Abstract
Purpose
To assess the prevalence of phosphodiesterase 5 (PDE5) inhibitor use and associated factors among University of Gondar undergraduate students.
Materials and Methods
An institution-based, cross-sectional study, using a survey questionnaire, was conducted from October to December 2015 to assess PDE5 inhibitor use and associated factors among male students at the University of Gondar. A Self-Esteem and Relationship questionnaire (14 items), an International Index of Erectile Function questionnaire (15 items) and a questionnaire on PDE5 inhibitor use (14 items) were included in the survey.
Results
Across all respondents (age, 21.9±1.88 years), more than half (55.7%, n=233) had heard about PDE5 inhibitors, but only 23 men (5.5%) reported trying a PDE5 inhibitor drug at least once. Older students were more likely to use PDE5 inhibitors compared to younger students (adjusted odds ratio [AOR], 1.40; 95% confidence interval [CI], 1.109~1.768). Those students who were smokers were 5.15 times more likely to use PDE5 inhibitors as compared to their non-smoking counterparts (AOR, 5.15; 95% CI, 2.096~12.687). In addition, multivariate logistic regression showed that being in a relationship, alcohol use, greater number of cigarettes smoked per day, and more sexual partners were significantly associated with PDE5 inhibitor use.
Conclusions
The prevalence of PDE5 inhibitor use among undergraduate students was 5.5%. Cigarette smoking and other substance use, older age, and greater number of sexual partners were significantly associated factors for PDE5 inhibitor use. These findings suggest that restricting access to PDE5 inhibitor drugs is essential to curtailing misuse among university students.
Erectile dysfunction (ED) aka impotence is defined as the inability to achieve or maintain an erection sufficient for satisfactory sexual performance [1]. It is a relatively common medical problem and is estimated to affect 322 million people worldwide, of whom 30 million live in Africa [2].
Phosphodiesterase 5 (PDE5) inhibitors such as sildenafil (Viagra), tadalafil (Cialis), and vardenafil (Levitra, Vivanza) are drugs approved by the United States Food and Drug Administration for the treatment of ED. Though these drugs are only approved for ED, many young healthy men use PDE5 inhibitors for sexual enhancement. Mounting evidence has identified a trend of recreational use of PDE5 inhibitors in combination with illicit drugs for sexual enhancement without medical indication [345]. Studies have identified several risk factors associated with PDE5 inhibitors, such as greater number of sexual partners, unprotected sexual relations, and sexually transmitted diseases [67].
In Ethiopia, alcohol, khat (Catha edulis), and tobacco are the most frequently used recreational substances and the rate of substance use is increasing, particularly in the younger population [8910]. Due to a lack of strong regulations, these PDE5 inhibitors can be easily accessed without prescriptions from pharmacies [11]. Although psychoactive substance use has become common practice among university students in Ethiopia, no studies have assessed the rate of PDE5 inhibitor use or its associated factors. Thus, we proposed to assess the prevalence of PDE5 inhibitor use and associated factors among University of Gondar (UOG) undergraduate students.
This institution-based, cross-sectional study was conducted from October to December 2015 to assess PDE5 inhibitor use and associated factors among male students at the UOG, Ethiopia. UOG is located in Gondar, in the Amhara region of Northwest Ethiopia. The university has a total of 12,248 male students enrolled at various campuses. The study used a quantitative data collection method and included all regular undergraduate students attending UOG.
The sample size was calculated using a single population proportion formula for a population greater than 10,000 (12,248 regular students). The sample was obtained using a proportional stratified random sampling technique. During the first stage, all 5 campuses were selected and the number of students from each campus was determined proportionally based on the number of students attending each campus. Undergraduate students from each campus were selected using a computer-generated simple random sampling technique. Using a 4% margin of error at 95% confidence level, the sample size was 572 after considering a 10% nonresponse rate.
A brief survey questionnaire containing open-ended and multiple-choice questions was distributed to a cohort of undergraduate students. The anonymous responses were collected by hand from each participant and they were provided with a period of 15 to 20 minutes to finish the questionnaire during their leisure time.
The 52-item survey-questionnaire was divided into 5 domains: (1) an assessment of personal and epidemiological data (7 items), (2) an assessment of sexual intercourse experience (2 items), (3) the Self-esteem and Relationship (SEAR) questionnaire (14 items), (4) the International Index of Erectile Function (IIEF) questionnaire (15 items), and (5) an assessment of PDE5 inhibitor use (14 items).
The SEAR questionnaire was used to assess sexual relationship scores ranging from 0 to 100 (transformed scores) and to classify them according to a validated tool [12]. The IIEF-15 questionnaire, containing 15 items, was used to assess erectile function [13]. A 17-item questionnaire was used to assess PDE5 inhibitor use among undergraduate students.
All statistical analysis was performed using IBM SPSS ver. 22 (IBM Co., Armonk, NY, USA). Summary statistics of sociodemographic data, sexual intercourse history, and extent of PDE5 inhibitor use were presented using frequency and percentages. Mean and standard deviation were used to summarize SEAR and IIEF scores. Binary logistic regression was performed to determine the associated factors contributing to PDE5 inhibitor use. Significant risk factors identified by binary logistic regression analysis were included in the multiple logistic regression. Odds ratios (OR) with 95% confidence intervals (95% CI) were also computed, along with their p-values. A p<0.05 was set as statistically significant.
The study protocol was approved by the institutional Review Board of the School of Pharmacy, University of Gondar, Ethiopia. Prior to survey questionnaire administration, written consent was obtained from each participant. Only those participants who consented to participate were included in the study. Confidentiality of the information provided by the participants was ensured by not disclosing the information. And consent to publish was obtain from the School of Pharmacy and also obtained from study participants.
The response rate was 73.1% (n=418). Nearly nine-tenths of the respondents were single (89.4%, n=355) with a mean age of 21.9±1.88 years. More than two-thirds (69.4%, n=290) of the respondents were Orthodox Christians and from middle-income families (57.4%, n=240). One-third (30.6%, n=128) of student participants were in their second year of study and students from the Technology (27.5%, n=115), Health Sciences (26.3%, n=110), and Social Sciences (24.6%, n=103) campuses actively participated in the study. When asked about substance use, nearly six-tenths (58.9%, n=246) reported that they drink alcohol. Half of the respondents reported that they had engaged in sexual activity (50.7%, n=212) in the previous 6 months (Table 1).
The overall scores for the study participants from the SEAR questionnaire (1~14 items) assessing the domains of sexual relationships (1~8 items) and confidence (9~14 items), including self-esteem (9~12 items) and overall relationship (13~14 items) are shown in Table 2. The mean score of the first domain, sexual relationship (1~8 items), was 62.4±19.4 (range, 25~100); nearly one-third (29.7%) of participants showed severe ED with poor sexual relations according to the SEAR scale. The second domain, confidence (self-esteem and overall relationship) was 68.0±17.8 (range, 12.5~100), with a greater number of participants with moderate (32%) to severe ED (31.1%). The self-esteem (9~12 items) subdomain of the confidence domain mean score was 67.6±19.1 (range, 18.7~100) and the majority scored more than 80. The overall relationship mean score (13~14 items) was 69.4±25.3 (range, 37.5~100) and nearly half of participants scored less than 77 (48.1%).
The mean IIEF score of men was 21.6±4.52 (range, 6~30); the organism function score was 7.3±2.00 (range, 3~10); the sexual desire score was 6.8±1.75 (range, 2~10); the intercourse satisfaction score was 10.0±2.42 (range, 2~15), and overall satisfaction was 7.8±1.88 (range, 2~10) (Fig. 1). More than six-tenths (62.3%) showed some degree of ED according to the IIEF scale.
Across all respondents, more than half (55.7%, n=233) had heard about PDE5 inhibitors, but only 23 (5.5%) men recorded trying a PDE5 inhibitor drug at least once. Among those men, 10 participants specified sildenafil and the remaining 13 were unable to recall the type of PDE5 inhibitors used. Most of the PDE5 inhibitor users took these drugs rarely (n=14), and 18 specified the exact dosage of the PDE5 inhibitors used. The motivation behind PDE5 inhibitor use was to increase erectile sensation (n=9), increase rigidity (n=8), enhance self-esteem (n=7) and to impress/satisfy the partner (n=4). However, the majority of the PDE5 inhibitor users reported that they used it along with illicit drugs (marijuana, shisha, and hashish; n=14). Participants also agreed that they could easily access PDE5 inhibitor drugs without a prescription (n=15) and obtain them through friends (n=13). When asked about their experience of PDE5 inhibitor use, 18 men reported a satisfactory to excellent experience, but reported that they experienced headache (n=8), blurred vision (n=5), and longer duration of action (n=4) after using PDE5 inhibitors. Many reported that they would like to use PDE5 inhibitors again (n=11) (Table 3).
Table 4 indicates sociodemographic and behavioral factors assumed to be associated with PDE5 inhibitor use among the study participants. Age, being in a relationship, alcohol use, cigarette smoking, and beliefs about the effect of illicit substances on sexual relations were found to be significantly associated with PDE5 inhibitor use in multivariate logistic regression analysis. In particular, older students were more likely to use PDE5 inhibitors compared to younger students (adjusted OR [AOR], 1.40; 95% CI, 1.109~1.768). Those students who were smokers were 5.15 times more likely to use PDE5 inhibitors as compared to their counterparts (AOR, 5.15; 95% CI, 2.096~12.687). Furthermore, multivariate logistic regression showed that being in a relationship, alcohol use, greater number of cigarettes smoked per day, and more sexual partners were found to be significantly associated with PDE5 inhibitor use (Table 4).
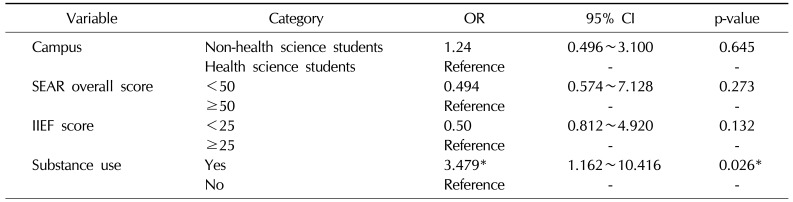
Binary logistic regression data are given in Table 5. Study campus, SEAR scores, and erectile function were not associated with PDE5 inhibitor use in the binary logistic regression analysis (p>0.05). The only significant factors were substance use (OR, 3.479; 95% CI, 1.162~10.416; p=0.026).
Many population-based studies have reported the recreational use of PDE5 inhibitors among young men aged 18 to 44 years [451114]. Indeed, these drugs are approved for treating ED patients, but young healthy men may wish to use them to enhance their sexual performance. This use without indication can have an impact on sexual function, relationships with partners, and self-esteem. Moreover, very few studies have addressed the use of PDE5 inhibitors in students [3151617]. This is the first study reporting the prevalence of PDE5 inhibitor use among university students in Ethiopia.
Through this investigation, we identified that PDE5 inhibitors were used as a recreational drug by 5.5% of the participants, which is consistent with the study of Musacchio et al [18] (6%) conducted on college students in the United States. Although the prevalence of PDE5 inhibitor use here is comparably much lower than what was found in a Brazilian study [3], our findings may suggest that PDE5 inhibitor use by young male students is becoming a problem in Ethiopia. Our population reported that they used PDE5 inhibitors to enhance their sexual performance by improving erectile sensation and increasing penile rigidity. Similar to other studies, a high percentage (71.5%) of PDE5 inhibitor users liked to use them with alcohol and other illicit drugs [3181920]. More than half (56.5%) received these drugs from a friend, and they also reported that they can easily access PDE5 inhibitors as non-prescribed drugs. This unexpected risky behavior may lead to adverse consequences and such a finding necessitates further in-depth investigation to better understand these issues.
We used 2 standardized and validated questionnaires to investigate undergraduate students' sexual relationships, using the SEAR questionnaire and IIEF-15 to address their sexual confidence. The scores reflected overall good sexual relationship and confidence levels, with no pervasive ED. However, 30% of the sample exhibited a ≤50 score for sexual relationship, 20.3% had lower confidence levels, and nearly 45% reported a ≤60 score, indicating ED according to the SEAR. These findings were lower than those of previous studies conducted on medical students and young adult ED patients treating with sildenafil [2122]. Similarly, only 7.5% had ED according to IIEF-15. Our findings indicate a relatively high rate of severe ED in university students, which raises concerns. Previous studies indicated that underlying psychological problems were one of the predictive risk factors associated with severe ED in young men [2123]. Psychological issues have a particular impact on the wellbeing of both partners and more emphasis is needed on addressing psychological impediments in order to improve all aspects of sexual aspiration. The Global Better Sex Survey reported out of the 48% of young men with a degree of ED, 18% showed a prevalence of severe ED, but very few had taken a medication for ED [24]. This indicates that there is an unmet need to focus on sexual health, particularly in young men.
The transition from high school to college is a critical developmental period and a time when young men may engage in unprotected sex, especially those with many perceived health risk factors. PDE5 inhibitor drugs should be used only for ED under the direct supervision of healthcare providers. Illegal access to these drugs and concurrent use with potentially hazardous substances like alcohol or other illicit drugs might carry additional health risks. In this study, nearly two-thirds of PDE5 inhibitor users reported that they can easily obtain the drugs through a friend, from pharmacies without prescriptions, or from other sources. In addition, more than half of these drug users would like to use them again, which raises concerns about risky behavior in young students. With regards to substance use, cigarette smoking showed a statistically significant association with higher odds of recreational use of PDE5 inhibitors, more so than other substances (AOR, 5.15; 95% CI, 2.096~12.687). However in the study of Korkes et al [3], nearly three-fourths (71.4%) of young medical students mixed alcohol with PDE5 inhibitors. In binary logistic regression, recreational substance users were 3.4 times more likely to also use PDE5 inhibitors as compared to non-substance users. The recreational use of PDE5 inhibitors with other substances can have potentially serious side effects. Moreover, most of the PDE5 inhibitor users frequently reported side effects such as headache, blurred vision, longer duration of action, and dizziness; these side effects have also been reported in previous studies [3425].
We used 2 standardized SEAR and IIEF questionnaires with a cross-sectional study method to assess erectile function, sexual relationships, and confidence. Open-ended questions were limited in the questionnaire and the study was pilot-tested. In addition, PDE5 inhibitor use was tested using a different questionnaire to reduce recall bias.
However, the study is not without limitations. First, this study was cross-sectional and conducted at a single institution; therefore, the findings should be interpreted carefully when trying to establish a causal relationship. In addition, it may be difficult to generalize the findings to the whole body of undergraduate students studying at different universities in Ethiopia. Finally, data presented here is self-reported, and some of the participants may provide extreme responses as compared to others, according to the beliefs and motivations of the participants, which might be subject to recall bias.
The prevalence of PDE5 inhibitor use among undergraduate students was 5.5%. Cigarette smoking and other substance use, older age, and greater number of sexual partners were significantly associated factors for PDE5 inhibitor use. These findings suggest that restricting access to PDE5 inhibitor drugs is essential for curtailing misuse among university students. Further studies focusing on psychosocial determinants of ED and PDE5 inhibitor use in the younger population are warranted.
ACKNOWLEDGEMENTS
We wish to express our sincere gratitude to the School of Pharmacy at the University of Gondar for the support and guidance they provided during the course of this study. We also would like to acknowledge the study participants for consenting to participate in the study.
References
1. NIH Consensus Conference. Impotence. NIH consensus development panel on impotence. JAMA. 1993; 270:83–90. PMID: 8510302.
2. Ayta IA, McKinlay JB, Krane RJ. The likely worldwide increase in erectile dysfunction between 1995 and 2025 and some possible policy consequences. BJU Int. 1999; 84:50–56. PMID: 10444124.
3. Korkes F, Costa-Matos A, Gasperini R, Reginato PV, Perez MD. Recreational use of PDE5 inhibitors by young healthy men: recognizing this issue among medical students. J Sex Med. 2008; 5:2414–2418. PMID: 18331258.

4. Bechara A, Casabé A, De Bonis W, Helien A, Bertolino MV. Recreational use of phosphodiesterase type 5 inhibitors by healthy young men. J Sex Med. 2010; 7:3736–3742. PMID: 20722788.

5. Lowe G, Costabile R. Phosphodiesterase type 5 inhibitor abuse: a critical review. Curr Drug Abuse Rev. 2011; 4:87–94. PMID: 21696344.

6. Mitchell KR, Prah P, Mercer CH, Datta J, Tanton C, Macdowall W, et al. Medicated sex in Britain: evidence from the third National Survey of Sexual Attitudes and Lifestyles. Sex Transm Infect. 2016; 92:32–38. PMID: 26092974.

7. Li J, McDaid LM. Alcohol and drug use during unprotected anal intercourse among gay and bisexual men in Scotland: what are the implications for HIV prevention. Sex Transm Infect. 2014; 90:125–132. PMID: 24345556.

8. Gebreslassie M, Feleke A, Melese T. Psychoactive substances use and associated factors among Axum University students, Axum Town, North Ethiopia. BMC Public Health. 2013; 13:693. PMID: 23895376.

9. Mossie TB, GebreMichael GB, Ayele AD. Magnitude of psychoactive substance abuse among university students, Adigrat, North Ethiopia: cross-sectional study. J Psych. 2015; 18:281.

10. Dingeta T, Oljira L, Assefa N. Patterns of sexual risk behavior among undergraduate university students in Ethiopia: a cross-sectional study. Pan Afr Med J. 2012; 12:33. PMID: 22891091.
11. Both R. A matter of sexual confidence: young men's non-prescription use of Viagra in Addis Ababa, Ethiopia. Cult Health Sex. 2016; 18:495–508. PMID: 26555512.

12. Cappelleri JC, Althof SE, Siegel RL, Shpilsky A, Bell SS, Duttagupta S. Development and validation of the Self-Esteem And Relationship (SEAR) questionnaire in erectile dysfunction. Int J Impot Res. 2004; 16:30–38. PMID: 14963468.

13. Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997; 49:822–830. PMID: 9187685.

14. Kimura M, Shimura S, Kobayashi H, Tai T, Chikano Y, Baba S, et al. Profiling characteristics of men who use phosphodiesterase type 5 inhibitors based on obtaining patterns: data from the nationwide Japanese population. J Sex Med. 2012; 9:1649–1658. PMID: 22513057.

15. Harte CB, Meston CM. Recreational use of erectile dysfunction medications in undergraduate men in the United States: characteristics and associated risk factors. Arch Sex Behav. 2011; 40:597–606. PMID: 20358273.

16. Duryea DG, Calleja NG, MacDonald DA. Nonmedical use of prescription drugs by college students with minority sexual orientations. J College Stud Psychother. 2015; 29:147–159.

17. Freitas VM, Menezes FG, Antonialli MM, Nascimento JW. Use of phosphodiesterase-5 inhibitors by college students. Rev Saude Publica. 2008; 42:965–967. PMID: 18797570.
18. Musacchio NS, Hartrich M, Garofalo R. Erectile dysfunction and viagra use: what's up with college-age males? J Adolesc Health. 2006; 39:452–454. PMID: 16919814.

19. Campbell N, Clark JP, Stecher VJ, Thomas JW, Callanan AC, Donnelly BF, et al. Adulteration of purported herbal and natural sexual performance enhancement dietary supplements with synthetic phosphodiesterase type 5 inhibitors. J Sex Med. 2013; 10:1842–1849. PMID: 23634714.

20. Santtila P, Sandnabba NK, Jern P, Varjonen M, Witting K, von der Pahlen B. Recreational use of erectile dysfunction medication may decrease confidence in ability to gain and hold erections in young males. Int J Impot Res. 2007; 19:591–596. PMID: 17657209.

21. Shindel AW, Ferguson GG, Nelson CJ, Brandes SB. The sexual lives of medical students: a single institution survey. J Sex Med. 2008; 5:796–803. PMID: 18208500.

22. Yang Y, Liu R, Jiang H, Hong K, Zhao L, Tang W, et al. Association between dosage frequency and the treatment outcomes of sildenafil in young and middle-aged men with erectile dysfunction: a chinese, multicenter, observational study. Urology. 2015; 86:62–67. PMID: 26142584.

23. Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: prevalence and predictors. JAMA. 1999; 281:537–544. PMID: 10022110.
24. Mulhall J, King R, Glina S, Hvidsten K. Importance of and satisfaction with sex among men and women worldwide: results of the global better sex survey. J Sex Med. 2008; 5:788–795. PMID: 18284556.

25. Hornung M, Halila GC, Barbosa V. Prevalence of universities that make use of medicines for erectile dysfunction treatment. Visão Acadêmica. 2012; 13:27–32.
Fig. 1
Mean scores±standard deviations of International Index of Erectile Function (IIEF) questionnaire (n=212).
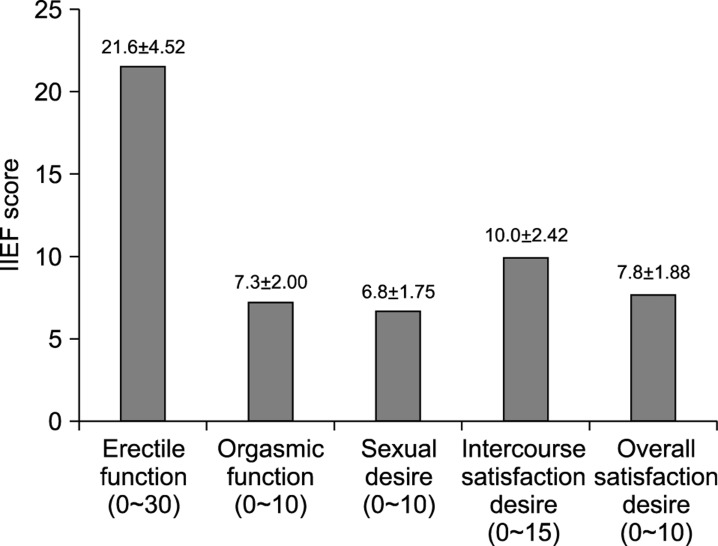
Table 1
Personal and epidemiological characteristics (n=418)
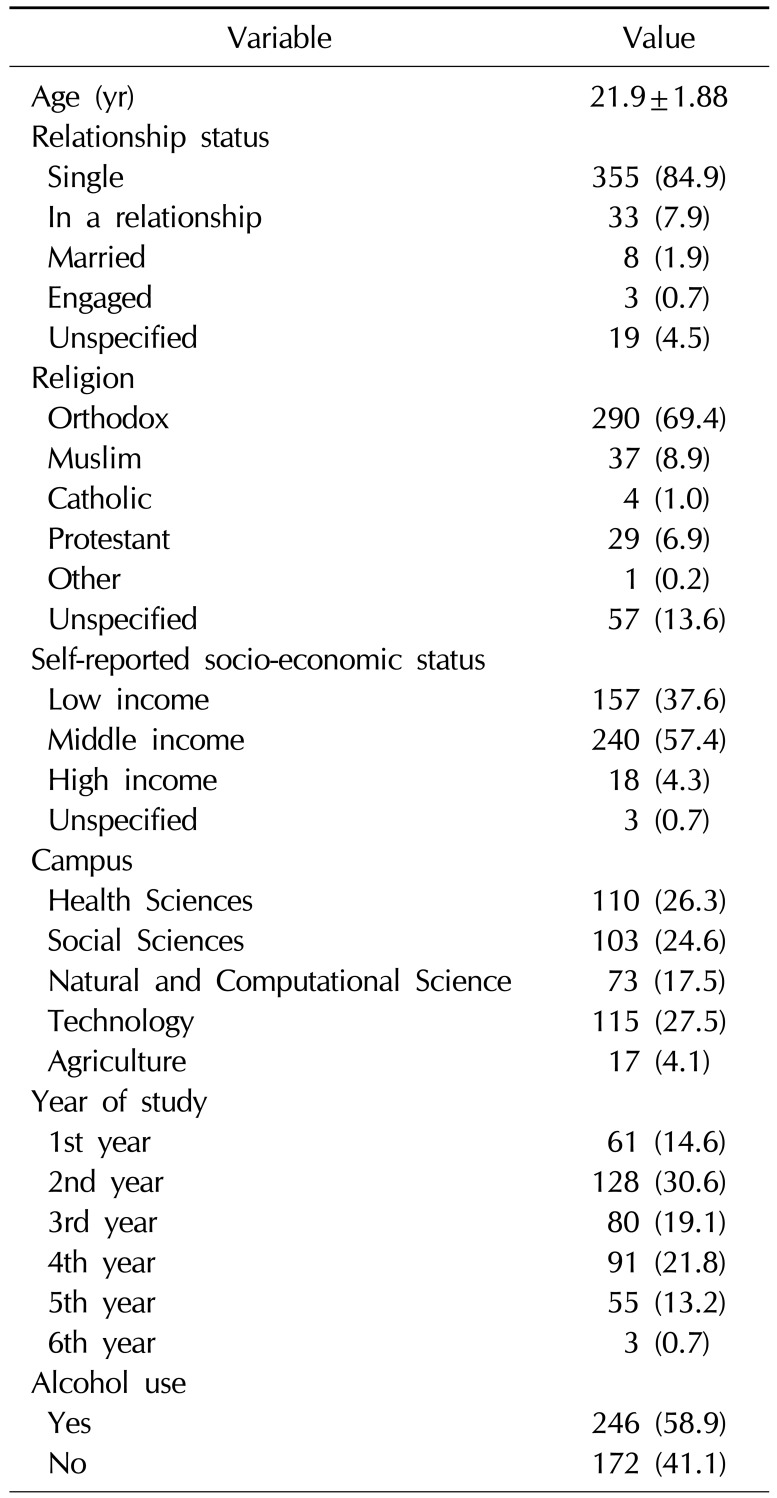
Table 2
Evaluation of ED according to self-esteem and relationship questionnaire (n=212)
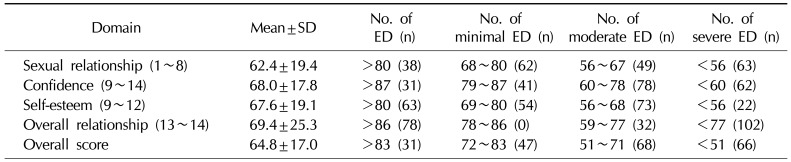
Table 3
Phosphodiesterase 5 inhibitors (PDE5I) use
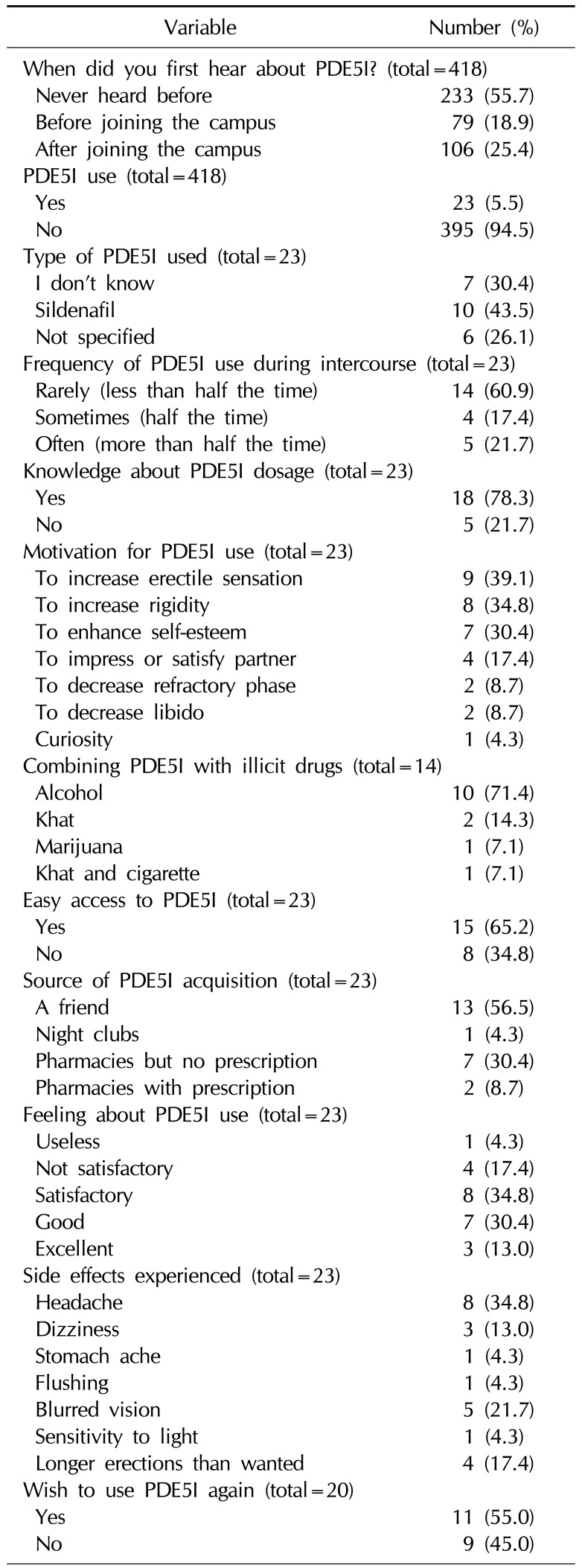
Table 4
Bivariate and multivariate logistic regression analysis of socio-demographic data and phosphodiesterase 5 inhibitor use
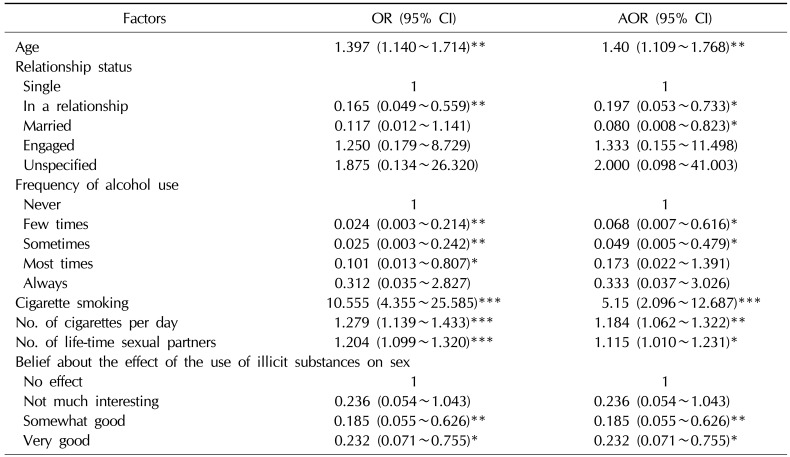
Table 5
Binary logistic regression between phosphodiesterase 5 inhibitors use among undergraduate students (n=418)




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download