Abstract
Purpose
This study evaluated the demographics and semen parameters of males with cancer who banked their sperm prior to chemotherapy.
Materials and Methods
This is a retrospective study of 66 cases referred for sperm banking prior to initiation of chemotherapy over a 15-year period (1999~2014). Patients who had previously received cancer treatment including chemotherapy or radiotherapy were not included in this study.
Results
We studied a total of 66 cancer patients referred for cryopreservation of sperm prior to chemotherapy. The mean age of the patients at the time of banking was 32.0±7.9 years (range, 19~58 years). The types of cancer were testicular cancer (31 cases, 47.0%), non-Hodgkin's disease (10 cases, 15.1%), Hodgkin's disease (5 cases, 7.6%), leukemia (8 cases, 12.1%), gastrointestinal malignancy (5 cases, 7.6%), and musculoskeletal malignancy (5 cases, 7.6%). There were significant differences in sperm concentration and viability among the various types of cancer, but no significant difference in semen volume or sperm motility and morphology.
As survival rates and life expectancy following treatment for cancer increase, quality-of-life (QoL) issues have drawn more attention. Fertility is one of the main QoL concerns for cancer survivors of reproductive age, and its loss, or the possibility of its loss, can be an important factor in the psychological morbidity of survivors [1]. The significance of preservation of future parenthood at the time of a cancer diagnosis is widely recognized; consequently, the role of sperm banking is expected to increase [2]. It is well known that some forms of cancer treatment, such as chemotherapy, can cause azoospermia or reduced spermatogenesis [3]. However, the types of cancer that can themselves harm semen quality are unclear. Some studies have found no difference in the quality of sperm between individuals with cancer and those without. By contrast, other studies have reported significant reductions in sperm quality in some malignancies, such as testicular cancer and Hodgkin's lymphoma [4,5]. Although cryopreservation is accepted as a safe and useful method of preserving fertility potential in male cancer patients regardless of semen quality [6], fertility and reproductive function remain the major concerns for 80% of males that have successfully recovered from cancer [7]. The aim of this study was to evaluate the clinical characteristics and semen parameters of patients with cancer who were referred for sperm banking prior to chemotherapy.
This was a retrospective study of 66 cases referred for sperm banking prior to initiation of chemotherapy over a 15-year period. Approval for this study was obtained from the Institutional Review Board of Pusan National University Hospital. Data collected were anonymized, and the principles of the Declaration of Helsinki were followed. We reviewed data from cancer patients who banked their sperm samples for fertility preservation at the Pusan National University Hospital sperm bank between 1999 and 2014. Patients who had previously received cancer therapy, including chemotherapy or radiotherapy, were excluded from the study.
Semen samples were collected by masturbation. An experienced technician performed computer-aided semen analysis for sperm concentration and motility. Sperm viability was analyzed with nigrosin-eosin staining and Kruger/strict morphology, employing methodologies of the World Health Organization (WHO, 4th edition) [8].
A freezing solution was added to sperm specimens in a 3 : 1 ratio. After 10 minutes, the solution was divided among straws for storage. The 1-mL straws were suspended in liquid nitrogen vapor (5 cm above the level of liquid nitrogen at -80℃ to -100℃) for 15 minutes. The samples were then immersed in liquid nitrogen (-196℃) for longer storage.
Statistical analyses were performed using the PASW software version 18.00 (IBM Co., Armonk, NY, USA). Data are expressed as mean±standard deviation. Analysis of variance (ANOVA) and Kruskal-Wallis tests were used for multiple group comparisons. p values <0.05 were considered to indicate statistical significance.
A total of 66 cancer patients who registered for cryopreservation of their sperm samples prior to chemotherapy were included in this study. The mean age of the patients at the time of banking was 32.0±7.9 years (range, 19~58 years). Forty-eight patients (72.7%) were single and eighteen (27.3%) were married. The mean interval between cancer diagnosis and referral to the sperm bank was 4 months (1~18 months). The types of cancer were testicular cancer (31 cases, 47.0%), non-Hodgkin's disease (10 cases, 15.1%), Hodgkin's disease (5 cases, 7.6%), leukemia (8 cases, 12.1%), gastrointestinal malignancy (5 cases, 7.6%), and musculoskeletal malignancy (5 cases, 7.6%). Patients with testicular cancer or hematological malignancy comprised the largest groups (Table 1).
There was no significant difference in age among the groups (p=0.747). Upon physical examination, three patients (4.5%) were found to have testicular atrophy (testis volume less than 12 mL). The pathology of testicular cancer was seminoma in 13 patients (41.9%), nonseminoma in 12 patients (36.4%), and unknown in the others (21.7%). Table 2 shows semen parameters across patients and for separate cancer groups. There were significant differences in sperm concentration and viability among the various types of cancer, but semen volume, as well as sperm motility and morphology showed no significant differences. The results of ANOVA with the least significant difference test post hoc indicated significant differences in semen concentration between testicular cancer and non-Hodgkin's disease (p=0.019), testicular cancer and musculoskeletal malignancy (p=0.025), and testicular cancer and gastrointestinal malignancy (p=0.057). These same tests also showed significant differences in sperm viability between testicular cancer and musculoskeletal malignancy (p=0.003), as well as non-Hodgkin's disease and gastrointestinal malignancy (p=0.011).
Although survival rates for most cancers continue to improve, physical and psychological after-effects of cancer remain of concern [5]. In a significant portion of cancer patients, fertility may already be damaged by the cancer itself, and further compromised by the chemotoxic agents of treatment, resulting in temporary or permanent infertility. The first report describing chemotherapy-induced azoospermia was published in 1948 [9]. Since drugs used to treat cancer directly damage proliferating cells, sperm cells in early differentiation are extremely sensitive to these agents. However, even the relatively quiescent sperm precursors can be damaged by the cumulative effects of multiple doses of chemotherapy [10]. The time for recovery of spermatogenesis is thought to be dose-dependent and, consequently, difficult to predict. It has been reported that, while male cancer patients receiving low doses of cytostatic agents may expect recovery of spermatogenesis around 12 weeks following chemotherapy, permanent azoospermia occurs in more than 50% of patients receiving high doses [11].
Alkylating agents including cisplatin and cyclophosphamide pose a high risk of azoospermia, particularly when coupled with ifosfamide, and the risk of permanent azoospermia seems to be dose- and agent-dependent [5]. These alkylating agents have been implicated in damaging germinal epithelial cells, thereby causing infertility [12].
We have summarized the clinical characteristics obtained from published studies on sperm banking before cancer treatment (Table 3) [13,14,15,16,17,18,19,20,21,22,23]. The diversity of malignancies observed in the present study, and the finding that testicular cancer and Hodgkin's disease comprised the largest groups, is comparable with previous studies.
In terms of semen parameters, we found significant differences in sperm concentration and viability among types of cancer, whereas semen volume and sperm motility and morphology showed no significant differences. In contrast, Keene et al's study [13] cited sperm motility to be lowest in Hodgkin's lymphoma, at only 20.0%. Similarly, there is discord between studies concerning semen parameters and cancer type (Table 3). In our study, sperm motility was 30.2% across all patients and lowest in those with non-Hodgkin's lymphoma (28.4%±19.4%) and leukemia (28.7%±15.4%). Amirjannati et al's study [14] showed that semen volume and sperm concentration were significantly different according to type of cancer. In the study by Bizet et al [15], the azoospermia rate was significantly higher in testicular cancer and non-Hodgkin's lymphoma than in Hodgkin's lymphoma. Further study is required to clarify the effects of cancer on semen parameters.
The literature suggests that lack of adequate knowledge about sperm banking, the perceived high cost, and lack of convenient facilities may create negative attitudes toward sperm banking [24]. This may be true for patients but, surprisingly, the situation is similar for oncologists who tend to overestimate the costs of sperm banking and the number of samples needed to make cryopreservation worthwhile.
Over the years, treatment regimens have been modified in an effort to protect gonadal function. Testicular shielding is used when testes do not need to be in the field of radiation, and reduced doses of alkylating agents are employed in an attempt to decrease gonadotoxicity. Nevertheless, the single greatest method of preserving fertility is sperm banking prior to initiation of therapy. In line with this, males have been encouraged to sperm bank [25].
To our knowledge, this is the first study to evaluate sperm cryopreservation before cancer treatment in Korea. Although there are no studies concerning the current local state of sperm banking, especially for patients with cancer, there have been studies in other countries. Sperm banking before cancer treatment is an effective method of fertility preservation endorsed by professional societies in the United States [26]. Nevertheless, surveys in the United Kingdom [2], Australia and New Zealand [27], Canada [28], and the United States [29] reveal that many patients do not receive adequate and timely information regarding sperm banking.
Although this is the first report of sperm banking in patients with cancer before cancer treatment, several limitations of this study should be noted. First, this study had a long-term period of 15 years. However, it was conducted in a single institution, and consequently does not cover the whole of Korea. Second, this was not a prospective study. Third, only patients with chemotherapy were included; patients with radiotherapy or surgery were excluded. Finally, the number of patients was considered to be low.
In this study we found that sperm quality could fall even before chemotherapy. Because chemotherapy can also negatively affect spermatogenesis, sperm cryopreservation prior to treatment should be strongly recommended for cancer patients of reproductive age. We suggest that cryopreservation of semen is the easiest, safest, and most accessible method of safeguarding fertility in male patients facing cancer treatment.
Figures and Tables
Table 1
Clinical characteristics of the patients referred for sperm cryopreservation
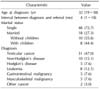
Table 2
Semen parameters according to type of cancer

Table 3
Comparison of prior work and the present study

| Author (year) | No. of patient | Mean age (yr) | Study period (year) | Cancer type (%) | Semen parameters according to type of cancer | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Chung et al (2013) [16] |
130 | 27.0 | 1995~2012 | Testicular cancer (51) | Hematological malignancy (non-Hodgkin's and Hodgkin's (22) | Gastrointestinal (7) | Musculoskeletal (7) | Neurological (4) | Nasopharyngeal (4) | Other (6) | - | - | NA |
|
Keene et al (2012) [13] |
180 | 16.1 | 1995~2009 | Acute leukemia (21) | Hodgkin's lymphoma (21) | Non-Hodgkin's lymphoma (14) | Malignant bone tumor (10) | Testicular cancer (7) | Soft tissue sarcoma (7) | Brain tumor (3) | Teratoma/germ cell tumor (3) | Other (6) | Sperm concentration, motility |
|
Bizet et al (2012) [15] |
1,007 | 29.3 | 1995~2009 | Testicular cancer (41) | Lymphoma (26) | Other hematological cancer (9.4) | Other (22.5) | - | - | - | - | - | Semen volume, sperm concentration, total count, motility |
|
Amirjannati et al (2011) [14] |
73 | 26.0 | 2005~2009 | Testis (59) | Hodgkin's (15) | Lymphoma (7) | Other (19) | - | - | - | - | - | Semen volume, sperm concentration |
|
Hagenäs et al (2010) [17] |
80 | 16.2 | 1995~2009 | Leukemia/non-Hodgkin's lymphoma (31), Hodgkin's (23.7), testis (20), solid tumor (25) | Other (7.5) | - | - | - | - | - | - | - | NA |
|
Ping et al (2010) [18] |
30 | NA (18~37) | 2003~2008 | Testis (70) | Hodgkin's (10) | Digestive system (3.3) | Nasopharyngeal (6.6) | Brain (6.6) | Bone (3.3) | - | - | - | NA |
|
Said et al (2009) [19] |
89 |
30.7 (testis), 29.0 (systemic malignancy) |
NA | Testis (43.8) | Lymphoma (30.3) | Leukemia (8.9) | Colorectal (11.2) | Skin (3.3) | Brain (2.2) | - | - | - | Sperm concentration, motility |
|
Klosky et al (2009) [20] |
66 | 16.63 | 2006~2007 | Solid tumor (28.8) | Leukemia/lymphoma (47.0) | CNS (24.2) | - | - | - | - | - | - | NA |
|
Bonetti et al (2009) [21] |
98 | 33.0 | 1996~2008 | Testicle (56.1) | Prostate (15.3) | Hodgkin's lymphoma (9.2) | Non-Hodgkin's lymphoma (7.1) | Leukemia (3.1) | Other (9.2) | - | - | - | Sperm concentration |
|
Williams et al (2009) [22] |
717 | 29.9 | 2000~2005 | Testicular cancer (45) | Hodgkin's lymphoma (10) | Non-Hodgkin's lymphoma (7) | Sarcoma (6) | Prostate (6) | Leukemia (5) | Gastrointestinal (3) | CNS (2) | - | Sperm density, motility, total motile sperm |
|
Crawshaw et al (2008) [23] |
16 | 15.5 | NA | Sarcoma (NA) lymphoma (NA) | Leukemia (NA) | Germ cell (NA) | CNS (NA) | - | - | - | - | - | NA |
| Present study | 66 | 32.0 | 1999~2014 | Testis (47) | Non-Hodgkin's (15.1) | Hodgkin's (7.6) | Leukemia (12.1) | Gastrointestinal (7.6) | Musculoskeletal (7.6) | Other (3) | - | - | Sperm concentration, viability |
ACKNOWLEDGEMENTS
This study was supported by a clinical grant from Pusan National University Hospital (2014).
References
1. Tschudin S, Bitzer J. Psychological aspects of fertility preservation in men and women affected by cancer and other life-threatening diseases. Hum Reprod Update. 2009; 15:587–597.

2. Glaser AW, Phelan L, Crawshaw M, Jagdev S, Hale J. Fertility preservation in adolescent males with cancer in the United Kingdom: a survey of practice. Arch Dis Child. 2004; 89:736–737.

3. Puscheck E, Philip PA, Jeyendran RS. Male fertility preservation and cancer treatment. Cancer Treat Rev. 2004; 30:173–180.

4. Rofeim O, Gilbert BR. Normal semen parameters in cancer patients presenting for cryopreservation before gonadotoxic therapy. Fertil Steril. 2004; 82:505–506.

6. Lass A, Abusheikha N, Akagbosu F, Brinsden P. Cancer patients should be offered semen cryopreservation. BMJ. 1999; 318:1556.

7. Bahadur G, Farhi J, Ling KL, Techatraisak K, Ashraf A, Oyede AW, et al. Pregnancy and miscarriage rates in 3978 donor insemination cycles: effect of age, parity and partner's infertility status on pregnancy outcome. Hum Fertil (Camb). 2000; 3:207–201.

8. World Health Organization. Laboratory manual of the WHO for the examination of human semen and sperm-cervical mucus interaction. Ann Ist Super Sanita. 2001; 37:I–XII.
9. Spitz S. The histological effects of nitrogen mustards on human tumors and tissues. Cancer. 1948; 1:383–398.

10. Gandini L, Sgrò P, Lombardo F, Paoli D, Culasso F, Toselli L, et al. Effect of chemo- or radiotherapy on sperm parameters of testicular cancer patients. Hum Reprod. 2006; 21:2882–2889.

11. Pont J, Albrecht W. Fertility after chemotherapy for testicular germ cell cancer. Fertil Steril. 1997; 68:1–5.

12. Kenney LB, Laufer MR, Grant FD, Grier H, Diller L. High risk of infertility and long term gonadal damage in males treated with high dose cyclophosphamide for sarcoma during childhood. Cancer. 2001; 91:613–621.

13. Keene DJ, Sajjad Y, Makin G, Cervellione RM. Sperm banking in the United Kingdom is feasible in patients 13 years old or older with cancer. J Urol. 2012; 188:594–597.

14. Amirjannati N, Sadeghi M, Hosseini Jadda SH, Ranjbar F, Kamali K, Akhondi MA. Evaluation of semen quality in patients with malignancies referred for sperm banking before cancer treatment. Andrologia. 2011; 43:317–320.

15. Bizet P, Saias-Magnan J, Jouve E, Grillo JM, Karsenty G, Metzler-Guillemain C, et al. Sperm cryopreservation before cancer treatment: a 15-year monocentric experience. Reprod Biomed Online. 2012; 24:321–330.

16. Chung JP, Haines CJ, Kong GW. Sperm cryopreservation for Chinese male cancer patients: a 17-year retrospective analysis in an assisted reproductive unit in Hong Kong. Hong Kong Med J. 2013; 19:525–530.

17. Hagenäs I, Jørgensen N, Rechnitzer C, Sommer P, Holm M, Schmiegelow K, et al. Clinical and biochemical correlates of successful semen collection for cryopreservation from 12-18-year-old patients: a single-center study of 86 adolescents. Hum Reprod. 2010; 25:2031–2038.
18. Ping P, Zhu WB, Zhang XZ, Yao KS, Xu P, Huang YR, et al. Sperm banking for male reproductive preservation: a 6-year retrospective multi-centre study in China. Asian J Androl. 2010; 12:356–362.

19. Said TM, Tellez S, Evenson DP, Del Valle AP. Assessment of sperm quality, DNA integrity and cryopreservation protocols in men diagnosed with testicular and systemic malignancies. Andrologia. 2009; 41:377–382.

20. Klosky JL, Randolph ME, Navid F, Gamble HL, Spunt SL, Metzger ML, et al. Sperm cryopreservation practices among adolescent cancer patients at risk for infertility. Pediatr Hematol Oncol. 2009; 26:252–260.

21. Bonetti TC, Pasqualotto FF, Queiroz P, Iaconelli A Jr, Borges E Jr. Sperm banking for male cancer patients: social and semen profiles. Int Braz J Urol. 2009; 35:190–197.

22. Williams DH 4th, Karpman E, Sander JC, Spiess PE, Pisters LL, Lipshultz LI. Pretreatment semen parameters in men with cancer. J Urol. 2009; 181:736–740.

23. Crawshaw MA, Glaser AW, Hale JP, Sloper P. Young males' experiences of sperm banking following a cancer diagnosis: a qualitative study. Hum Fertil (Camb). 2008; 11:238–234.
24. Schover LR, Brey K, Lichtin A, Lipshultz LI, Jeha S. Oncologists' attitudes and practices regarding banking sperm before cancer treatment. J Clin Oncol. 2002; 20:1890–1897.

25. Hobbie WL, Ogle SK, Ginsberg JP. Fertility concerns for young males undergoing cancer therapy. Semin Oncol Nurs. 2009; 25:245–250.

26. Lee SJ, Schover LR, Partridge AH, Patrizio P, Wallace WH, Hagerty K, et al. American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol. 2006; 24:2917–2931.

27. Heath JA, Stern CJ. Fertility preservation in children newly diagnosed with cancer: existing standards of practice in Australia and New Zealand. Med J Aust. 2006; 185:538–541.

28. Neal MS, Nagel K, Duckworth J, Bissessar H, Fischer MA, Portwine C, et al. Effectiveness of sperm banking in adolescents and young adults with cancer: a regional experience. Cancer. 2007; 110:1125–1129.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download