Abstract
Purpose
This study discusses the treatment of premature ejaculation (PE) using various approaches with the goal of evaluating the methods of diagnosis and treatment of PE in clinical practice in 2014 in South Korea.
Materials and Methods
We surveyed 200 urologists and andrologists who treated patients with PE from July 1, 2014 to July 29, 2014 using an online questionnaire. The questionnaire was composed of 4 parts: disease, comorbidities, diagnosis, and treatment. Using the answers to this survey, current trends in the diagnosis and treatment of PE were investigated using weighted averages.
Results
The median number per month of patients who were diagnosed with PE was 14 patients (interquartile range, 7~24). The time to ejaculation necessary for a diagnosis of PE was considered to be <1 minute by 12% of respondents, <2 minutes by 27%, <3 minutes by 28%, <5 minutes by 13%, and 20% stated that diagnosis was based on a patient's subjective complaint. The treatment methods preferred by PE patients were reported to be pharmacological treatment (87%), surgical treatment (9.5%), and behavioral management (3.5%). The treatment methods used by respondents were pharmacological treatment (77%), surgical treatment (15%), and behavioral management (14%). The most commonly used pharmacological treatment was the oral administration of dapoxetine (97%).
According to the definition published by the International Society for Sexual Medicine (ISSM) in 2008, patients with premature ejaculation (PE) cannot achieve sexual satisfaction, and the patient and his partner feel distress and discomfort. Thus, the patient lacks confidence in himself, potentially to the point of affecting everyday life, including personal relations. Therefore, patients with PE require treatment [12]. The reported prevalence of PE has varied due to its various definitions [3]. However, PE is known to be a common type of sexual dysfunction [456].
It has been suspected that PE may occur due to genetic, neurological, psychological, urological, and/or endocrine causes, but it is not yet certain which causes are the most relevant [7]. Since the etiology of PE has not yet been clarified, a range of treatment methods such as behavioral management; pharmacological treatment, including oral medications and topical anesthetics; and surgical treatment, which remains controversial, have been developed. According to previous research, the most common treatment method is oral medication, and selective serotonin reuptake inhibitors (SSRIs) such as dapoxetine are the most commonly used oral medications. Additionally, phosphodiesterase type 5 inhibitors and tramadol may be used as oral medications [89].
In the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, released in 2013, PE is defined as involving a time to ejaculation of less than 1 minute after vaginal penetration with ejaculation occurring before the patient wants, and the symptom must be present on an ongoing basis. The symptom must occur during almost all or all sexual activities for a period of at least 6 months, which can lead to considerable frustration. Diagnosis and treatment vary depending on the definition of PE. It is important to identify how best to diagnose and treat PE in clinical practice. Thus, this study investigated the methods of diagnosis and treatment of PE in clinical practice in 2014 in South Korea.
We obtained a list of 614 urologists and andrologists (203 who worked in a general hospital and 203 who worked in other clinical settings) who had registered with the Korean Society for Sexual Medicine and Andrology. We asked them to participate in the survey using email from July 1, 2014 to July 29, 2014. A total of 200 respondents (50 who worked in a general hospital and 150 who worked in other clinical settings) who treated patients with PE agreed to participate and completed the questionnaire (response rate, 32.5%).
The questionnaire was composed of the following 4 parts: disease, comorbidities, diagnosis, and treatment. In the disease section, the first question asked respondents to identify the average number of patients who sought care due to their PE symptoms per month and the ratio of patients who were actually diagnosed with PE among those who were seen, and the second question asked about the age distribution of patients who visited with a complaint of PE. In the comorbidities section, the first question asked participants to identify which disease most commonly accompanied PE. The second question asked participants to identify the ratio of patients who had both erectile dysfunction and PE. The third question was a multiple-response question asking about the treatment method used for patients who had erectile dysfunction and PE. In the diagnosis section, multiple-response questions asked about the standard times to ejaculation used to diagnose PE, whether the survey respondents utilized the premature ejaculation diagnostic tool (PEDT) [10], which patients were diagnosed using the PEDT if the survey respondents used the PEDT, and if the survey respondents did not use the PEDT, they were asked why they did not use it. In the treatment section, multiple-response questions were used to survey which factors were considered in the treatment of PE, which treatment methods were preferred by patients in descending order, and the ratio of treatment methods that were employed. Additionally, multiple-response questions were used to assess which medications were prescribed as oral PE medications and how clinicians guided patients in maximizing the effects of oral medications, as well as difficulties experienced regarding prescribing the medication after diagnosis.
Using the answers, the current status of diagnosis and treatment of PE in the field was assessed using averages that were weighted according to the number of the patients who were diagnosed with PE. Survey crafter ver. 4.0.15 (Survey Crafter, Inc., Acton, MA, USA) was used for all statistical analyses.
Of the survey respondents, 25% worked in general hospitals and 75% worked in other clinical settings. Urology was the major field of 99% of respondents, while the remaining 1% identified themselves as working in the field of andrology. The gender distribution was 99% male and 1% female. The number of years of experience of medical specialists was 1~10 years for 23% of respondents, 11~20 years for 46% of respondents, 21~30 years for 27% of respondents, and more than 31 years for 5% of respondents, with an average of 17 years. The age distribution of survey respondents was as follows: 12% were 30~39 years old, 47% were 40~49 years old, 32% were 50~59 years old, 9% were 60~69 years old, and 1% were 70~79 years old, with an average age of 49.00±7.74 years.
The median number of patients counseled for PE per month was 20 patients (interquartile range [IQR], 10~40 patients), and the median number of patients who were actually diagnosed with PE was 14 patients (IQR, 7~24 patients). The age distribution of PE patients was as follows: 21% of patients were in their 20s, 29% were in their 30s, 29% were in their 40s, and 21% were in their 50s or older.
Erectile dysfunction was the most commonly observed comorbidity in patients visiting for PE symptoms (58% of patients), while the other comorbidities were as follows: prostatitis (25%), psychological disorders (3%), prostate hypertrophy (2%), and no comorbidity (10%). Regarding treatment, 60% of respondents indicated that medication for erectile dysfunction was prescribed first, and if that medication did not show any effects, PE medication was prescribed subsequently. Additionally, 57% of answers described the co-administration of medication for erectile dysfunction and PE, while 10% of answers stated that medication was only prescribed for erectile dysfunction, 9% indicated surgical treatment, and 8% described behavioral management.
For the diagnosis of PE, the standard time to ejaculation was considered to be less than 1 minute by 12% of respondents, less than 2 minutes by 27% of respondents, less than 3 minutes by 28% of respondents, less than 5 minutes by 13% of respondents, and a patient's subjective complaint by 20% of respondents. Of the respondents, 42% stated that they used the PEDT. If the PEDT was not utilized, respondents were asked why in a multiple-response question, to which 63% of respondents who did not use the PEDT answered that they thought that the patient's subjective symptoms were more important, while 40% of respondents stated that they did not use the PEDT due to limitations in counseling time, 27% of respondents answered that they did not think it was necessary, 16% of respondents stated that it had insufficient diagnostic value, 16% of respondents replied that it was not helpful for treatment, 12% of respondents indicated that patients did not want the test, and 4% of respondents answered that they were not aware of the questionnaire.
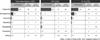
Multiple responses were used to assess the factors necessary to consider in PE treatment. Stability was indicated by 71% of the respondents, the price of the drug by 69%, comorbidities of the patient by 64%, PE type (primary or secondary) by 60%, adverse events by 55%, convenience and easy administration by 52%, the age of the patient by 46%, the physician's experience with prescribing the drug by 42%, the manufacturer of the drug by 12%, and insurance coverage by 12%. The treatment methods most preferred by PE patients were reported to be pharmacological treatment (87%), surgical treatment (9.5%), and behavioral management (3.5%). Adding patients' first and second choices together, pharmacological treatment was chosen by 100% of respondents, surgical treatment by 65%, and behavioral management by 35%. Respondents who worked in a general hospital had the following breakdown of responses: pharmacological treatment, 100%; surgical treatment, 44%; and behavioral management, 56%. The corresponding answers from respondents who worked in other clinical settings were as follows: pharmacological treatment, 100%; surgical treatment, 72%; and behavioral management, 27%. The treatment methods employed by the respondents were investigated, and it was found that 77% of respondents reported using pharmacological treatment, 15% reported using surgical treatment, and 14% indicated that they used behavioral management (Fig. 1). The oral PE medication prescribed by respondents was also investigated in a multiple-response question. Of the respondents, 97% prescribed dapoxetine, 59% prescribed clomipramine, and 35% prescribed SSRIs such as sertraline, fluoxetine, and paroxetine (Fig. 2). In response to the question about obstacles to prescribing medication, the first-ranked answer was objections from the patient regarding the drug price (42%), followed by patients' resistance to taking medication regularly despite acknowledging its necessity (38%), and patients' preferences for a one-time treatment, such as surgical treatment (14%). However, when the first-ranked and second-ranked answers were added together, the most common answer was patients' resistance to taking medication regularly despite acknowledging its necessity (78%) (Fig. 3).
Shindel et al [11] reported that the majority of the urologists in the United States diagnosed PE based on patients' complaints, and that on-demand SSRI therapy was the most commonly selected first line of treatment. Since the diagnosis is made only on the basis of subjective factors, the diagnosis rate varies among physicians. In this study, it can be seen that consultations regarding PE took place more frequently in general hospitals than in clinics, but that PE was diagnosed in a higher percentage of cases in clinics, which may be explained by the tendency of non-hospital clinics to have more relaxed criteria.
The PEDT is used as a tool to objectively diagnose PE [12]. The PEDT contains 5 questions, and it can be used to diagnose PE based on the sum of scores of 0 to 4 points for each item. In this study, respondents stated that they did not use the PEDT because they thought that the patients' subjective symptoms were more important or due to limitations in counseling time. This shows that in numerous cases, respondents still diagnose PE based on subjective symptoms. It also seems that additional research is needed regarding the diagnostic value of the PEDT as an objective tool for the more accurate diagnosis and assessment of PE.
The squeeze technique and the stop-start technique were widely used as behavioral management strategies [13]. However, these behavioral managements require a partner's help and are associated with recurrence. However, a study reported that behavioral management together with the pharmacological treatment led to more effective treatment than the pharmacological treatment alone [14]. In fact, 14% of respondents indicated using behavioral management, so it is clearly a relevant treatment method.
In the 1970s, delayed ejaculation was observed in men who were taking SSRIs for depression. Thus, antidepressants such as clomipramine and SSRIs including fluoxetine, paroxetine, and sertraline were used to treat PE [13151617]. This reflects off-label use, since these medications have not been approved for PE. Dapoxetine is a SSRI with a short half-life, and it is the first drug to have been approved for PE treatment. In several studies, the effectiveness of dapoxetine has been demonstrated, and it is currently widely used around the world [181920]. In this study, dapoxetine was found to be the most widely prescribed medication. Jiann and Huang [21] reported that the satisfaction rate and response rate to dapoxetine treatment were 45.0% and 74.6%, respectively, demonstrating a gap between the efficacy of dapoxetine and patient expectations regarding the treatment of PE. However, in this study, off-label medications were found to be widely used, especially in non-hospital clinics, which may be due to the relatively expensive price of dapoxetine and pressure from patients who want to keep taking previous medications.
The surgical treatment of PE is controversial due to the lack of academic proof of its efficacy. Surgical treatment is not included in the guidelines of the European Association of Urology on PE. Additionally, the ISSM guidelines state that there is a lack of evidence regarding PE surgery, and that it may cause sexual dysfunction and is therefore not recommended [22]. It has also been reported that circumcision was not found to help treat PE [23]. However, one study reported that selective neurectomy of the dorsal nerves of the penis was an effective treatment of PE [24]. In 2004, it was announced that penis augmentation using hyaluronic acid is a safe and effective way to reduce sensation in the glans, and that 68% of patients were satisfied with this treatment [25]. In this study, it was found that respondents working in non-hospital clinics thought that patients preferred surgical treatment to a greater extent than the respondents working in general hospitals, and that they showed a relative preference for surgical treatment (3% vs. 18%). These results confirm those that have been reported in earlier studies [26].
The most commonly observed comorbidity in patients seeking care for PE was erectile dysfunction (58%). Respondents were asked about treatment methods for male patients with PE and erectile dysfunction, and the 60% of the answers stated that medication for erectile dysfunction was prescribed first, and if the medication did not lead to any improvement, PE medication was prescribed afterward. Previous studies have found that if a patient has erectile dysfunction and PE at the same time, it is more effective for the erectile dysfunction medication to be taken first [2728].
Participants were asked to rank obstacles in prescribing medication for patients, and the first-ranked answer was objections from patients regarding drug prices. Thus, the price of oral medication is an important factor in PE treatment. Moreover, some patients prefer surgical treatment because it only requires a one-time treatment. These are the challenges that oral medication must overcome (Fig. 3).
The principal limitation of this study is that it did not survey all urologists. In addition, by using weighted averages, the medical practices of clinicians who examine many PE patients may have been overemphasized. Despite these limitations, not been enough studies have been performed on the diagnosis and treatment of PE in clinical practice. Our study will be a useful aid in the treatment of patients with PE. Further studies with larger sample sizes are necessary to more accurately characterize the diagnosis and treatment of PE in clinical practice.
In 2014 in South Korea, various diagnostic methods and treatment methods were used for PE. The most commonly used treatment was the oral administration of dapoxetine. Additionally, it was found that surgical treatment was performed in some cases. If diagnostic criteria and treatment methods are standardized by the establishment of PE guidelines via large, prospective studies, better therapeutic results may be expected.
Figures and Tables
Fig. 1
(A) Treatment methods preferred by premature ejaculation patients. (B) Treatment methods employed by respondents. GH: general hospital, CL: other clinical environments. *The use of a cream was not provided as an answer choice, but was volunteered by a respondent.

References
1. McMahon CG, Althof SE, Waldinger MD, Porst H, Dean J, Sharlip ID, et al. An evidence-based definition of lifelong premature ejaculation: report of the International Society for Sexual Medicine (ISSM) ad hoc committee for the definition of premature ejaculation. J Sex Med. 2008; 5:1590–1606.

2. Rowland DL, Patrick DL, Rothman M, Gagnon DD. The psychological burden of premature ejaculation. J Urol. 2007; 177:1065–1070.

3. Rowland DL, Kolba TN. Understanding the effects of establishing various cutoff criteria in the definition of men with premature ejaculation. J Sex Med. 2015; 12:1175–1183.

4. Rosen RC. Prevalence and risk factors of sexual dysfunction in men and women. Curr Psychiatry Rep. 2000; 2:189–195.

5. Rowland D, Perelman M, Althof S, Barada J, McCullough A, Bull S, et al. Self-reported premature ejaculation and aspects of sexual functioning and satisfaction. J Sex Med. 2004; 1:225–232.

6. Laumann EO, Nicolosi A, Glasser DB, Paik A, Gingell C, Moreira E, et al. Sexual problems among women and men aged 40-80 y: prevalence and correlates identified in the global study of sexual attitudes and behaviors. Int J Impot Res. 2005; 17:39–57.

8. Gökçe A, Halis F, Demirtas A, Ekmekcioglu O. The effects of three phosphodiesterase type 5 inhibitors on ejaculation latency time in lifelong premature ejaculators: a double-blind laboratory setting study. BJU Int. 2011; 107:1274–1277.

9. Kirby EW, Carson CC, Coward RM. Tramadol for the management of premature ejaculation: a timely systematic review. Int J Impot Res. 2015; 27:121–127.

10. Kam SC, Han DH, Lee SW. The diagnostic value of the premature ejaculation diagnostic tool and its association with intravaginal ejaculatory latency time. J Sex Med. 2011; 8:865–871.

11. Shindel A, Nelson C, Brandes S. Urologist practice patterns in the management of premature ejaculation: a nationwide survey. J Sex Med. 2008; 5:199–205.

12. Symonds T, Perelman MA, Althof S, Giuliano F, Martin M, May K, et al. Development and validation of a premature ejaculation diagnostic tool. Eur Urol. 2007; 52:565–573.

13. Goodman RE. The management of premature ejaculation. J Int Med Res. 1977; 5:1 Suppl. 78–79.
14. Cormio L, Massenio P, La Rocca R, Verze P, Mirone V, Carrieri G. The combination of dapoxetine and behavioral treatment provides better results than dapoxetine alone in the management of patients with lifelong premature ejaculation. J Sex Med. 2015; 12:1609–1615.

15. Waldinger MD, Hengeveld MW, Zwinderman AH. Paroxetine treatment of premature ejaculation: a double-blind, randomized, placebo-controlled study. Am J Psychiatry. 1994; 151:1377–1379.
16. Wise TN. Sertraline as a treatment for premature ejaculation. J Clin Psychiatry. 1994; 55:417.
17. Kara H, Aydin S, Yücel M, Agargün MY, Odabaş O, Yilmaz Y. The efficacy of fluoxetine in the treatment of premature ejaculation: a double-blind placebo controlled study. J Urol. 1996; 156:1631–1632.

18. Yue FG, Dong L, Hu TT, Qu XY. Efficacy of dapoxetine for the treatment of premature ejaculation: a meta-analysis of randomized clinical trials on intravaginal ejaculatory latency time, patient-reported outcomes, and adverse events. Urology. 2015; 85:856–861.

19. Mirone V, Arcaniolo D, Rivas D, Bull S, Aquilina JW, Verze P. PAUSE study team. Results from a prospective observational study of men with premature ejaculation treated with dapoxetine or alternative care: the PAUSE study. Eur Urol. 2014; 65:733–739.

20. Buvat J, Tesfaye F, Rothman M, Rivas DA, Giuliano F. Dapoxetine for the treatment of premature ejaculation: results from a randomized, double-blind, placebo-controlled phase 3 trial in 22 countries. Eur Urol. 2009; 55:957–967.

21. Jiann BP, Huang YJ. Assessing satisfaction in men with premature ejaculation after dapoxetine treatment in real-world practice. Int J Clin Pract. 2015; 69:1326–1333.

22. Althof SE, Abdo CH, Dean J, Hackett G, McCabe M, McMahon CG, et al. International Society for Sexual Medicine's guidelines for the diagnosis and treatment of premature ejaculation. J Sex Med. 2010; 7:2947–2969.

23. Morris BJ, Krieger JN. Does male circumcision affect sexual function, sensitivity, or satisfaction?: a systematic review. J Sex Med. 2013; 10:2644–2657.
24. Zhang GX, Yu LP, Bai WJ, Wang XF. Selective resection of dorsal nerves of penis for premature ejaculation. Int J Androl. 2012; 35:873–879.

25. Kim JJ, Kwak TI, Jeon BG, Cheon J, Moon DG. Effects of glans penis augmentation using hyaluronic acid gel for premature ejaculation. Int J Impot Res. 2004; 16:547–551.

26. Yang DY, Ko K, Lee WK, Park HJ, Lee SW, Moon KH, et al. Urologist's practice patterns including surgical treatment in the management of premature ejaculation: a Korean nationwide survey. World J Mens Health. 2013; 31:226–231.

27. McMahon CG, Giuliano F, Dean J, Hellstrom WJ, Bull S, Tesfaye F, et al. Efficacy and safety of dapoxetine in men with premature ejaculation and concomitant erectile dysfunction treated with a phosphodiesterase type 5 inhibitor: randomized, placebo-controlled, phase III study. J Sex Med. 2013; 10:2312–2325.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download