Abstract
Purpose
To perform a systematic review and meta-analysis of randomized controlled trials (RCTs) comparing monopolar transurethral resection of the prostate (MTURP) and photoselective vaporization of the prostate (PVP) in order to provide the most up-to-date and reliable recommendations possible.
Materials and Methods
Relevant RCTs were identified from electronic databases for meta-analysis of the surgical outcomes and complications of MTURP and PVP. Meta-analytical comparisons were made using qualitative and quantitative syntheses. The outcome variables are presented as odds ratios with 95% confidence intervals (CIs).
Results
In total, 11 articles were included in this comparative analysis of PVP versus MTURP. Most of the recently published studies exhibited low risk in terms of quality assessment. MTURP was superior to PVP regarding operative time; however, with regard to catheterization and hospitalization time, the mean differences were -1.39 (95% CI=-1.83~-0.95, p<0.001) and -2.21 (95% CI=-2.73~-1.69, p<0.001), respectively, in favor of PVP. PVP was superior to MTURP with regard to transfusion rate and clot retention, but no statistically significant differences were found with regard to acute urinary retention and urinary tract infection. The long-term complications of bladder neck contracture and urethral stricture showed no statistically significant differences between PVP and MTURP. Long-term functional outcomes, including the International Prostate Symptom Score and maximum flow rate, likewise did not display statistically significant differences between PVP and MTURP.
Male lower urinary tract symptoms (LUTS) are one of the most common clinical symptoms encountered in adult men, and have a major impact on quality of life [1]. Male LUTS are commonly due to bladder outlet obstruction secondary to benign prostatic hyperplasia (BPH) [2]. In such patients, medical treatments, including alpha-blockers, 5-alpha-reductase inhibitors, muscarinic receptor antagonists, and low-dose tadalafil, are preferred, but surgery is an option for patients with bothersome LUTS due to benign prostatic obstruction (BPO) who do not desire to undergo medical treatment, in cases where medication does not prove efficacious, and in cases of complicated LUTS. Monopolar transurethral resection of the prostate (MTURP) has been the standard surgical procedure for men with prostate sizes of 30~80 mL and bothersome moderate-to-severe LUTS secondary to BPO [3]. However, over the last decades, various innovative transurethral surgical procedures have been developed to supplement or replace transurethral resection of the prostate (TURP), including transurethral microwave thermotherapy, transurethral needle ablation of the prostate, and laser prostatectomy.
Laser prostatectomy has the advantage of involving relatively less bleeding, as well as preventing transurethral resection (TUR) syndrome and capsule perforation during the procedure [45]. The most representative lasers currently in use are holmium:yttrium-aluminium-garnet (Ho: YAG), thulium:YAG (Tm:TAG), kalium-titanyl-phosphate (KTP), and semiconductor diodes (SCD). Photoselective vaporization of the prostate (PVP) using KTP or SCD lasers is one of the most popular laser-based surgical procedures performed to treat BPH, and leads to the immediate removal of prostatic tissue, relief of BPO, and reduction of LUTS. PVP is considered to be a safe and effective procedure and requires a relatively short training period [67].
As PVP has emerged as an alternative to MTURP in the treatment of BPH, several valuable randomized controlled trials (RCTs) have compared the surgical efficacy and safety of MTURP and PVP [7891011121314151617]. Thus, we performed a systematic review and meta-analysis of these RCTs in order to compare MTURP and PVP and to be able to provide the most up-to-date and reliable recommendations possible.
RCTs that met the following criteria were included: (1) a study design including a comparison of functional outcomes and complications between PVP and MTURP in men treated for BPH; (2) the inclusion of accurate perioperative variables, including operative time, catheterization time, and hospitalization time, as well as complication-related variables, including transfusion rate as well as rates of acute urinary retention, clot retention, and urinary tract infection; (3) evaluation of long-term functional outcomes, including the International Prostate Symptom Score (IPSS) and the maximum flow rate (Qmax) parameter; and (4) accessible full text of the study or abstract presented at a scientific conference.
A literature search was performed for all publications prior to December 31, 2015 in the PubMed and EMBASE™ online databases. A cross-reference search of eligible articles was carried out in order to identify additional studies not found by the computerized search. The following MeSH terms and keywords were used: prostatic hyperplasia, TUR of prostate, photoselective vaporization, TUR, prostate, BPH, and RCT.
One researcher (D.H.K.) screened the titles and abstracts that were identified using this search strategy. The other two researchers (J.Y.L. and K.S.C.) independently assessed the full text of the papers to determine whether they met the inclusion criteria. The data entry procedure was designed to ensure the inclusion of the most relevant data, such as the author, year of publication, patient demographics, treatments, fertility rates, and the inclusion of a reference standard. Disagreements were resolved by discussion until a consensus was reached or by arbitration involving another researcher (Y.D.C.).
Once the final group of articles was agreed upon, two researchers (J.Y.L. and D.H.K.) independently assessed the quality of each article using the Cochrane risk of bias as a quality assessment tool for RCTs. This process involved assigning a judgment of "yes," "no," or "unclear" for each domain in order to designate a low, high, or unclear risk of bias, respectively. If one domain or no domain was deemed "unclear" or "no," the study was classified as having a low risk of bias. If four or more domains were deemed "unclear" or "no," the study was classified as having a high risk of bias. If two or three domains were deemed "unclear" or "no," the study was classified as having a moderate risk of bias [18]. Publication bias was examined using funnel plots and statistical results from the Begg and Mazumdar rank correlation test [19] and Egger's regression test [20] for funnel plot asymmetry. In the absence of publication bias, this method assumes that the largest studies will be plotted near the average and that smaller studies will be spread evenly on both sides of the average, creating a roughly funnel-shaped distribution. Deviation from this shape can indicate publication bias. Quality assessment and investigation of publication bias were carried out using Review Manager 5 (RevMan 5.2.3; Cochrane Collaboration, Oxford, UK) and R (R version 3.0.3; R Foundation for Statistical Computing, Vienna, Austria; http://www.r-project.org), with its metafor package.
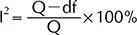
Heterogeneity among studies was evaluated using the Q statistic and Higgins' I2 statistic [21]. Higgins' I2 is used to measure a set of studies to identify the percentage of total variation due to heterogeneity rather than chance. Higgins' I2 is calculated as follows: where Q is Cochran's heterogeneity statistic and df refers to the degrees of freedom.
An I2 greater than 50% is considered to represent substantial heterogeneity. For the Q statistic, heterogeneity was deemed to be significant if the p-value was <0.10 [22]. When evidence of heterogeneity was found, the data were analyzed using a random-effects model to obtain a summary estimate for the test sensitivity along with 95% confidence intervals (CIs). Studies in which positive results were confirmed were analyzed using pooled specificity with 95% CIs. In addition, Galbraith's radial plots [23] were performed to evaluate heterogeneity.
When a significant Q-test indicated heterogeneity across studies (p<0.10 or I2>50%), a random-effects model was used for the meta-analysis; otherwise, a fixed-effects model was employed [24]. The meta-analysis of comparable data was carried out using Review Manager 5.3 and R, using its meta and metafor packages.
Our database search found 40 articles that could have potentially been included in the meta-analysis. Based on the inclusion and exclusion criteria, 11 articles were excluded after a simple reading of the titles and abstracts of the articles, and two articles were excluded due to the patient population. Ultimately, 11 articles were included in the analysis of PVP versus MTURP (Fig. 1) [7891011121314151617]. The studies that were included are summarized in Table 1.
Fig. 2 presents the details of quality assessment, as measured by the Cochrane Collaboration risk-of-bias tool. Two trials exhibited a moderate risk of bias for all quality criteria, while the others were classified as having a low risk of bias (Table 1). The most common risk factor for quality assessment was the risk of insufficient information concerning allocation concealment, followed by concerns involving random sequence generation. Most recently published studies exhibited a low risk with regard to quality assessment.
The Begg and Mazumdar rank correlation tests [19] in each analysis showed no evidence of publication bias in the present meta-analysis (operation time, p=0.275; catheterization time, p=0.239; hospitalization time, p=0.469; transfusion rate, p=0.283; acute urinary retention, p=0.773; clot retention, p=0.333; urinary tract infection, p=0.399; bladder neck contracture, p=1.000; urethral stricture, p=0.469; IPSS, p=0.719; Qmax, p=1.000). Egger's regression intercept tests [20] revealed that catheterization time exhibited publication bias, whereas all other variables showed no evidence of publication bias (operation time, p=0.351; catheterization time, p<0.001; hospitalization time, p=0.215; transfusion rate, p=0.233; acute urinary retention, p=0.431; clot retention, p=0.555; urinary tract infection, p=0.237; bladder neck contracture, p=0.923; urethral stricture, p=0.584; IPSS, p=0.925; Qmax, p=0.731). Funnel plots from these meta-analyses are shown in Fig. 3.
Forest plots are shown in Fig. 4, 5, 6, 7. A heterogeneity test showed that notable degrees of heterogeneity were detected in the analyses for operation time, catheterization time, and hospitalization time (Fig. 4); thus, random-effects models were used to further assess these variables. However, no significant heterogeneity was found in the other analyses, so fixed-effect models were applied. In Galbraith's radial plots, no variables demonstrated heterogeneity after the selection of effect models for each variable (Fig. 8).
In a meta-analysis of operation time between PVP and MTURP, the forest plot using the random effect model showed a mean difference of 12.89 (95% CI=7.09~18.70, p<0.001), favoring MTURP (Fig. 4A). However, the mean differences for catheterization and hospitalization time were -1.39 (95% CI=-1.83~-0.95, p<0.001) and -2.21 (95% CI=-2.73~-1.69, p<0.001), respectively, favoring PVP (Fig. 4A, 4B). PVP was found to be superior to MTURP with regard to the transfusion rate (odds ratio [OR]=0.17, 95% CI=0.08~0.37, p<0.001) and clot retention (OR=0.10, 95% CI=0.03~0.27, p<0.001) (Fig. 5A, 5C); however, no statistically significant differences were found regarding acute urinary retention and urinary tract infection (Fig. 5B, 5D). The long-term complications of bladder neck contracture and urethral stricture showed no statistically significant differences between PVP and MTURP (Fig. 6). Long-term functional outcomes, including IPSS and Qmax, also demonstrated no statistically significant differences between PVP and MTURP (Fig. 7).
Several meta-analyses comparing PVP and MTURP have already been published [252627]. These meta-analyses have found that MTURP was characterized by a shorter operative time, while PVP showed shorter catheterization and hospitalization times. Bleeding-related complications and TUR syndrome occurred more frequently in MTURP. In terms of voiding efficacy, the effects of the two procedures were similar. The results of the present meta-analysis are not different from those reported in previous studies, but our study does have some advantages compared to previous studies. First, some of those analyses included case-control studies, while our meta-analysis included only RCTs. Second, at least three years have passed since the most recent meta-analysis, and we were able to include additional high-quality RCTs that have been published since. Thus, the present meta-analysis can provide the most up-to-date and reliable recommendations that have yet been published.
As the elderly population has increased, the prevalence of typical age-related male diseases, such as male LUTS secondary to BPH, has increased [28]. The effectiveness of medical treatment for this conditions is relatively high, but patients need to undergo surgery in cases of renal insufficiency secondary to BPH, recurrent urinary tract infections (UTIs), gross hematuria due to BPH or bladder stones, and LUTS refractory to other therapies [29]. MTURP has demonstrated improved long-term efficacy and safety, and has emerged as the gold standard surgery in patients with prostate sizes under 80 mL and moderate-to-severe LUTS secondary to BPO [3]. However, TURP-related morbidities such as TUR syndrome and bleeding still pose considerable challenges. For this reason, alternative procedures have been developed that show similar levels of efficacy but lower complication rates. Laser procedures, such as Holmium laser enucleation of the prostate (HoLEP) and PVP, are the most representative alternatives to MTURP. A meta-analysis by Tan et al [30] found that HoLEP showed a similar voiding efficiency and a lower complication rate than MTURP. In other recent meta-analyses, the IPSS and Qmax scores after one year among patients treated with HoLEP were slightly better than among patients treated with MTURP [3132]. However, HoLEP has the disadvantage of requiring a substantial amount of training due to the technical challenges that it poses, and it can be dangerous for unskilled surgeons to perform this procedure [7]. PVP is also one of the most popular alternative treatments. The main advantage of PVP is that it is technically simpler than HoLEP, with a relatively straight-forward learning curve [67]. However, HoLEP can be safely used to treat larger prostates that would otherwise be treated through open prostatectomy. Although we only compared PVP and MTURP in the present meta-analysis, HoLEP is another promising alternative, and we suggest that meta-analyses comparing MTURP, PVP, and HoLEP are needed in the future.
When analyzing transurethral prostate surgical procedures, voiding parameters should be considered the most important treatment outcomes. In this meta-analysis, no significant differences were found between PVP and MTURB in IPSS and Qmax at one year of follow-up. The long-term data regarding PVP remains insufficient, making it impossible to analyze follow-up results over a period longer than one year. Further studies should be performed to evaluate the long-term efficacy of PVP in terms of voiding parameters.
Regarding perioperative outcomes, the mean operative time was significantly shorter, by approximately 13 minutes, in the MTURP group. Various explanations of this finding may be proposed: the surgeons may not have been experienced with PVP; the laser may not have provided enough energy or power to the prostatic tissue; or the PVP laser energy absorption in water may be minimal, resulting in prolonged operations [33]. However, the mean operative time of PVP can be substantially reduced by improving the surgeon's overall faculties, technical skills, and confidence. Furthermore, recent studies on PVP using lasers with more than 120 W of power (160 W and 180 W) [343536] have been conducted with the goal of reducing the operative time of PVP. In contrast, the catheterization and hospitalization times were significantly shorter in the PVP group. The discharge was especially faster in the subgroup of PVP patients more than two days compared to the subgroup of MTURP patients. The catheterization and hospitalization time are important factors affecting patients' quality of life, so this result indicates a major advantage of PVP.
It is well-known that KTP lasers are strongly absorbed by hemoglobin, resulting in excellent homeostasis [37]. For this reason, bleeding-related complications occurred more frequently in the MTURP group, as well as higher transfusion and clot retention rates. This finding indirectly supports the results of studies evaluating PVP in patients taking anticoagulants [3839]. No significant differences between the groups were found with regard to either early postoperative complications, including acute urinary retention and UTIs, or late complications, including bladder neck contracture and urethral stricture. TUR syndrome does not occur in PVP because saline is used as the fluid medium instead of glycine, and it was therefore impossible to perform a meta-analysis for TUR syndrome. The total TUR syndrome rate in the MTURP group was 1.7% (7/409). Combining all of these results regarding efficacy and safety, it seems reasonable for PVP to be performed as an alternative surgical treatment for treating male LUTS secondary to BPH, although long-term follow-up remains essential in the future.
Most of the studies we analyzed used GreenLight™ lasers (KTP, wavelength 532 nm) for PVP, but SCD lasers were used in one study [17]. The SCD laser uses the wavelength (980 nm) that has the highest absorption for hemoglobin and water, providing both hemostatic and ablative properties [17]. The GreenLight™ laser power was also not uniform (80 W or 120 W) across the studies we analyzed. These discrepancies may theoretically be a source of bias, but do not think that it was significant because this meta-analysis was focused on PVP overall, rather than on laser type or power. As stated above, studies are now evaluating PVP performed with lasers with more than 120 W of power (160 W and 180 W) [343536], but it is too early to present an informed discussion of the efficacy and safety of high-energy PVP. These issues must be addressed in future comparative studies.
One limitation of our meta-analysis is that we did not assess sexual complications, such as erectile dysfunction and ejaculatory disorders. So far, an insufficient number of RCTs have evaluated sexual complications. Additionally, our study was also susceptible to some degree of publication bias. However, Sutton et al [40] reviewed 48 articles from the Cochrane Database of Systematic Reviews and showed that publication bias and related biases were common within their sample of meta-analyses, and found that these biases did not affect the conclusions in most cases. Despite these limitations, our study is a valuable meta-analysis because it spans studies performed over a longer period than previous analyses and provides more up-to-date and reliable evidence.
In our meta-analysis of functional outcomes and complications following PVP and MTURP, voiding efficiency at one year of follow-up was similar between these two procedures. The operative time was significantly shorter for MTURP, while the catheterization and hospitalization times were significantly shorter for PVP. Bleeding-related complications occurred more frequently in MTURP. Based on these findings, we believe that PVP can be performed as an alternative surgical procedure for treating male LUTS secondary to BPH.
References
1. Martin SA, Haren MT, Marshall VR, Lange K, Wittert GA. Prevalence and factors associated with uncomplicated storage and voiding lower urinary tract symptoms in community-dwelling Australian men. World J Urol. 2011; 29:179–184. PMID: 20963421.

2. Chapple CR. Lower urinary tract symptoms suggestive of benign prostatic obstruction--triumph: design and implementation. Eur Urol. 2001; 39(Suppl 3):31–36. PMID: 11275740.
3. Oelke M, Bachmann A, Descazeaud A, Emberton M, Gravas S, Michel MC, et al. EAU guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol. 2013; 64:118–140. PMID: 23541338.

4. Malek RS, Kuntzman RS, Barrett DM. Photoselective potassium-titanyl-phosphate laser vaporization of the benign obstructive prostate: observations on long-term outcomes. J Urol. 2005; 174:1344–1348. PMID: 16145416.

5. Lee R, Gonzalez RR, Te AE. The evolution of photoselective vaporization prostatectomy (PVP): advancing the surgical treatment of benign prostatic hyperplasia. World J Urol. 2006; 24:405–409. PMID: 16699795.

6. Bachmann A, Ruszat R, Wyler S, Reich O, Seifert HH, Müller A, et al. Photoselective vaporization of the prostate: the basel experience after 108 procedures. Eur Urol. 2005; 47:798–804. PMID: 15925076.

7. Bouchier-Hayes DM, Van Appledorn S, Bugeja P, Crowe H, Challacombe B, Costello AJ. A randomized trial of photoselective vaporization of the prostate using the 80-W potassium-titanyl-phosphate laser vs transurethral prostatectomy, with a 1-year follow-up. BJU Int. 2010; 105:964–969. PMID: 19912196.

8. Horasanli K, Silay MS, Altay B, Tanriverdi O, Sarica K, Miroglu C. Photoselective potassium titanyl phosphate (KTP) laser vaporization versus transurethral resection of the prostate for prostates larger than 70 mL: a short-term prospective randomized trial. Urology. 2008; 71:247–251. PMID: 18308094.

9. Al-Ansari A, Younes N, Sampige VP, Al-Rumaihi K, Ghafouri A, Gul T, et al. GreenLight HPS 120-W laser vaporization versus transurethral resection of the prostate for treatment of benign prostatic hyperplasia: a randomized clinical trial with midterm follow-up. Eur Urol. 2010; 58:349–355. PMID: 20605316.

10. Capitán C, Blázquez C, Martin MD, Hernández V, de la Peña E, Llorente C. GreenLight HPS 120-W laser vaporization versus transurethral resection of the prostate for the treatment of lower urinary tract symptoms due to benign prostatic hyperplasia: a randomized clinical trial with 2-year follow-up. Eur Urol. 2011; 60:734–739. PMID: 21658839.

11. Lukacs B, Loeffler J, Bruyère F, Blanchet P, Gelet A, Coloby P, et al. Photoselective vaporization of the prostate with GreenLight 120-W laser compared with monopolar transurethral resection of the prostate: a multicenter randomized controlled trial. Eur Urol. 2012; 61:1165–1173. PMID: 22341632.

12. Mohanty NK, Vasudeva P, Kumar A, Prakash S, Jain M, Arora RP. Photoselective vaporization of prostate vs. transurethral resection of prostate: a prospective, randomized study with one year follow-up. Indian J Urol. 2012; 28:307–312. PMID: 23204660.

13. Pereira-Correia JA, de Moraes Sousa KD, Santos JB, de Morais Perpétuo D, Lopes-da-Silva LF, Krambeck RL, et al. GreenLight HPS™ 120-W laser vaporization vs transurethral resection of the prostate (<60 mL): a 2-year randomized double-blind prospective urodynamic investigation. BJU Int. 2012; 110:1184–1189. PMID: 22257240.
14. Kumar A, Vasudeva P, Kumar N, Nanda B, Jha SK, Mohanty N. A prospective randomized comparative study of monopolar and bipolar transurethral resection of the prostate and photoselective vaporization of the prostate in patients who present with benign prostatic obstruction: a single center experience. J Endourol. 2013; 27:1245–1253. PMID: 23746047.

15. Xue B, Zang Y, Zhang Y, Yang D, Gao J, Sun C, et al. GreenLight HPS 120-W laser vaporization versus transurethral resection of the prostate for treatment of benign prostatic hyperplasia: a prospective randomized trial. J Xray Sci Technol. 2013; 21:125–132. PMID: 23507858.

16. Telli O, Okutucu TM, Suer E, Burgu B, Gulpinar O, Yaman O, et al. A prospective, randomized comparative study of monopolar transurethral resection of the prostate versus photoselective vaporization of the prostate with GreenLight 120-W laser, in prostates less than 80 cc. Ther Adv Urol. 2015; 7:3–8. PMID: 25642290.
17. Cetinkaya M, Onem K, Rifaioglu MM, Yalcin V. 980-Nm diode laser vaporization versus transurethral resection of the prostate for benign prostatic hyperplasia: randomized controlled study. Urol J. 2015; 12:2355–2361. PMID: 26571321.
18. Chung JH, Lee SW. Assessing the quality of randomized controlled urological trials conducted by Korean medical institutions. Korean J Urol. 2013; 54:289–296. PMID: 23700493.

19. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994; 50:1088–1101. PMID: 7786990.

20. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997; 315:629–634. PMID: 9310563.

21. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003; 327:557–560. PMID: 12958120.

22. Fleiss JL. Analysis of data from multiclinic trials. Control Clin Trials. 1986; 7:267–275. PMID: 3802849.

23. Galbraith RF. A note on graphical presentation of estimated odds ratios from several clinical trials. Stat Med. 1988; 7:889–894. PMID: 3413368.

24. DerSimonian R, Kacker R. Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials. 2007; 28:105–114. PMID: 16807131.

25. Teng J, Zhang D, Li Y, Yin L, Wang K, Cui X, et al. Photoselective vaporization with the green light laser vs transurethral resection of the prostate for treating benign prostate hyperplasia: a systematic review and meta-analysis. BJU Int. 2013; 111:312–323. PMID: 23145474.

26. Ding H, Du W, Lu ZP, Zhai ZX, Wang HZ, Wang ZP. Photoselective green-light laser vaporisation vs. TURP for BPH: meta-analysis. Asian J Androl. 2012; 14:720–725. PMID: 22902908.

27. Thangasamy IA, Chalasani V, Bachmann A, Woo HH. Photoselective vaporisation of the prostate using 80-W and 120-W laser versus transurethral resection of the prostate for benign prostatic hyperplasia: a systematic review with meta-analysis from 2002 to 2012. Eur Urol. 2012; 62:315–323. PMID: 22575913.

28. Berry SJ, Coffey DS, Walsh PC, Ewing LL. The development of human benign prostatic hyperplasia with age. J Urol. 1984; 132:474–479. PMID: 6206240.

29. McVary KT, Roehrborn CG, Avins AL, Barry MJ, Bruskewitz RC, Donnell RF, et al. Update on AUA guideline on the management of benign prostatic hyperplasia. J Urol. 2011; 185:1793–1803. PMID: 21420124.

30. Tan A, Liao C, Mo Z, Cao Y. Meta-analysis of holmium laser enucleation versus transurethral resection of the prostate for symptomatic prostatic obstruction. Br J Surg. 2007; 94:1201–1208. PMID: 17729384.

31. Yin L, Teng J, Huang CJ, Zhang X, Xu D. Holmium laser enucleation of the prostate versus transurethral resection of the prostate: a systematic review and meta-analysis of randomized controlled trials. J Endourol. 2013; 27:604–611. PMID: 23167266.

32. Li S, Zeng XT, Ruan XL, Weng H, Liu TZ, Wang X, et al. Holmium laser enucleation versus transurethral resection in patients with benign prostate hyperplasia: an updated systematic review with meta-analysis and trial sequential analysis. PLoS One. 2014; 9:e101615. PMID: 25003963.

33. Wendt-Nordahl G, Huckele S, Honeck P, Alken P, Knoll T, Michel MS, et al. 980-nm diode laser: a novel laser technology for vaporization of the prostate. Eur Urol. 2007; 52:1723–1728. PMID: 17611013.

34. Chen J, Wang M, Wang S, Sun P, Zhao Y, Zhang L, et al. 160-Watt lithium triboride laser vaporization versus transurethral resection of prostate: a prospective nonrandomized two-center trial. Urology. 2012; 79:650–654. PMID: 22386419.

35. Ouyang Y, Liu C, Guan W, Zhao Y, Xu Y, Wu Y. Impact of 160 W Greenlight laser vaporization of the prostate on erectile function: a prospective randomized controlled trial with 1-year follow-up. Photomed Laser Surg. 2014; 32:463–467. PMID: 25101536.

36. Castellan P, Castellucci R, Schips L, Cindolo L. Safety, efficacy and reliability of 180-W GreenLight laser technology for prostate vaporization: review of the literature. World J Urol. 2015; 33:599–607. PMID: 25647174.

37. Reich O, Bachmann A, Schneede P, Zaak D, Sulser T, Hofstetter A. Experimental comparison of high power (80 W) potassium titanyl phosphate laser vaporization and transurethral resection of the prostate. J Urol. 2004; 171:2502–2504. PMID: 15126885.

38. Choi YS, Bae WJ, Kim SJ, Kim KS, Cho HJ, Hong SH, et al. Efficacy and safety of 120-W GreenLight High-Performance System laser photo vaporization of the prostate: 3-year results with specific considerations. Prostate Int. 2013; 1:169–176. PMID: 24392442.

39. Sandhu JS, Ng CK, Gonzalez RR, Kaplan SA, Te AE. Photoselective laser vaporization prostatectomy in men receiving anticoagulants. J Endourol. 2005; 19:1196–1198. PMID: 16359214.

40. Sutton AJ, Duval SJ, Tweedie RL, Abrams KR, Jones DR. Empirical assessment of effect of publication bias on meta-analyses. BMJ. 2000; 320:1574–1577. PMID: 10845965.

Fig. 1
Flow diagram of screened, excluded, and analyzed publications. Based on the inclusion and exclusion criteria, 11 articles were excluded after a simple reading of the titles and abstracts of the articles, and two articles were excluded due to the patient population.
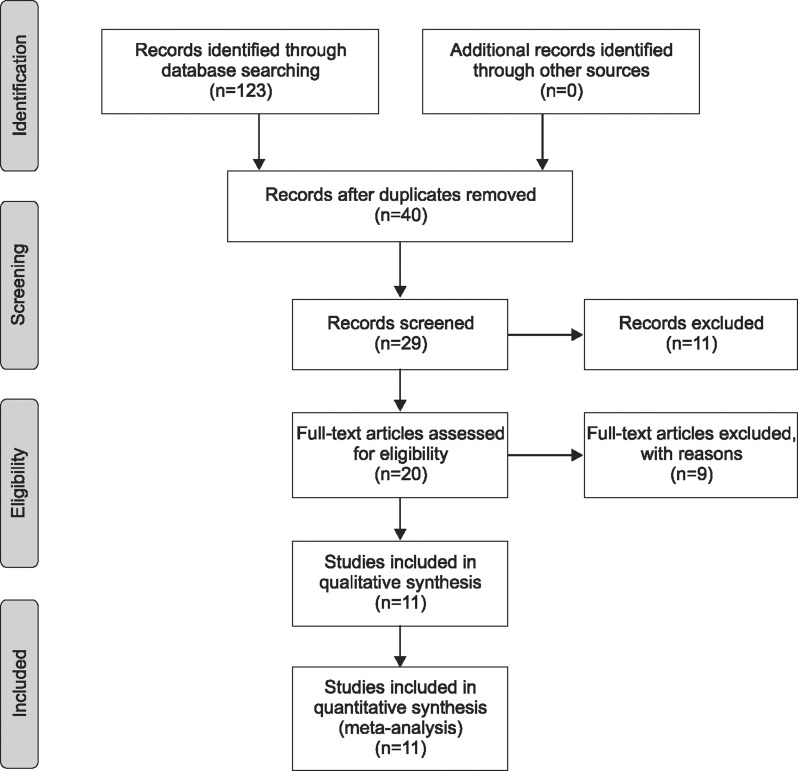
Fig. 2
Methodological quality graph. Two researchers' judgments about each methodological quality item are presented as percentages across all included studies. Two trials exhibited a moderate risk of bias for all quality criteria and all others were classified as having a low risk of bias.
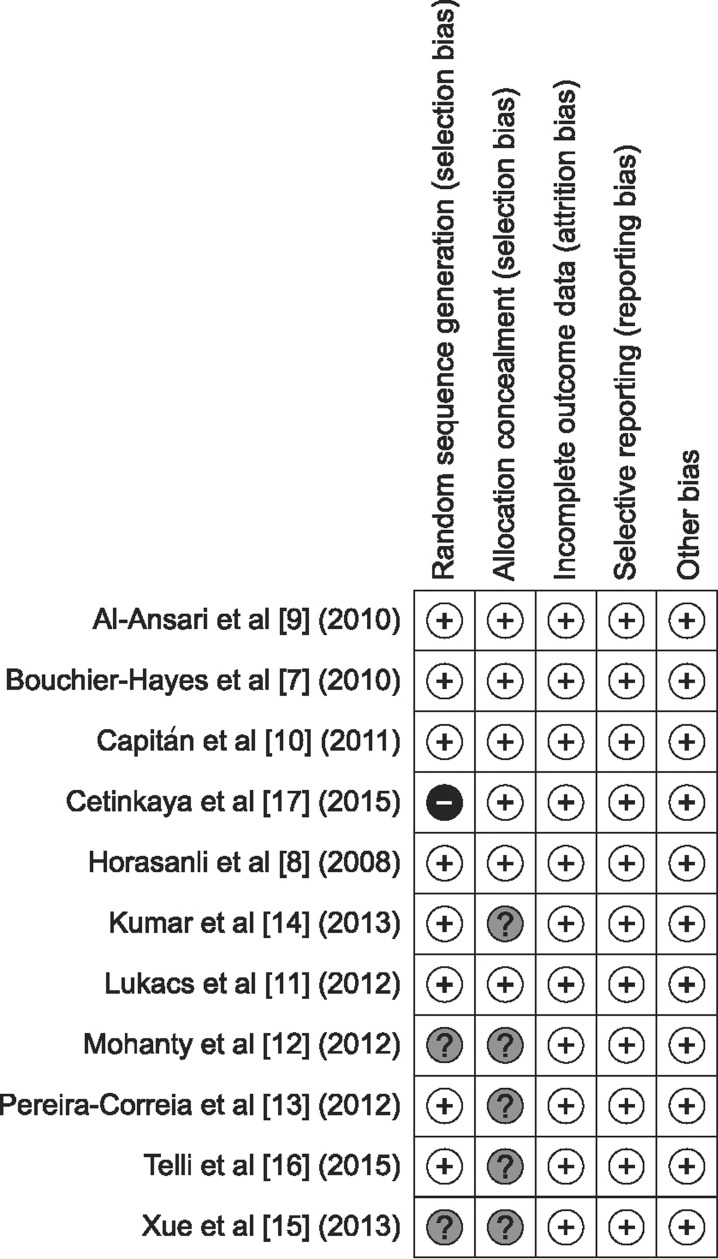
Fig. 3
Funnel plots. Egger's regression intercept tests demonstrated that catheterization time showed evidence of publication bias (p<0.001), whereas the other variables had no evidence of publication bias. (A) Operation time. (B) Hospitalization time. (C) Catheterization time. (D) Transfusion rate. (E) Acute urinary retention. (F) Clot retention. (G) Urinary tract infection. (H) Bladder neck contracture. (I) Urethral stricture. (J) International Prostate Symptom Score. (K) Maximum flow rate. SE: standard error, MD: mean difference, OR: odds ratio.
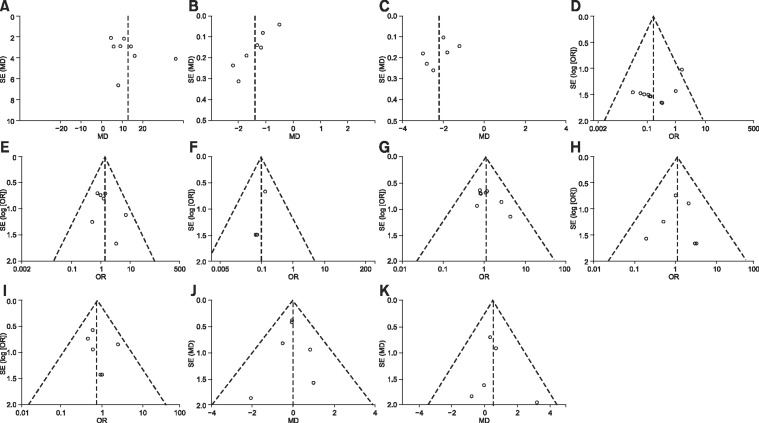
Fig. 4
Forest plots comparing operation time (A), catheterization time (B), and hospitalization time between PVP and MTURP (C). With regard to operative time, the forest plot using the random effect model showed a MD of 12.89 (95% CI=7.09~18.70, p<0.001) in favor of MTURP. However, the MDs for catheterization and hospitalization time were -1.39 (95% CI=-1.83~-0.95, p<0.001) and -2.21 (95% CI=-2.73~-1.69, p<0.001), respectively, in favor of PVP. PVP: photoselective vaporization of the prostate, MTURP: monopolar transurethral resection of the prostate, SD: standard deviation, CI: confidence interval, MD: mean difference, W: weight.
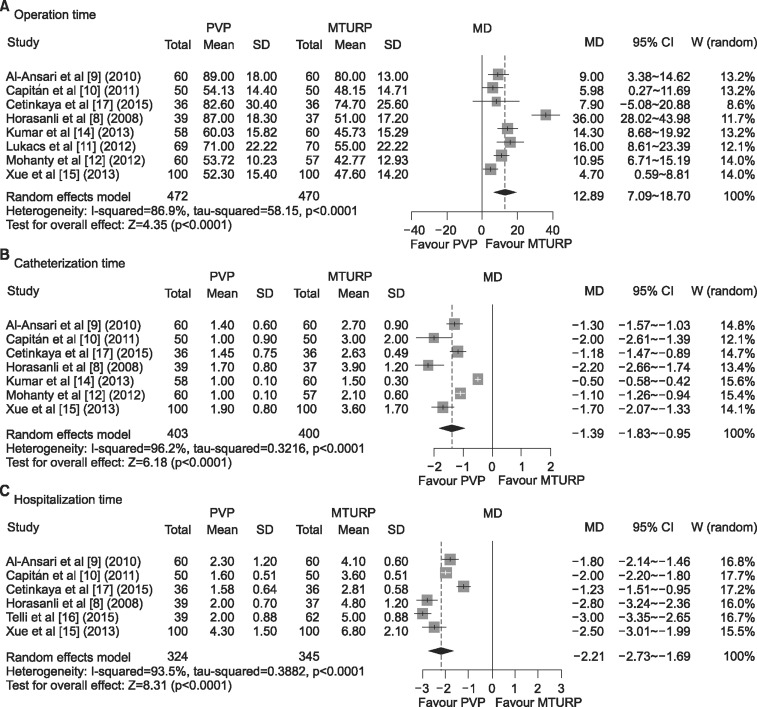
Fig. 5
Forest plots of transfusion rates (A), acute urinary retention (B), clot retention (C), and urinary tract infection comparing PVP and MTURP (D). Superior results were found for PVP regarding transfusion rates (OR=0.17, 95% CI=0.08~0.37, p<0.001) and clot retention (OR=0.10, 95% CI=0.03~0.27, p<0.001), but no statistically significant differences were found for acute urinary retention and urinary tract infection. PVP: photoselective vaporization of the prostate, MTURP: monopolar transurethral resection of the prostate, OR: odds ratio, CI: confidence interval, W: weight.
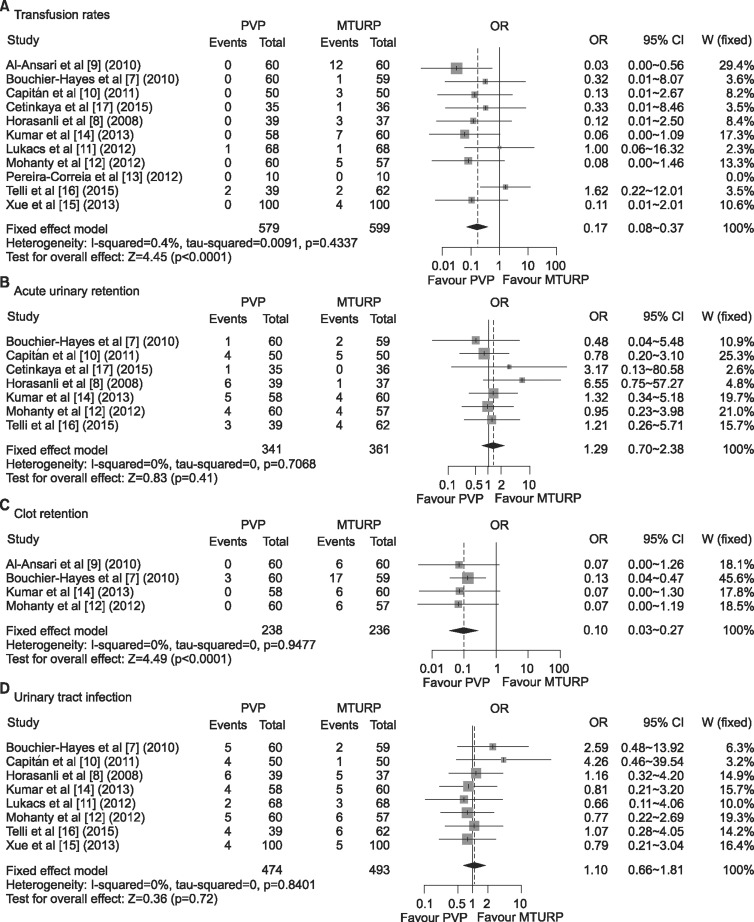
Fig. 6
Forest plots comparing bladder neck contracture (A) and urethral stricture between PVP and MTURP (B). No statistically significant differences were found. PVP: photoselective vaporization of the prostate, MTURP: monopolar transurethral resection of the prostate, OR: odds ratio, CI: confidence interval, W: weight.
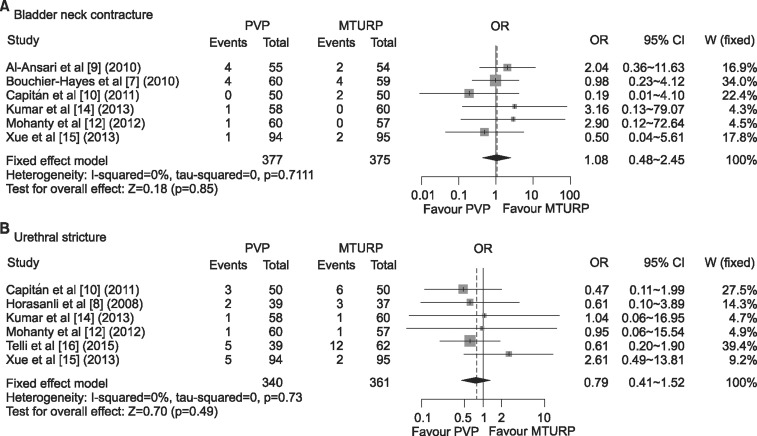
Fig. 7
Forest plots comparing long-term functional outcomes, including IPSS (A) and Qmax (B). No differences were found between PVP and MTURP. IPSS: International Prostate Symptom Score, PVP: photoselective vaporization of the prostate, MTURP: monopolar transurethral resection of the prostate, SD: standard deviation, MD: mean difference, CI: confidence interval, W: weight, Qmax: maximum flow rate.
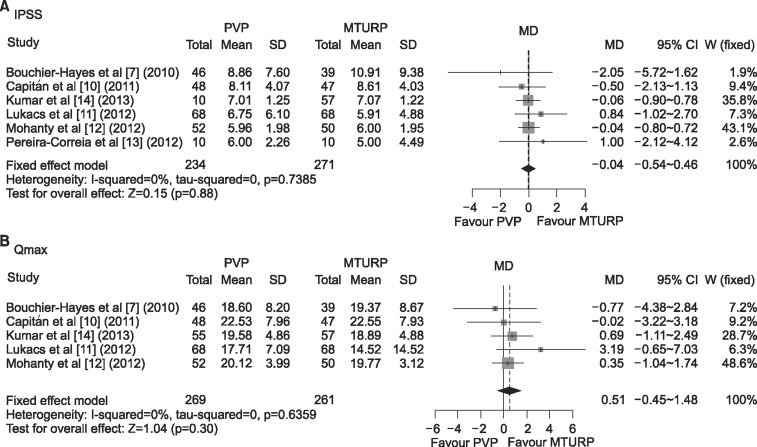
Fig. 8
Galbraith's radial plots. Most variables demonstrated little heterogeneity after selecting the effect models for each variable. (A) Operation time. (B) Hospitalization time. (C) Catheterization time. (D) Transfusion rate. (E) Acute urinary retention. (F) Clot retention. (G) Urinary tract infection. (H) Bladder neck contracture. (I) Urethral stricture. (J) International Prostate Symptom Score. (K) Maximum flow rate.
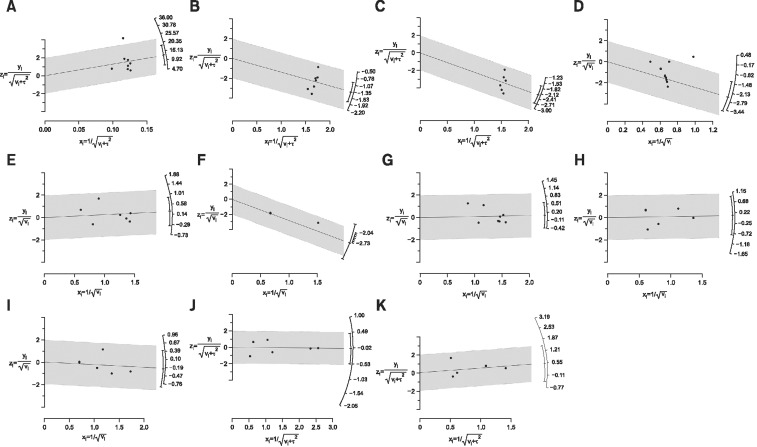
Table 1
Studies included in this meta-analysis
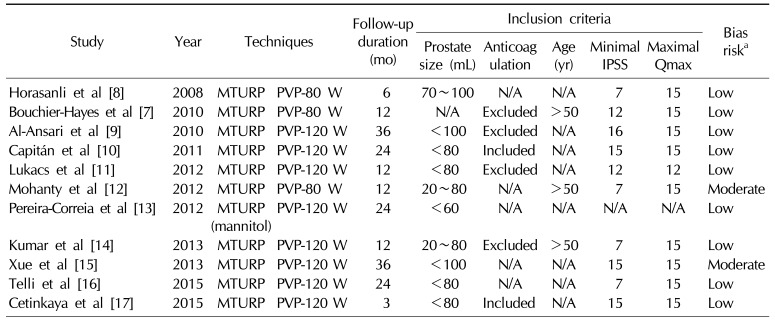
| Study | Year | Techniques | Follow-up duration (mo) | Inclusion criteria | Bias riska | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Prostate size (mL) | Anticoag ulation | Age (yr) | Minimal IPSS | Maximal Qmax | ||||||
| Horasanli et al [8] | 2008 | MTURP | PVP-80 W | 6 | 70~100 | N/A | N/A | 7 | 15 | Low |
| Bouchier-Hayes et al [7] | 2010 | MTURP | PVP-80 W | 12 | N/A | Excluded | >50 | 12 | 15 | Low |
| Al-Ansari et al [9] | 2010 | MTURP | PVP-120 W | 36 | <100 | Excluded | N/A | 16 | 15 | Low |
| Capitán et al [10] | 2011 | MTURP | PVP-120 W | 24 | <80 | Included | N/A | 15 | 15 | Low |
| Lukacs et al [11] | 2012 | MTURP | PVP-120 W | 12 | <80 | Excluded | N/A | 12 | 12 | Low |
| Mohanty et al [12] | 2012 | MTURP | PVP-80 W | 12 | 20~80 | N/A | >50 | 7 | 15 | Moderate |
| Pereira-Correia et al [13] | 2012 | MTURP (mannitol) | PVP-120 W | 24 | <60 | N/A | N/A | N/A | N/A | Low |
| Kumar et al [14] | 2013 | MTURP | PVP-120 W | 12 | 20~80 | Excluded | >50 | 7 | 15 | Low |
| Xue et al [15] | 2013 | MTURP | PVP-120 W | 36 | <100 | N/A | N/A | 15 | 15 | Moderate |
| Telli et al [16] | 2015 | MTURP | PVP-120 W | 24 | <80 | N/A | N/A | 7 | 15 | Low |
| Cetinkaya et al [17] | 2015 | MTURP | PVP-120 W | 3 | <80 | Included | N/A | 15 | 15 | Low |
IPSS: International Prostate Symptom Score, Qmax: maximum flow rate, MTURP: monopolar transurethral resection of the prostate, PVP: photoselective vaporization of the prostate, N/A: not available.
aQuality assessment was based on using Cochrane's risk of bias as a quality assessment tool for randomized controlled trials. If four or more domains were deemed "unclear" or "no," the study was classified as having a high risk of bias. If two or three domains were deemed "unclear" or "no," the study was classified as having a moderate risk of bias.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download