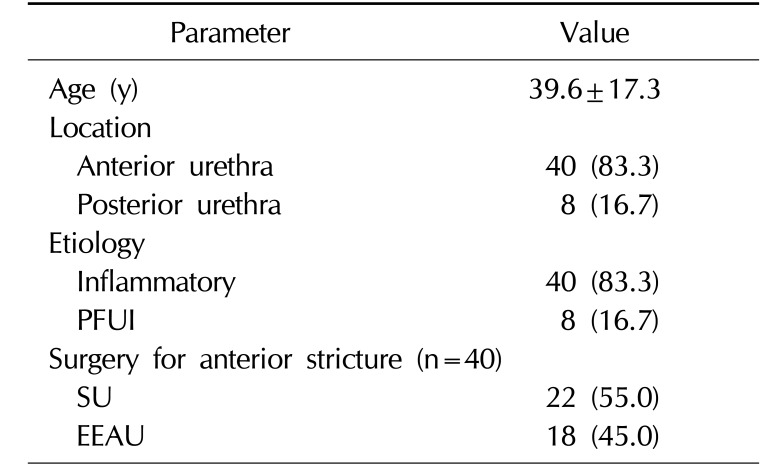
1. Baseline and operative characteristics
The baseline characteristics, stricture location, and surgery type are summarized in
Table 1. We had 8 patients with hypertension in our study population. None of them received beta blockers or diuretics; instead, they received calcium-channel blockers, angiotensin-converting enzyme inhibitors, or angiotensin receptor blockers. Among patients with anterior USD, SU was performed in 22 patients (55.0%) and EEAU in 18 patients (45.0%), while all 8 patients with PFUI underwent PPU. Only 1 patient had a short-segment penile urethral stricture, and he underwent SU. We did not perform EEAU for short-segment penile urethral strictures.
Table 1
Demographic and operative characteristics
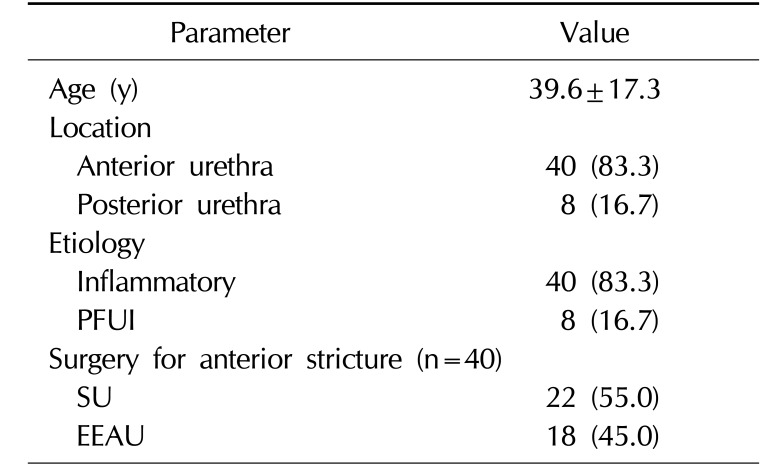
|
Parameter |
Value |
|
Age (y) |
39.6±17.3 |
|
Location |
|
|
Anterior urethra |
40 (83.3) |
|
Posterior urethra |
8 (16.7) |
|
Etiology |
|
|
Inflammatory |
40 (83.3) |
|
PFUI |
8 (16.7) |
|
Surgery for anterior stricture (n=40) |
|
|
SU |
22 (55.0) |
|
EEAU |
18 (45.0) |

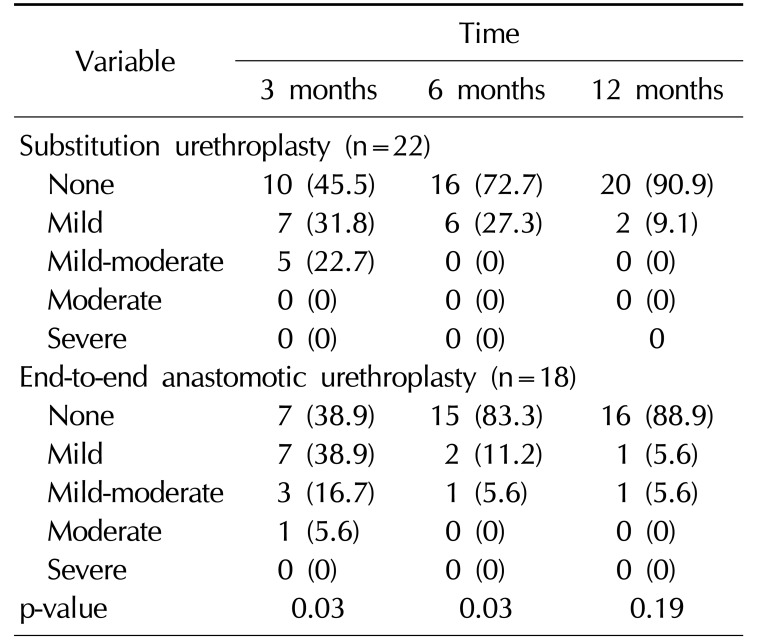
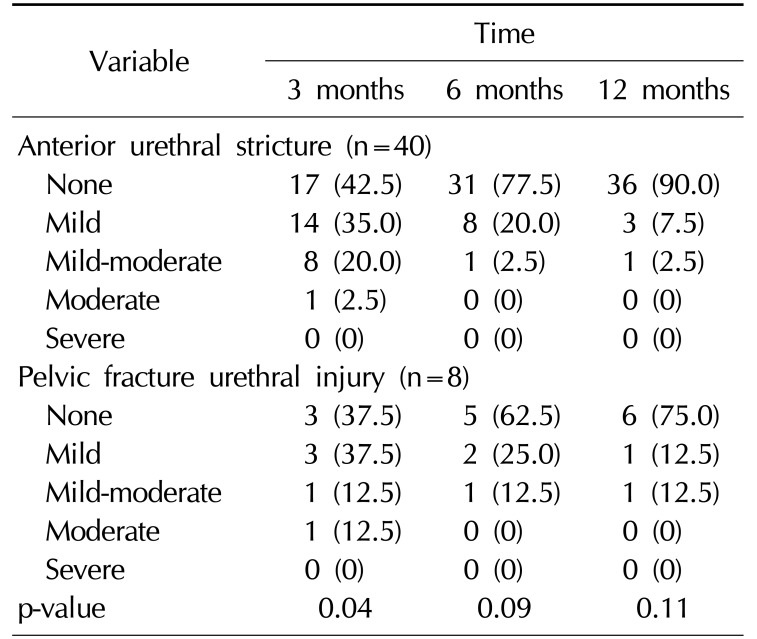
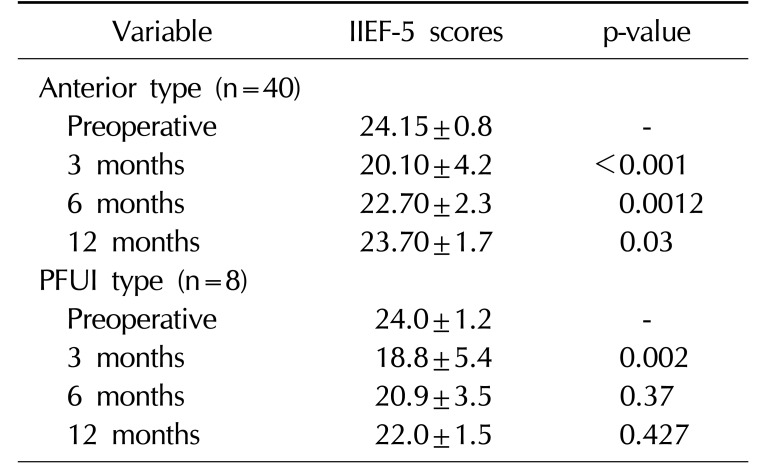
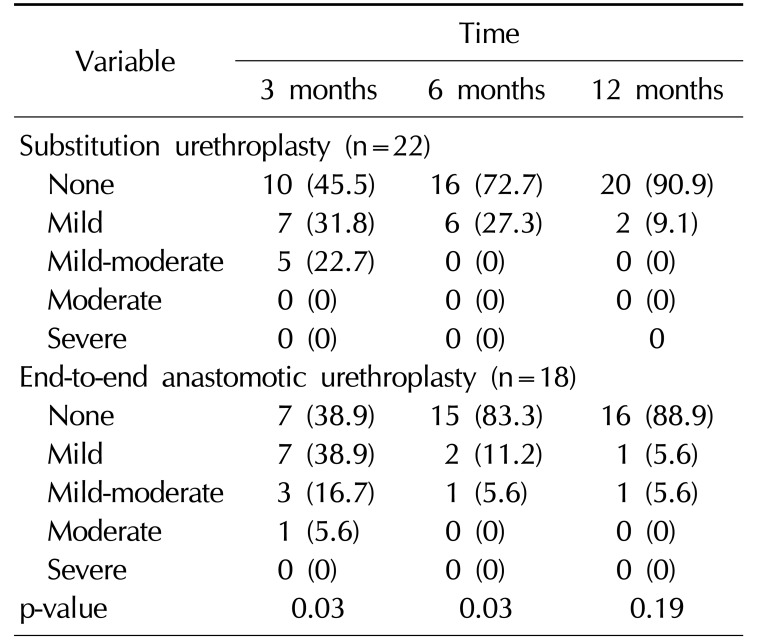
2. Erectile function in patients with an anterior urethral stricture
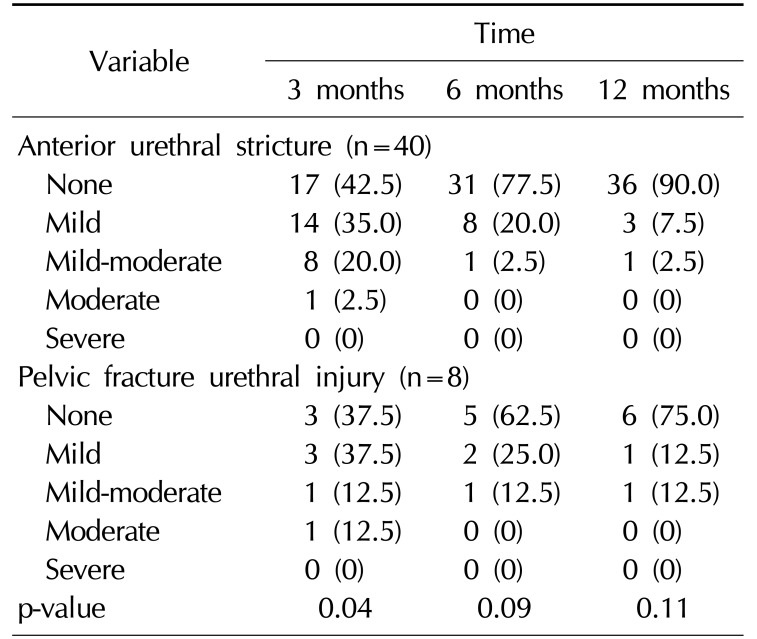
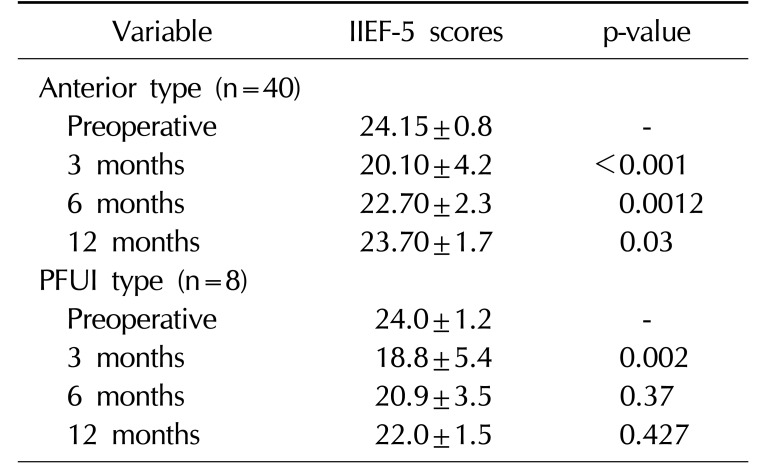
In the 40 patients undergoing urethroplasty for a stricture of the anterior urethra, ED was present in 23 patients (57.5%) at 3 months, 9 patients (22.5%) at 6 months, and 4 patients (10.0%) at 12 months (
Table 2). The mean preoperative IIEF-5 score was 24.15±0.8. At 3 months postoperatively, the mean IIEF-5 score was 20.10±4.2, showing a statistically significant decrease in erectile function. The mean IIEF-5 score was 22.70±2.3 at 6 months and 23.70±1.7 at 12 months, showing a statistically significant improvement in the recovery of erectile function (
Table 3). Among the patients with a stricture of the anterior urethra, 22 underwent SU. Out of these 22 patients, 12 patients (54.5%) had ED at 3 months, 6 patients (27.3%) at 6 months, and 2 patients (9.1%) at 12 months (Table 4). The other 18 (45%) underwent EEAU. Among the patients who underwent EEAU, 11 patients (61.1%) had ED at 3 months, 3 patients (16.7%) at 6 months, and 2 patients (11.1%) at 12 months (
Table 4,
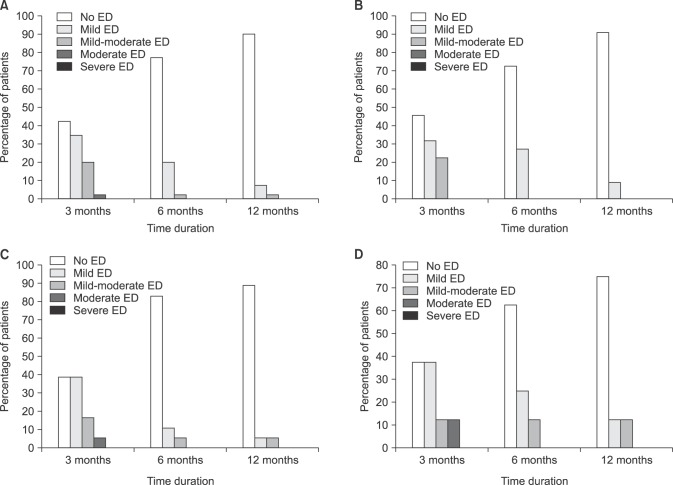
Fig. 1). We found that patients who underwent SU and EEAU had similar ED rates at 1 year postoperatively. At 3 months, the proportion of patients with normal erectile function was higher in the SU group, but at 6 months, erectile function was better in the EEAU group (
Table 4).
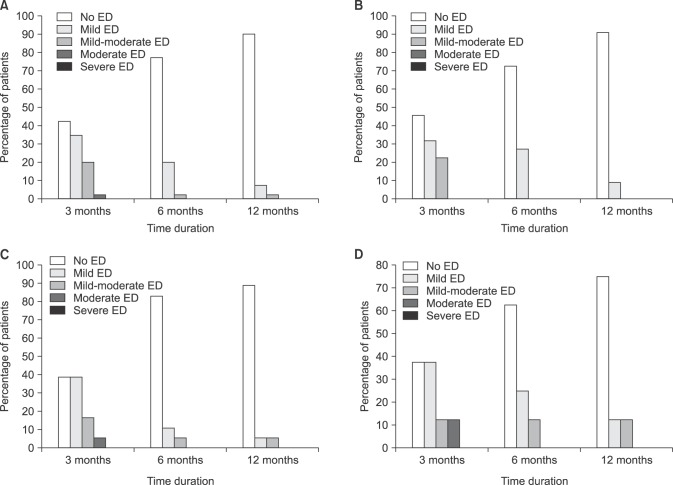 | Fig. 1Severity of erectile dysfunction (ED). Anterior urethral stricture (A), substitution urethroplasty for anterior urethral stricture (B), end-to-end anastomotic urethroplasty for anterior urethral stricture (C), pelvic fracture urethral injury (D).
|
Table 2
Severity of erectile dysfunction in patients with anterior urethral stricture and pelvic fracture urethral injury
|
Variable |
Time |
|
3 months |
6 months |
12 months |
|
Anterior urethral stricture (n=40) |
|
None |
17 (42.5) |
31 (77.5) |
36 (90.0) |
|
Mild |
14 (35.0) |
8 (20.0) |
3 (7.5) |
|
Mild-moderate |
8 (20.0) |
1 (2.5) |
1 (2.5) |
|
Moderate |
1 (2.5) |
0 (0) |
0 (0) |
|
Severe |
0 (0) |
0 (0) |
0 (0) |
|
Pelvic fracture urethral injury (n=8) |
|
None |
3 (37.5) |
5 (62.5) |
6 (75.0) |
|
Mild |
3 (37.5) |
2 (25.0) |
1 (12.5) |
|
Mild-moderate |
1 (12.5) |
1 (12.5) |
1 (12.5) |
|
Moderate |
1 (12.5) |
0 (0) |
0 (0) |
|
Severe |
0 (0) |
0 (0) |
0 (0) |
|
p-value |
0.04 |
0.09 |
0.11 |

Table 3
IIEF-5 scores at various time intervals in patients with anterior urethral stricture and PFUI
|
Variable |
IIEF-5 scores |
p-value |
|
Anterior type (n=40) |
|
|
|
Preoperative |
24.15±0.8 |
- |
|
3 months |
20.10±4.2 |
<0.001 |
|
6 months |
22.70±2.3 |
0.0012 |
|
12 months |
23.70±1.7 |
0.03 |
|
PFUI type (n=8) |
|
|
|
Preoperative |
24.0±1.2 |
- |
|
3 months |
18.8±5.4 |
0.002 |
|
6 months |
20.9±3.5 |
0.37 |
|
12 months |
22.0±1.5 |
0.427 |

Table 4
Severity of erectile dysfunction in substitution and anastomotic urethroplasty for anterior urethral stricture
|
Variable |
Time |
|
3 months |
6 months |
12 months |
|
Substitution urethroplasty (n=22) |
|
|
|
|
None |
10 (45.5) |
16 (72.7) |
20 (90.9) |
|
Mild |
7 (31.8) |
6 (27.3) |
2 (9.1) |
|
Mild-moderate |
5 (22.7) |
0 (0) |
0 (0) |
|
Moderate |
0 (0) |
0 (0) |
0 (0) |
|
Severe |
0 (0) |
0 (0) |
0 |
|
End-to-end anastomotic urethroplasty (n=18) |
|
|
|
|
None |
7 (38.9) |
15 (83.3) |
16 (88.9) |
|
Mild |
7 (38.9) |
2 (11.2) |
1 (5.6) |
|
Mild-moderate |
3 (16.7) |
1 (5.6) |
1 (5.6) |
|
Moderate |
1 (5.6) |
0 (0) |
0 (0) |
|
Severe |
0 (0) |
0 (0) |
0 (0) |
|
p-value |
0.03 |
0.03 |
0.19 |

3. Erectile function in patients who underwent urethroplasty for pelvic fracture urethral injury
In the 8 patients who underwent PPU for PFUI, 5 patients (62.5%) had ED at 3 months, 3 patients (37.5%) at 6 months, and 2 patients (25.0%) at 12 months (
Table 2) (
Fig. 1). The mean preoperative IIEF score was 24.0±1.2. At 3 months postoperatively, the mean IIEF score was 18.8±5.4, showing a statistically significant decrease in erectile function. The mean IIEF score was 20.9±3.5 at 6 months and 22.0±1.5 at 12 months, showing an improvement in the recovery of erectile function, but this improvement was not statistically significant (
Table 3). Comparing the outcomes of anterior urethral stricture with those of PFUI, we found that the recovery of erectile function in patients with PFUI was similar to that in patients with an anterior urethral stricture at 1 year postoperatively (
Table 2).
Go to :

DISCUSSION
Urethral reconstructive surgery offers a long-term cure for USD in most patients, with success rates >90% in most series [
7]. Urethroplasty has a low overall complication rate, and most patients are satisfied with their outcomes [
8].
De novo postoperative ED is an increasingly recognized complication. Due to its good surgical outcomes, single-stage urethroplasty is being performed as the first choice in most patients, while two-stage procedures are reserved for complicated, lengthy, and multiple or recurrent strictures.
Mundy [
4] was the first to comment on ED after urethroplasty in 1993, reporting a permanent ED rate of 5% after anastomotic repairs and a rate of 0.9% after graft urethroplasty. In studies that assessed postoperative erectile function at more than one time point, ED was found to be transient, resolving between 6 to 12 months in 86% of cases. Erickson et al [
7] studied the incidence of ED after anterior urethroplasty. Out of 52 patients, 20 patients (38.5%) had postoperative ED, and 18 patients recovered fully at a mean postoperative period of 190 days, ranging from 92 to 398 days.
The first study to specifically analyze ED after urethroplasty was published by Coursey et al [
9] in 2001. In this multicenter study, 250 men were retrospectively analyzed for post-urethroplasty sexual dysfunction, and nearly 30% reported some degree of postoperative ED. A control circumcision group was analyzed along with the urethroplasty group, and a similar rate of sexual dysfunction was noted. The incidence of ED following urethroplasty was 30.9%, compared to 27.3% after circumcision, highlighting the psychogenic effects on erectile function following any form of penile surgery [
9].
ED after urethroplasty is thought to be attributable to cavernous or perineal nerve injury or the disruption of bulbar arterial flow [
7]. The proposed surgical methods for reducing injury to these structures during urethroplasty include bulbospongiosus and perineal nerve preservation, bulbar artery preservation, and non-transection of the corpus spongiosum [
101112]. During PPU for PFUI, dissection is carried out more posteriorly to excise scar tissue and to gain adequate length for tension-free anastomosis. To achieve tension-free anastomosis, corporeal separation or inferior pubectomy may be needed, increasing the chances of injury to neurovascular structures and thereby increasing the likelihood that ED will develop.
In our study, the incidence of ED was greater in patients who underwent PPU for PFUI than in patients who underwent urethroplasty for an anterior urethral stricture. We used the IIEF-5 as a validated, multidimensional, self-reported instrument for the assessment of ED [
13]. The majority of patients had mild ED (IIEF score, 17~21). As time advanced, gradual improvements in erectile function were noted, underscoring the psychological impact of surgery on erectile function. When patients were assessed at 6 months and 12 months, many had recovered erectile function, and majority of those with ED exhibited mild ED.
We did not specifically assess the role of phosphodiesterase-5 inhibitors, because our goal was to assess the natural course of the disease. We also found that a slightly higher proportion of patients had ED at 6 months than was reported in other studies; however, when followed-up for 1 year, the prevalence was similar to that reported in the literature. This could be due to the minute difference in IIEF-5 scores between the no ED (IIEF score, 22~25) and mild ED (IIEF score, 17~21) categories. We trained our patients to fill the IIEF-5 questionnaire, but due to impaired comprehension as a result of their generally low educational status, we may have received improper responses. We also found that most patients with ED at 3 months showed mild ED and were able to regain normal erectile function at 6 months and at 1 year. We observed that de novo ED after urethroplasty had a good prognosis. Erectile function improved in most patients, and the degree of improvement was greater in cases of anterior urethral stricture.
PFUI occurs in approximately 10% of patients with a pelvic fracture injury, and the resulting incontinence, impotence, and urethral stricture remain a source of lifelong misery in many patients. Turner Warwick described the problem accurately by stating: “It is the urologist who will have to share the burden of the ultimate disability with the patient when the thoracic and abdominal and even the orthopedic aspects are probably long forgotten.”
Although we present a single-center study, our study has limitations. Surgery was not done by a single surgeon. It is possible that a larger study with a longer follow-up period would have allowed us to better identify the effects of urethroplasty on postoperative erectile function. We were not able to perform penile sonography due to financial constraints. The prospective nature of the study allowed each patient to serve as his own control.
Go to :

CONCLUSIONS
Patients undergoing urethroplasty for USD may develop de novo ED postoperatively. In patients with normal preoperative erectile function, the incidence of ED following surgery for PFUI was found to be similar to that following surgery for anterior urethral stricture at 1 year postoperatively. Among cases of anterior urethral stricture, recovery was better with SU at 3 months, but at 1 year the recovery was similar between patients who underwent SU and those who underwent EEAU. Erectile function should be assessed and documented in each patient before urethroplasty.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download