Abstract
Purpose
Microsurgical vasovasostomy is associated with high patency and pregnancy rates, but is difficult and requires significant effort and time to learn. Therefore, we assessed a simplified loupe-assisted vasovasostomy method using a Prolene stent.
Materials and Methods
The medical records of 82 patients who underwent loupe-assisted vasovasostomy with a Prolene stent by a single surgeon between January 2004 and December 2015 were reviewed. The association between the vasal obstructive interval (VOI) and the success rate was evaluated.
Results
The average age at the time of vasovasostomy was 39.8 years (range, 29~57 years). The mean VOI was 6.6 years (range, 1~19 years). The mean operation time was 87.0 minutes (range, 55.0~140.0 minutes). The overall patency and natural pregnancy rates were 90.2% and 45.1%, respectively. The success rate decreased as time after vasectomy increased (odds ratio, 0.869; 95% confidence interval, 0.760~0.993; p=0.039). The cases were divided into 2 groups according to the mean VOI: group A (>7 years) and group B (≤7 years), with 31 cases (37.8%) and 51 cases (62.2%), respectively. The patency and pregnancy rates of group A were 80.6% and 51.6%, respectively, while those of group B were 96.1% and 41.2%, respectively.
Vasectomy is a very common operation and is regarded as a safe and effective method of contraception worldwide [1]. Approximately 500,000 vasectomies are performed yearly in the USA [2]. In South Korea, more than 10,000 men have opted for vasectomy; this number reflects the impact a government policy of birth control that has been in place since the early 1980s [3]. In recent years, the need for vasovasostomy has risen due to the increase in divorce and remarriage and the increasing desire for more babies following vasectomy. Although vasovasostomy is usually performed to restore male fertility, it occasionally serves as a treatment for post-vasectomy pain syndrome and for secondary obstructions by infection or by iatrogenic injury, such as those caused by hernia repair. Surveys have suggested that 2% to 6% of vasectomized men may eventually seek reversal at some period in their lives [45]. Since the first vasovasostomy was performed by Quinby and O'Conor in 1915, many vasovasostomy techniques have been developed, and various success rates have been reported [6]. In 1975, Silber [7] performed the first 2-layer microsurgical vasovasostomy in the USA. Microsurgical vasovasostomy, particularly using a 2-layer technique, boasts excellent patency and pregnancy rates [8], but it is difficult and requires much effort and time to master. With the advent of the microsurgical technique, vasovasostomy has become more a specialist's undertaking. The surgeon and assistant should be familiar with microsurgery, otherwise the operation time becomes much longer. In addition, a surgical microscope is a very expensive and large device. For these reasons, vasovasostomy using a microscope is performed by only a minority of urologists. Many techniques have been subsequently described in an attempt to establish a simplified procedure. Here, we describe a simplified method for loupe-assisted vasovasostomy using a Prolene stent and assess the results of the procedure.
The study was performed with the approval and oversight of the Institutional Review Board of the Ulsan University Hospital (UUH 2016-12-034), which waived the requirement for informed consent because of the retrospective design of this study.
We performed a retrospective analysis of a single surgeon's experience with loupe-assisted vasovasostomy using a Prolene stent between January 2004 and December 2015. All men who underwent vasovasostomy were identified from hospital electronic medical records. A review of anesthesia documentation was used to calculate operation time. The operation time was based on the start and end times of the procedure, with the exception of time spent on anesthesia. The status of the testis and epididymis prior to surgery was reviewed based on a physical examination and a scrotal ultrasound. Semen analyses had also been performed to confirm azoospermia.
A total of 167 men were identified and reviewed. After the chart review, we telephoned each patient in an attempt to learn of his pregnancy status. Forty-six men who could not be contacted were excluded. Of the remaining 121 men, some were excluded from the final analysis if they required a redo operation (2), were operated on for post-vasectomy pain syndrome (1), or did not undergo postoperative semen analysis at 12 weeks (32 men). Four men who had varicocele before surgery were also excluded because it could have influenced the vasovasostomy results.
The final cohort consisted of 82 men. We divided these patients into 2 groups based on the mean vasal obstructive interval (VOI) and compared the success rates between the groups.
A 2-cm vertical scrotal incision was made at the midline. The vas deferens was grasped above and below the obstruction site using 2 vas clamps. The vas was mobilized enough to allow for tension-free anastomosis. A tagging suture was made at the testicular end of the vas, and this end was cut close to the granuloma. Semen was obtained at the cut surface of the vas and sent to the laboratory. Another tagging suture was made at the abdominal end of the vas, which was cut in the same way. The tail of a luminal stent (Prolene 3-0) was inserted into the lumen of the abdominal end of the vas (Fig. 1A). The other end of the stent had a needle that was passed through the lumen and penetrated the wall of the testicular end of the vas (Fig. 1B). Four interrupted anastomoses of the vas were performed by suturing the full layer of the vas wall and approximating the full layers of the vas, including the margin of the vasal mucosa, in order to minimize an intraluminal exposure of suture material. A 6-0 nylon suture was used to perform the anastomosis. The needle was passed from the outside to the inside of the testicular vas and then from the inside to the outside of the abdominal vas. The other side of the vasovasostomy was done in the same way. A 0.5-cm incision just 1 cm below the initial incision site was performed along the median raphe. The 2 stents were passed through the 0.5-cm incision site and tied to one another. The skin suture was performed with nylon 3-0. The luminal stent was removed after 6 weeks under local anesthesia. It was removed by a 1-cm incision in the area where the knot was palpable, and the skin was sutured using chromic 3-0 sutures.
Each participant routinely underwent a postoperative semen analysis at 6 weeks, immediately before stent removal, and then again at 12 weeks. Since the result of the former may not have accurately reflected patency due to the presence of the stent in the vas, we used the result of the latter to assess patency. All semen samples were collected by masturbation after at least 3 days of sexual abstinence. Patency was defined as the presence of motile sperm in the ejaculate. Men who did not undergo semen analyses but had a successful natural pregnancy were also regarded as having a patent anastomosis.
All statistical tests were 2-tailed, with a p-value <0.05 considered to indicate statistical significance. The association of the VOI and the success rate was evaluated using logistic regression analysis. Data were analyzed using IBM SPSS Statistics ver. 21 (IBM Co., Armonk, NY, USA).
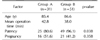
The study participants' baseline characteristics are presented in Table 1. Regarding the reason for reversal, 33 men were divorced and had remarried and 48 men wanted more babies with the same spouse. One man was in his first marriage. The mean age at the time of vasovasostomy was 39.8 years (range, 29~57 years). The mean VOI was 6.6 years (range, 1~19 years). The mean operation time was 87.0 minutes (range, 55~140 minutes). Semen analyses at the sixth week and 12th week after surgery showed sperm concentrations of 10.5 million/mL and 9.5 million/mL, respectively. The overall patency and natural pregnancy rates were 90.2% and 45.1%, respectively. The success rate decreased as time after vasectomy increased (continuous variables odds ratio, 0.869; 95% confidence interval [CI], 0.760~0.993; p=0.039). The cases were divided into two groups according to VOI: group A (>7 years) and group B (≤7 years), with 31 cases (37.8%) and 51 cases (62.2%), respectively. The patency and pregnancy rates of group A were 80.6% and 51.6%, respectively, while those of group B were 96.1% and 41.2%, respectively. Patients with a VOI ≤7 years showed higher patency rates than those with VOI >7 years (VOI >7 year odds ratio, 0.170; 95% CI, 0.032~0.905; p=0.038) (Table 2). Group A showed a higher (but not statistically significant) pregnancy rate.
Six men underwent the procedure under local anesthesia, 4 men underwent the procedure under general anesthesia, and the remaining 72 men underwent the procedure under sedation and local anesthesia. A man complained of a foreign body sensation at the surgical site and a stitch from the dartos layer was removed under local anesthesia. Another man had a mild wound problem that was treated conservatively. Four men had epididymitis that improved after conservative treatment. No complications required reoperation.
An ideal vasovasostomy procedure requires precise mucosal approximation with a watertight anastomosis. Although the 2-layer microsurgical approach remains the gold standard in vasovasostomy [910], other researchers have reported no difference in patency when comparing modified 1-layer to 2-layer anastomoses [1011]. Herrel et al [11] conducted a review of 31 English-language articles describing the results of microscopic vasovasostomy and reported a mean postoperative patency of 89.4%. We reported a 90.2% patency rate and a 45.1% pregnancy rate. The patency rates in our method were comparable to those obtained in most studies of microsurgical vasovasostomy.
The pregnancy rates associated with microscopic vasovasostomy in other studies vary (25.9%~92.5%) [1213]. This is probably due to the different definitions of pregnancy and the various follow-up periods from operation to pregnancy. Although it was not statistically significant, patients with a VOI >7 years showed higher pregnancy rates than those with a VOI ≤7 years in this study. However, these 2 groups had different follow-up periods, which could have affected the potential for natural pregnancy. Therefore, we considered patency as assessed using the more objective technique of semen analysis to be the preferable outcome for use as an indicator of a successful operation.
The 2-layer microsurgical vasovasostomy, as popularized by Silber [6], has the advantage of precise suture placement between the divided ends of the vas. The anastomosis is initiated with sutures of the inner layer to approximate the mucosa of the vas deferens. An outer layer of sutures is placed to close the seromuscular layers. However, performing a 2-layer anastomosis is time consuming and requires specific surgical skills. Therefore, a modified 1-layer vasovasostomy (MOLV) is preferred by some surgeons, because it is easier to perform and saves operating time [1415]. In the MOLV, a full-thickness suture is placed through all layers of the vas to bring the 2 ends together, followed by an additional layer of interrupted seromuscular sutures between the full-thickness sutures. In a retrospective study of 106 patients that included both the modified 1-layer and traditional 2-layer microsurgical techniques, Nyame et al [16] reported a significantly shorter operation time for MOLV (median, 120.0 minutes vs. 165.0 minutes, respectively). Although MOLV effectively reduced the operation time compared with 2-layer vasovasostomy, it still takes much more time than our method (median, 87.0 minutes) and is limited by the requirement for a microscope.
Shessel et al first reported a vasovasostomy using luminal stents (2-0 nylon) under loupe magnification in 1981 [17]. He used the exteriorized stent, and the stent was removed after a certain period of time. Despite the simplicity of the technique, this surgical method using a luminal stent has not been popular, which may be due to the refusal to expose the stent to the outside. However, in our method, the stent was not exposed to the outside.
In anastomosis of the vas, it is most important that the needle accurately passes through the lumen. The presence of the stent in the lumen helps differentiate between the lumen and the wall. With the help of the loupe magnification and the luminal stent, we were able to reduce the likelihood that the needle would pass through incorrectly. In microscopic surgery, slight movements are greatly magnified by the operating microscope and disturb the anastomosis. Since our method is possible even when a microscope is not available, it can reduce the need for general anesthesia by reducing the constraints on the location or equipment, making surgery possible even in smaller hospitals.
Previous studies have reported that the age of the female partner may have a significant effect on pregnancy rates [171819]. However, data regarding advanced age of the female partner and pregnancy rates following vasovasostomy were limited in our study. In addition, a high proportion of patients were lost to follow-up, which could have influenced our results due to potential selection bias. These factors might explain why the relationship between VOI and pregnancy success rate in our study differed from those in other studies. Another limitation of this study is that although the operations were performed by the same surgeon, they could not be directly compared to operations that were performed using microscopic surgical methods.
Figures and Tables
 | Fig. 1Photographs showing our method using the Prolene stent. (A) The tail portion of the Prolene 3-0 suture was inserted into the abdominal end of the vas. (B) The needle penetrated the wall of the testicular end of the vas. |
Table 1
Patient characteristics

References
2. Dickey RM, Pastuszak AW, Hakky TS, Chandrashekar A, Ramasamy R, Lipshultz LI. The evolution of vasectomy reversal. Curr Urol Rep. 2015; 16:40.

5. Sharma V, Le BV, Sheth KR, Zargaroff S, Dupree JM, Cashy J, et al. Vasectomy demographics and postvasectomy desire for future children: results from a contemporary national survey. Fertil Steril. 2013; 99:1880–1885.

6. Silber SJ. Microscopic vasectomy reversal. Fertil Steril. 1977; 28:1191–1202.
8. Singh I, Kaza RC. A case in favour of one sided microscopic vasovasostomy: the New Delhi experience. Int Urol Nephrol. 1996; 28:27–31.
9. Boorjian S, Lipkin M, Goldstein M. The impact of obstructive interval and sperm granuloma on outcome of vasectomy reversal. J Urol. 2004; 171:304–306.

10. Belker AM, Thomas AJ Jr, Fuchs EF, Konnak JW, Sharlip ID. Results of 1,469 microsurgical vasectomy reversals by the Vasovasostomy Study Group. J Urol. 1991; 145:505–511.

11. Herrel LA, Goodman M, Goldstein M, Hsiao W. Outcomes of microsurgical vasovasostomy for vasectomy reversal: a meta-analysis and systematic review. Urology. 2015; 85:819–825.

12. Safarinejad MR, Lashkari MH, Asgari SA, Farshi A, Babaei AR. Comparison of macroscopic one-layer over number 1 nylon suture vasovasostomy with the standard two-layer microsurgical procedure. Hum Fertil (Camb). 2013; 16:194–199.

13. Silber SJ, Grotjan HE. Microscopic vasectomy reversal 30 years later: a summary of 4010 cases by the same surgeon. J Androl. 2004; 25:845–859.

15. Sharlip ID. Vasovasostomy: comparison of two microsurgical techniques. Urology. 1981; 17:347–352.

16. Nyame YA, Babbar P, Almassi N, Polackwich AS, Sabanegh E. Comparative cost-effectiveness analysis of modified 1-layer versus formal 2-layer vasovasostomy technique. J Urol. 2016; 195:434–438.

17. Gerrard ER Jr, Sandlow JI, Oster RA, Burns JR, Box LC, Kolettis PN. Effect of female partner age on pregnancy rates after vasectomy reversal. Fertil Steril. 2007; 87:1340–1344.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download