Abstract
Purpose
Due to the increasing numbers of radical prostatectomies (RP) performed for prostate cancer, a substantial and increasing number of patients suffer from postoperative urinary incontinence and erectile dysfunction (ED). The objective of our study was to see whether an inflatable penile prosthesis implantation could control urinary incontinence for patients with the dual problems of ED and incontinence.
Materials and Methods
From March 2010 through May 2015, 25 post-RP patients were referred to our clinic with ED or incontinence. The degree of incontinence was classified according to the International Consultation on Incontinence Questionnaire-Short Form. Inflatable penile prostheses were implanted in all 25 patients.
Results
For one month after implantation, partial or full inflation was performed progressively to control urine leakage. Of 18 patients, 13 patients were categorized with mild or moderate stress incontinence. All 13 patients obtained control of incontinence with partial inflation (30% to 60%) and all reported satisfactory outcomes. Five out of the 18 patients were categorized with severe total incontinence. Three of the 5 patients could tolerate incontinence with full inflation on and off. Thirteen patients out of the total of 18 (72.2%) had their incontinence controlled by an inflating penile prosthesis.
The prevalence of urinary incontinence in men is as high as 39% and increases with age [1]. The most prevalent cause of urinary stress incontinence in men is the radical prostatectomy (RP), a standard treatment for localized prostate cancer (PCa). Postoperative incontinence is one of the most adverse complications of RP, with a major impact on quality of life. Due to the increasing number of RPs performed for PCa, a substantial and increasing number of patients suffer from postoperative stress incontinence.
With younger patients being diagnosed and living longer, there is an increasing demand for providing better health-related quality of life [23]. Despite improved surgical techniques of open, laparoscopic and robot-assisted RP, reported postoperative incontinence rates are between 5% and 48% [45]. This large variation in the rates of reported incontinence after RP may be attributed, to a certain extent, to the influence of the interviewing physician, as well as the lack of a standardized definition [67]. The treatment of post-prostatectomy incontinence consists of three different approaches: conservative, pharmacotherapeutic, and surgical treatment. Continence may improve significantly during the first year after surgery and some studies show continued improvement within the first 2 years [8]. In general, surgical intervention should be considered if the status of incontinence is stable and there is no further improvement. The artificial urinary sphincter (AUS) is still the treatment of choice for persistent incontinence. It has now been in clinical use for more than 30 years. The success rate of the AUS is still highest compared with all other treatment options. The long-term results are very good, with success rates up to 90% [9]. Despite its reliability in treating urinary incontinence, the AUS is not perfect, with complication rates up to 12%, 15% for late erosion and 7% for delayed recurrent incontinence [10]. There are also many patients who present the combined problems of incontinence and erectile failure after RP. Walsh et al [11] introduced nerve-sparing RP, and reported a postoperative potency rate 86% and continence rate of 93% [12].
It would be very advantageous if inflatable penile prosthesis implantation could prevent urinary incontinence in patients with both incontinence and erectile dysfunction (ED) since it is also an effective treatment for ED. To our knowledge, no reports are currently available about this new concept. With this idea in mind, the authors implanted inflatable penile prostheses as a first-line treatment in those patients with the dual adverse outcomes of incontinence and ED after RP, and followed the treatment effect on urinary incontinence.
From March 2010 through May 2015, 25 patients were referred to our clinic with urinary incontinence or ED after RP, from 5 different university hospitals in Seoul, Korea.
Robot-assisted RP was performed in 11 patients and open retropubic RP was performed in 14 patients. The study design was approved by the IRB (Choi's SS Clinic No 1) and informed consent was obtained in all patients. In all patients, blood chemistry, urinalysis, urinary flow rates (UFR), International Consultation on Incontinence Questionnaire-Short Form (CIQ-SF) answers, prostate specific antigen (PSA), and penile duplex ultrasonogram were recorded. Under stable conditions, the mean PSA level was 0.02 ng/dL (0.01~0.05 ng/dL). The mean maximum UFR was 21 mL/s (10~40 mL/s). The degree of incontinence was classified as follows, depending upon the scores of the ICIQ-SF: mild, 10 or less; moderate, from 11 to 17; severe, 18 or more. Prostate ultrasonography and a cystoscopic exam were done in some patients with severe leaking. All 25 patients were diagnosed with vasculogenic ED by duplex ultrasonographic study, with poor peak arterial systolic flow of less than 30 mL/s and findings of venous leakage. Out of 25 patients, 7 patients were continent and 18 patients were incontinent (Table 1).
Eighteen patients were classified according to the ICIQ-SF score as mild (5 patients), moderate (8 patients), or severe (5 patients). The mean age of the patients was 69 years (54~78 years). The waiting time to visit our clinic after RP was, on average, 3 years and 4 months (6 months~10 years).
For all 25 patients, an AMS 3-piece inflatable penile prosthesis (American Medical System, MN, USA) was implanted under local anesthesia only (caudal, pudendal, ilioinguinal, and penile) in 20 patients and under spinal anesthesia in 5 patients. Due to severe post-RP fibrosis in the pelvic cavity, the reservoir insertion was somewhat difficult in 2 patients. In one patient, the reservoir had to be implanted under the rectus muscle. The other case was complicated by a hernia, resulting in secondary herniorrhaphy. Except in the complicated cases, all patients were discharged that day or the following day.
The implanted size of the penile prosthesis was as follows: AMS CXR (American Medical System), 20 cases (14~18 cm) ; AMS CX (American Medical System), 5 cases (16~18.5 cm).
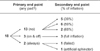
The mean length of the implanted prosthesis was 16.4 cm. The mean follow-up duration was 2 years (3 months~4 years 6 months). After the operation, incontinence was re-evaluated by self-report and by a surgeon's interview. For the primary endpoint, we asked "Do you still need a pad or other sanitary protection 24 hours per day?" For the secondary endpoint, we asked "What percent of penile inflation made you dry?"
In 25 post-RP patients, 7 patients were continent and 18 patients were incontinent. After implantation of the inflatable penile prosthesis, the 13 patients with stress incontinence achieved completely pad-free status with 30% to 60% penile inflation. They willingly maintained the partial inflation status in their ordinary daily lives. Three patients were able to control leaking on and off only by full inflation. Two patients could not control leaking even with full inflation. One of them was disappointed with this outcome, and so received a secondary artificial sphincter implantation. The pad-free success rate was 72.2% (13/18 patients) (Fig. 1).
These results show that in patients with the dual problems of ED and incontinence, an inflatable penile prosthesis could control stress incontinence except in case of total sphincteric incontinence.
Urinary incontinence and ED are well-known adverse effects after an RP for PCa. All patients undergoing RP using any surgical approach, open, laparoscopic, or robotic, are at risk of developing urinary incontinence. According to the continence definition of 'no pad', 12-month urinary incontinence rates ranged from 4% to 31%, with a mean value of 16%. Various measures have been used for evaluation of urinary incontinence, ranging from urodynamic studies to pad tests and self-reporting questionnaires including the International Prostate Symptom Score quality of life and the ICIQ-SF. These are useful tools to gauge patients' perceptions, because they enable us to obtain information about voiding and other kinds of incontinence such as urge and stress incontinence. Furthermore, the pad test is viewed as a credible, non-invasive, effective test for quantifying urine loss, and is commonly used in research as well as clinical practice.
Most studies quantify incontinence accurately, with the number of pads being used as a marker of degree [131415].
We did not use the validated instrument to assess incontinence outcomes after surgery in every case. The surgeon was the primary data gatherer, following the operation with an interview. In men, urinary continence is thought to be controlled by five main structures: the detrusor muscle, the internal sphincter, the trigonal muscles, the levator muscle, and the rhabdosphincter. The male urethral sphincter complex consists of a smooth muscle and skeletal muscle component. There are a number of explanations as to the cause of post-prostatectomy incontinence, and it is likely that it is multifactorial in origin.
During a prostatectomy, the prostate, which has a degree of control over continence as part of the proximal sphincter unit, is removed. In addition, the proximal urethral sphincter is lost; therefore, postoperative continence depends largely on the rhabdosphincter. Furthermore, the proximity of the neurovascular supply and rhabdosphincter to the prostate puts these structures at high risk of damage intraoperatively. In addition to the urethral sphincter, the bladder is also affected by RP, with effects on detrusor innervation and function. Incontinence after RP can be broadly divided into two causes: urethral and detrusor. The urethral cause of incontinence has been found to be a result of either urethral sphincter incompetence, changes in urethral length, or strictures [16]. Multiple studies have demonstrated sphincter incompetence after RP. In the majority of patients with stress incontinence, it is likely a result of sphincter injury. Intrinsic sphincter deficiency on urodynamic testing is present in up to 88% of patients postoperatively. Urodynamic testing has shown that 39.5% of post-RP patients have pure sphincteric insufficiency, with only 18.5% demonstrating no sphincteric involvement.
Maximal urethral closure pressure (MUCP) appears to be reduced postoperatively, with rates up to 41%. Similar results were demonstrated by Dubbelman et al [17], who reported significantly higher pre- and postoperative MUCP in men regaining continence at 6 months postoperatively compared with incontinent patients. They also stated that poor preoperative MUCP is an important prognostic factor for persistent incontinence postoperatively [1819]. Nerves-paring prostatectomy offers greater rates of continence due to neurovascular bundle preservation. It is likely that the combination of intraoperative nerve and neurovascular damage has effects on both the detrusor and ureteric function, and this combination results in varying degrees of incontinence and ED depending on the amount of neurovascular involvement.
In general, surgical intervention should be offered if the incontinence status is stable and no further improvement of continence can be achieved with conservative treatment up to 12 months [202122]. Among our patients, the mean duration of the wait for surgery was 3 years and 4 months (6 months~10 years). Conservative, non-invasive management of post-prostatectomy stress urinary incontinence (SUI) includes lifestyle interventions, pelvic floor muscle training with or without biofeedback, and bladder training. In some patients with additional overactive bladder symptoms, additional antimuscarinic therapy is recommended as a first-line treatment [2324]. The AUS is still the treatment of choice for persistent moderate to severe incontinence. Despite a good success rate, the AUS does carry a risk of complications such as erosion, mechanical failure, and infection. The revision rates due to mechanical failure are reported to be 8% to 45% [102526]. The first male slings for incontinence were described by Berry [27] and Kaufman [28]; however, these slings fell out of favor because of low success rates and high complication rates. There have been several new, minimally invasive sling systems introduced recently for male SUI. Male slings are an alternative for men with SUI.
Nowadays, patient demand for minimally invasive treatment options is high and will drive the choice to use a sling. In recent years, numerous minimally invasive treatment options with different success rates have been investigated. Male slings showed promising results, but lower success rates may occur [29]. Almost every currently marketed male sling is implanted in the region of the bulbar urethra. Continence is achieved due to bulbar urethral compression by these devices.
In fact, adjustability allows compression to be kept to a minimum, allowing for normal micturition without residual urine. Bulking agents such as collagen and silicone autologous fat should only be used in highly selected cases due to the low success rate [30].
Our basic concept for this study was to increase the bulbar urethral closing pressure by self-inflation of an inflatable penile prosthesis, consequently preventing urinary leakage. No reports are now available in regard to this new concept. Our study showed that urinary incontinence could be controlled by inflating the penile prosthesis to some degree (from 30% up to full rigid erection) on an as-needed basis with a more than 72.2% success rate.
Post-RP urinary incontinence can be controlled by inflating an inflatable penile prosthesis. Inflating the inflatable penile prosthesis from partial up to full rigidity increases the intra-urethral closing pressure, consequently preventing urinary leakage with an approximately 72.2% success rate. Therefore, especially in patients with the dual adverse problems of incontinence and ED after RP, the inflatable penile prosthesis is highly recommended as an initial surgical treatment.
Figures and Tables
Table 1
Characteristics of patients (n=25)

References
1. Thüroff JW, Abrams P, Andersson KE, Artibani W, Chapple CR, Drake MJ, et al. EAU guidelines on urinary incontinence. Eur Urol. 2011; 59:387–400.

2. Shamliyan TA, Wyman JF, Ping R, Wilt TJ, Kane RL. Male urinary incontinence: prevalence, risk factors, and preventive interventions. Rev Urol. 2009; 11:145–165.
3. Penson DF, McLerran D, Feng Z, Li L, Albertsen PC, Gilliland FD, et al. 5-year urinary and sexual outcomes after radical prostatectomy: results from the prostate cancer outcomes study. J Urol. 2005; 173:1701–1705.

4. Ficarra V, Novara G, Rosen RC, Artibani W, Carroll PR, Costello A, et al. Systematic review and meta-analysis of studies reporting urinary continence recovery after robot-assisted radical prostatectomy. Eur Urol. 2012; 62:405–417.

5. Loughlin KR, Prasad MM. Post-prostatectomy urinary incontinence: a confluence of 3 factors. J Urol. 2010; 183:871–877.

6. van der Poel HG, Tillier C, de Blok WM, Acar C, van Muilekom EH, van den Bergh RC. Interview-based versus questionnaire-based quality of life outcomes before and after prostatectomy. J Endourol. 2013; 27:1411–1416.

7. Lee SR, Kim HW, Lee JW, Jeong WJ, Rha KH, Kim JH. Discrepancies in perception of urinary incontinence between patient and physician after robotic radical prostatectomy. Yonsei Med J. 2010; 51:883–887.

8. Ahlering TE, Gordon A, Morales B, Skarecky DW. Preserving continence during robotic prostatectomy. Curr Urol Rep. 2013; 14:52–58.

9. Trigo Rocha F, Gomes CM, Mitre AI, Arap S, Srougi M. A prospective study evaluating the efficacy of the artificial sphincter AMS 800 for the treatment of postradical prostatectomy urinary incontinence and the correlation between preoperative urodynamic and surgical outcomes. Urology. 2008; 71:85–89.

10. Hussain M, Greenwell TJ, Venn SN, Mundy AR. The current role of the artificial urinary sphincter for the treatment of urinary incontinence. J Urol. 2005; 174:418–424.

11. Walsh PC, Marschke P, Ricker D, Burnett AL. Patient-reported urinary continence and sexual function after anatomic radical prostatectomy. Urology. 2000; 55:58–61.

12. Kundu SD, Roehl KA, Eggener SE, Antenor JA, Han M, Catalona WJ. Potency, continence and complications in 3,477 consecutive radical retropubic prostatectomies. J Urol. 2004; 172:2227–2231.

13. Kojima Y, Takahashi N, Haga N, Nomiya M, Yanagida T, Ishibashi K, et al. Urinary incontinence after robot-assisted radical prostatectomy: pathophysiology and intraoperative techniques to improve surgical outcome. Int J Urol. 2013; 20:1052–1063.

14. Moore K, Allen M, Voaklander DC. Pad tests and self-reports of continence in men awaiting radical prostatectomy: establishing baseline norms for males. Neurourol Urodyn. 2004; 23:623–626.

15. Hammerer P, Huland H. Urodynamic evaluation of changes in urinary control after radical retropubic prostatectomy. J Urol. 1997; 157:233–236.

16. Myers RP, Goellner JR, Cahill DR. Prostate shape, external striated urethral sphincter and radical prostatectomy: the apical dissection. J Urol. 1987; 138:543–550.

17. Dubbelman YD, Groen J, Wildhagen MF, Rikken B, Bosch JL. Urodynamic quantification of decrease in sphincter function after radical prostatectomy: relation to postoperative continence status and the effect of intensive pelvic floor muscle exercises. Neurourol Urodyn. 2012; 31:646–651.

18. Holm HV, Fosså SD, Hedlund H, Schultz A, Dahl AA. Severe postprostatectomy incontinence: is there an association between preoperative urodynamic findings and outcome of incontinence surgery? Scand J Urol. 2015; 49:250–259.

19. Hoyland K, Vasdev N, Abrof A, Boustead G. Post-radical prostatectomy incontinence: etiology and prevention. Rev Urol. 2014; 16:181–188.
20. Walsh PC, Partin AW, Epstein JI. Cancer control and quality of life following anatomical radical retropubic prostatectomy: results at 10 years. J Urol. 1994; 152:1831–1836.

21. Steiner MS, Morton RA, Walsh PC. Impact of anatomical radical prostatectomy on urinary continence. J Urol. 1991; 145:512–514.

22. Holm HV, Fosså SD, Hedlund H, Schultz A, Dahl AA. How should continence and incontinence after radical prostatectomy be evaluated? A prospective study of patient ratings and changes with time. J Urol. 2014; 192:1155–1161.

23. Bauer RM, Gozzi C, Hübner W, Nitti VW, Novara G, Peterson A, et al. Contemporary management of postprostatectomy incontinence. Eur Urol. 2011; 59:985–996.

24. Goode PS, Burgio KL, Johnson TM 2nd, Clay OJ, Roth DL, Markland AD, et al. Behavioral therapy with or without biofeedback and pelvic floor electrical stimulation for persistent postprostatectomy incontinence: a randomized controlled trial. JAMA. 2011; 305:151–159.
25. Gousse AE, Madjar S, Lambert MM, Fishman IJ. Artificial urinary sphincter for post-radical prostatectomy urinary incontinence: long-term subjective results. J Urol. 2001; 166:1755–1758.

26. Kim SP, Sarmast Z, Daignault S, Faerber GJ, McGuire EJ, Latini JM. Long-term durability and functional outcomes among patients with artificial urinary sphincters: a 10-year retrospective review from the University of Michigan. J Urol. 2008; 179:1912–1916.

27. Berry J. New procedure for correction of urinary incontinence: a preliminary report. J Urol. 1961; 85:771–775.
28. Kaufman JJ. Urethral compression operations for the treatment of post-prostatectomy incontinence. J Urol. 1973; 110:93–96.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download