Abstract
Purpose
Prostate tumor volume calculated after surgery using pathologic tissue has been shown to be an independent risk factor for biochemical recurrence. Nonetheless, prostate size varies among individuals, regardless of the presence or absence of cancer. We assumed to be lower margin positive rate in the surgical operation, when the prostate volume is larger and the tumor lesion is same. Thus, we defined the tumor-prostate ratio in the ratio of tumor volume to prostate volume. In order to compensate the prostate tumor volume, the effect of tumor-prostate ratio on biochemical recurrence was examined.
Materials and Methods
This study included 251 patients who underwent open retropubic radical prostatectomy for prostate cancer in a single hospital. We analyzed the effects of tumor volume and tumor-prostate ratio, as well as the effects of known risk factors for biochemical recurrence, on the duration of disease-free survival.
Results
In the univariate analysis, the risk factors that significantly impacted disease-free survival time were found to be a prostate-specific antigen level ≥10 ng/mL, a tumor volume ≥5 mL, tumor-prostate ratio ≥10%, tumor capsular invasion, lymph node invasion, positive surgical margins, and seminal vesicle invasion. In the multivariate analysis performed to evaluate the risk factors found to be significant in the univariate analysis, positive surgical margins (hazard ratio=3.066) and a tumor density ≥10% (hazard ratio=1.991) were shown to be significant risk factors for biochemical recurrence.
Numerous studies have been conducted to determine factors effecting the prognosis of patients after radical prostatectomy, especially regarding the recurrence of localized prostate cancer. Prostate-specific antigen (PSA) levels, the Gleason score after radical prostatectomy, the postoperative pathological tumor grade, and positive surgical margins are important independent prognostic factors that have been used to predict whether prostate cancer has been completely cured in a given patient [1].
Prostate tumor volume is associated with cancer cell differentiation, necrosis, and neovasculature, which are important factors reflecting the biological condition of a tumor [23]. In the treatment of localized prostate cancer, prostate cancer volume may reflect its clinical progression. Nevertheless, discordant results have been reported regarding whether tumor volume is an independent predictor for the postoperative prognosis of prostate cancer. Although several studies have reported tumor volume to be associated with biochemical recurrence following radical prostatectomy, this hypothesis is still highly controversial. We speculated that the source of this controversy may be the diversity of prostate volume among patients. In other words, given a constant tumor volume, the rate of positive surgical margins in cases with a relatively large prostate volume may be lower than in cases with a relatively small prostate volume.
Based on this possibility, we investigated whether the ratio of tumor volume to prostate volume was an independent risk factor for the biochemical recurrence of prostate cancer after radical prostatectomy.
This study was conducted on 251 patients who underwent open retropubic radical prostatectomy for prostate cancer in a Severance Hospital from 1998 to 2005. Patients who received preoperative hormone therapy or whose tumor volume was not measured after the surgery were excluded.
Preoperatively, in each patient, prostate volume was measured via prostate ultrasonography and PSA levels were measured through a blood test. Additionally, in patients suspected to have prostate cancer based on those results, prostate cancer was definitively diagnosed via prostate biopsy. The Gleason score was obtained in patients diagnosed with prostate cancer. This study included only patients definitively diagnosed with prostate cancer who underwent radical prostatectomy and whose postoperative tumor volume could be measured using a computer. Prostate volume was calculated by converting the weight recorded in the pathology report to volume, applying the Stanford protocol based on the entire pathological tissue. Tumor volume was calculated by summing up the volume of all tumors within the prostate using a same method.
The definition of biochemical recurrence following radical prostatectomy was at least two instances of PSA levels increasing by more than 0.02 ng/mL. We used univariate analysis to determine the risk factors associated with biochemical recurrence, including the parameters examined preoperatively, tumor volume, and tumor-prostate ratio, by assessing their effect on the duration of disease-free survival. Multivariate analysis was then performed to analyze the risk factors that showed a significant relationship in the univariate analysis. Additionally, the following postoperative parameters were included in the analysis: pathological disease stage, PSA level, prostate volume, tumor volume, final Gleason score, and the presence of positive margins. Tumor-prostate ratio was calculated as the ratio of tumor volume to prostate volume, and was incorporated into the analysis.
To evaluate the effect of each factor on biochemical recurrence following surgery, statistical analysis was performed. Univariate analysis was performed using Kaplan-Meier survival analysis. Multivariate analysis was performed using a Cox proportional hazard model. In all statistical analyses were performed using SPSS Statistics ver. 10.0 (SPSS Inc., Chicago, IL, USA). A p<0.05 were considered to indicate statistical significance.
The characteristics of the 251 patients who underwent radical prostatectomy were examined. When classified based on the volume of the prostate 40 mL; 156 patients (62.2%) were found to have had smaller values, while 95 patients (37.8%) were found to have had larger values. When classified based on the PSA 10 ng/mL; 125 patients were found to have had higher values, while 126 patients were found to have had lower values. Among the patients who underwent surgery, 102 patients (40.6%) exhibited positive surgical margins (Table 1). In the univariate analysis, the risk factors found to be significantly associated with biochemical recurrence were a PSA level ≥10 ng/mL (p=0.009), tumor volume ≥5 mL (p<0.05), capsular invasion (p=0.009), lymph node invasion (p=0.008), and positive surgical margins (p=0.000) (Table 2). In addition, tumor-prostate ratio ≥10% showed a significant effect on biochemical recurrence (p=0.007) (Fig. 1).
In the multivariate analysis performed on the risk factors established to be significant within the univariate analysis, positive surgical margins (hazard ratio [HR]=3.066, p=0.000) and tumor-prostate ratio ≥10% were shown to be significant risk factors for biochemical recurrence (HR=1.991, p=0.026) (Table 3).
Radical prostatectomy is still the most important treatment of prostate cancer. Complete resection of the prostate allows prostate cancer to be almost completely cured, and numerous urologists employ this treatment modality. However, complete resection cannot always be accomplished. Due to various factors, such as differences in surgical experience, the effect of previous hormone therapy, and efforts to reduce the injury to the neurovascular bundles in order to improve the quality of life of the patient after surgery, invasion of the surgical margins is occasionally detected in the postoperative pathological findings. Therefore, efforts have been made to determine the optimal resection method based on the preoperative condition of the patient and predictions regarding postoperative progression. With this goal in mind, preoperative prognostic factors have been identified. In addition, postoperative prognostic factors determining whether additional hormone therapy or radiation therapy is required also play an important role.
Positive surgical margins have been confirmed as an important postoperative prognostic factor [4]. Due to the careful selection of patients for surgery and improvements in surgical techniques, the incidence of positive surgical margins has dramatically decreased over the past 20 years. Presently, open abdominal surgery methods, such as the suprapubic approach and the perineal approach, do not show significantly different outcomes from laparoscopic techniques [567]. That is, the incidence of positive surgical margins due to the surgical method used or differences in individual technique can be overcome by ensuring adequate familiarity with the surgical methods. In addition, biochemical recurrence, which is strongly associated with surgical outcome, may not be very different from each surgical methods. However, tumor volume has also been suggested to have a predictive effect in patients clinically diagnosed with localized prostate cancer who undergo radical prostatectomy, as it may affect the incidence of positive surgical margins. Nevertheless, the use of tumor volume as a prognostic factor remains controversial. In an analysis of the pathological reports of 200 specimens of radical prostatectomy, McNeal [8] found that tumor volume was strongly associated with the Gleason score, the pathological disease stage, surgical margin invasion, and seminal vesicle invasion. Subsequently, Stamey et al [1] reported a mutual association of tumor volume with cancer progression. Nelson et al [9] reported that tumor volume was a significant independent predictive factor. However, several studies have reported different results. Noguchi et al [10] reported that PSA levels were not a significant factor predicting biochemical recurrence after radical prostatectomy in men with large volume cancer. Marks et al [11] reported that univariate analysis showed tumor volume to be a risk factor for biochemical recurrence, but in multivariate analysis, only PSA levels, disease stage, and the Gleason score were found to be significant. In addition, several studies have argued that although tumor volume may have some value as a prognostic factor, it is less useful than other parameters because it is cumbersome to calculate. It has been suggested that methods measuring the maximal tumor diameter should be introduced in order to address this issue, and that the ratio of high-grade tumors should be incorporated [121314]. As such, although it is intuitive that the tumor volume during surgery may have an effect, no consensus exists in the literature. This may be due to two issues. The first has to do with differences in the methods used to measure tumor volume. Prostate tumors are rarely present in only one area within the prostate; instead, they show an irregular and scattered pattern. Hence, it is not easy to calculate the tumor volume. The method that classifies pathological specimens into groups of 1%, 5%, 10%, or 20% based on microscopy incorporates many variables, such as the number of specimen blocks and the number of specimens containing signs of prostate cancer [15]. This procedure may fail to detect small tumors [16]. Another method is to calculate the tumor volume using computerized analysis. Although this is a more accurate method, it is not always performed [171819]. In our study, a computerized volume summation analysis method was used to calculate tumor volume. Nonetheless, the prognostic value of tumor volume remains unclear. It may be the case that prostate volume affects the likelihood of positive surgical margins as well. In other words, in two patients with the same tumor volume but with different prostate volumes, the likelihood of the tumor cells reaching the surgical margins would be higher in the patient with the smaller prostate volume (Fig. 2).
In our results, tumor volume appeared to have a significant effect in the univariate analysis, but this was not confirmed in the multivariate analysis. Instead, tumor-prostate ratio and positive surgical margins were shown to be independent significant risk factors. Additional studies are required to adequately understand the additional significance of tumor-prostate ratio as a parameter. In addition, we obtained interesting results regarding lymph node invasion and seminal vesicle invasion. Although lymph node invasion was found to be a significant factor for biochemical recurrence in the univariate analysis, it was not found to be significant in the multivariate analysis. It has been generally shown that lymph node invasion typically takes place in fewer than 1% of cases with a PSA level <10 ng/mL. In our study, lymph node invasion was observed in 0.4% of cases with a PSA level <10 ng/mL, in contrast to in 3.2% of cases with a PSA level ≥10 ng/mL. Lymph node invasion occurred in 3.6% of cases with a Gleason score ≥7. Lymph node invasion was not detected in any cases with a Gleason score <7. Such results are consistent with those of previous studies arguing that it is not always necessary to send out frozen nodes for intraoperative analysis in cases with a PSA level <10 ng/mL and a Gleason score <7 [20].
Few studies have evaluated the prognostic value of seminal vesicle invasion. Epstein et al [21] and Ohori et al [22] reported that seminal vesicle invasion was not significantly associated with the prognosis. Potter et al [23] reported that seminal vesicle invasion can be pathologically classified into several types, with potentially different prognoses. Similarly, in our study, no association of seminal vesicle invasion with biochemical recurrence was observed. Additional studies on seminal vesicle invasion may be required.
In cases of localized or locally advanced prostate cancer, tumor-prostate ratio was found to be an independent risk factor for biochemical recurrence following prostatectomy, along with positive surgical margins. This may explain the previous contradictory results regarding tumor volume.
Figures and Tables
Fig. 1
Biochemical recurrence-free survival according to tumor density, using a cutoff of 10% (p=0.007).
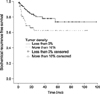
Fig. 2
A schematic illustrating a hypothetical scenario in which one patient has a larger prostate than the other, with identical tumor volumes. The patient with the smaller prostate will likely have a worse prognosis.

Table 1
Characteristics of the patients who underwent radical prostatectomy

Table 2
Univariate analysis of the risk factors for biochemical recurrence

References
1. Stamey TA, McNeal JE, Yemoto CM, Sigal BM, Johnstone IM. Biological determinants of cancer progression in men with prostate cancer. JAMA. 1999; 281:1395–1400.

2. Nicholson B, Theodorescu D. Angiogenesis and prostate cancer tumor growth. J Cell Biochem. 2004; 91:125–150.

3. Epstein JI, Carmichael M, Partin AW, Walsh PC. Is tumor volume an independent predictor of progression following radical prostatectomy? A multivariate analysis of 185 clinical stage B adenocarcinomas of the prostate with 5 years of followup. J Urol. 1993; 149:1478–1481.

4. Bostwick DG, Grignon DJ, Hammond ME, Amin MB, Cohen M, Crawford D, et al. Prognostic factors in prostate cancer. College of American Pathologists Consensus Statement 1999. Arch Pathol Lab Med. 2000; 124:995–1000.
5. Korman HJ, Leu PB, Goldstein NS. A prospective comparison of anatomic radical perineal and retropubic prostatectomy specimens: are surgical margins equivalent? Prostate Cancer Prostatic Dis. 2000; 3:S22.

6. Brown JA, Garlitz C, Gomella LG, Hubosky SG, Diamond SM, McGinnis D, et al. Pathologic comparison of laparoscopic versus open radical retropubic prostatectomy specimens. Urology. 2003; 62:481–486.

7. Rassweiler J, Seemann O, Schulze M, Teber D, Hatzinger M, Frede T. Laparoscopic versus open radical prostatectomy: a comparative study at a single institution. J Urol. 2003; 169:1689–1693.

8. McNeal JE. Cancer volume and site of origin of adenocarcinoma in the prostate: relationship to local and distant spread. Hum Pathol. 1992; 23:258–266.

9. Nelson BA, Shappell SB, Chang SS, Wells N, Farnham SB, Smith JA Jr, et al. Tumour volume is an independent predictor of prostate-specific antigen recurrence in patients undergoing radical prostatectomy for clinically localized prostate cancer. BJU Int. 2006; 97:1169–1172.

10. Noguchi M, Stamey TA, McNeal JE, Yemoto CM. Preoperative serum prostate specific antigen does not reflect biochemical failure rates after radical prostatectomy in men with large volume cancers. J Urol. 2000; 164:1596–1600.

11. Marks RA, Koch MO, Lopez-Beltran A, Montironi R, Juliar BE, Cheng L. The relationship between the extent of surgical margin positivity and prostate specific antigen recurrence in radical prostatectomy specimens. Hum Pathol. 2007; 38:1207–1211.

12. Alschibaja M, Wegner M, Massmann J, Funk A, Hartung R, Paul R. Prostate cancer volume: can it be predicted preoperatively? Urol Int. 2005; 75:354–359.
13. Eichelberger LE, Koch MO, Eble JN, Ulbright TM, Juliar BE, Cheng L. Maximum tumor diameter is an independent predictor of prostate-specific antigen recurrence in prostate cancer. Mod Pathol. 2005; 18:886–890.

14. Chun FK, Briganti A, Jeldres C, Gallina A, Erbersdobler A, Schlomm T, et al. Tumour volume and high grade tumour volume are the best predictors of pathologic stage and biochemical recurrence after radical prostatectomy. Eur J Cancer. 2007; 43:536–543.

15. Humphrey PA, Vollmer RT. Percentage carcinoma as a measure of prostatic tumor size in radical prostatectomy tissues. Mod Pathol. 1997; 10:326–333.
16. Srigley JR. Key issues in handling and reporting radical prostatectomy specimens. Arch Pathol Lab Med. 2006; 130:303–317.

17. Renshaw AA, Chang H, D'Amico AV. Estimation of tumor volume in radical prostatectomy specimens in routine clinical practice. Am J Clin Pathol. 1997; 107:704–708.

18. Noguchi M, Stamey TA, McNeal JE, Yemoto CE. Assessment of morphometric measurements of prostate carcinoma volume. Cancer. 2000; 89:1056–1064.

19. Chen ME, Johnston D, Reyes AO, Soto CP, Babaian RJ, Troncoso P. A streamlined three-dimensional volume estimation method accurately classifies prostate tumors by volume. Am J Surg Pathol. 2003; 27:1291–1301.

20. Epstein JI, Amin M, Boccon-Gibod L, Egevad L, Humphrey PA, Mikuz G, et al. Prognostic factors and reporting of prostate carcinoma in radical prostatectomy and pelvic lymphadenectomy specimens. Scand J Urol Nephrol Suppl. 2005; (216):34–63.

21. Epstein JI, Carmichael M, Walsh PC. Adenocarcinoma of the prostate invading the seminal vesicle: definition and relation of tumor volume, grade and margins of resection to prognosis. J Urol. 1993; 149:1040–1045.

22. Ohori M, Wheeler TM, Kattan MW, Goto Y, Scardino PT. Prognostic significance of positive surgical margins in radical prostatectomy specimens. J Urol. 1995; 154:1818–1824.

23. Potter SR, Epstein JI, Partin AW. Seminal vesicle invasion by prostate cancer: prognostic significance and therapeutic implications. Rev Urol. 2000; 2:190–195.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download