Abstract
Abscess formation of the corpus cavernosum is very rare. Here, we report a case of long-term anabolic androgenic steroid (AAS) abuse that is suspected to have facilitated the development of a corpus cavernosum abscess in a healthy bodybuilder. Cultures obtained from the abscess contained Staphylococcus epidermidis, a microorganism that almost exclusively affects immunocompromised patients. Therefore, prompt drainage of pus from cavernosal bodies should be the primary aim of the treatment. This case illustrates the potential danger of AAS suppressing the immune system and causing a serious infection.
Abscess of the corpus cavernosum is an unusual infection and can develop after trauma, as a complication of cavernosography; after intracavernous injection of vasoactive agents or perineal abscess drainage; with intermittent self-catheterization, seeding from periodontal infection or tuberculosis; as a result of neglected penile fracture; or spontaneously from undetermined causes [1,2,3,4].
Androgenic anabolic steroids (AASs) are agents that non-athlete weightlifters commonly use for the purpose of looking leaner or more muscular, simply for enhancing their personal appearance [5]. These compounds are structurally related to testosterone, bind to androgen receptors, and exert masculinizing and anabolic effects to varying degrees [5]. The adverse effects of long-term use of AAS remain unknown.
Here, we report a case of spontaneous corpus cavernosum abscess in a healthy body-builder with a history of long-term high-dose use of AAS.
A 38-year-old well-muscled healthy man presented with a 1-week history of penile swelling and pain. Initially, he noticed a small bump on the left side of his penile shaft, which later became gradually larger and painful. The patient did not have urinary infection; urethral discharge or trauma, including scratching of the genitalia; history of sexually transmitted diseases; tuberculosis; diabetes or any other systemic disorders; or dental carries. His past medical history was unremarkable except for long-term irregular use of AAS. His hobby was muscle training, and he has been receiving various AAS injections (nandrolone and stanozolol) for the past 10 years.
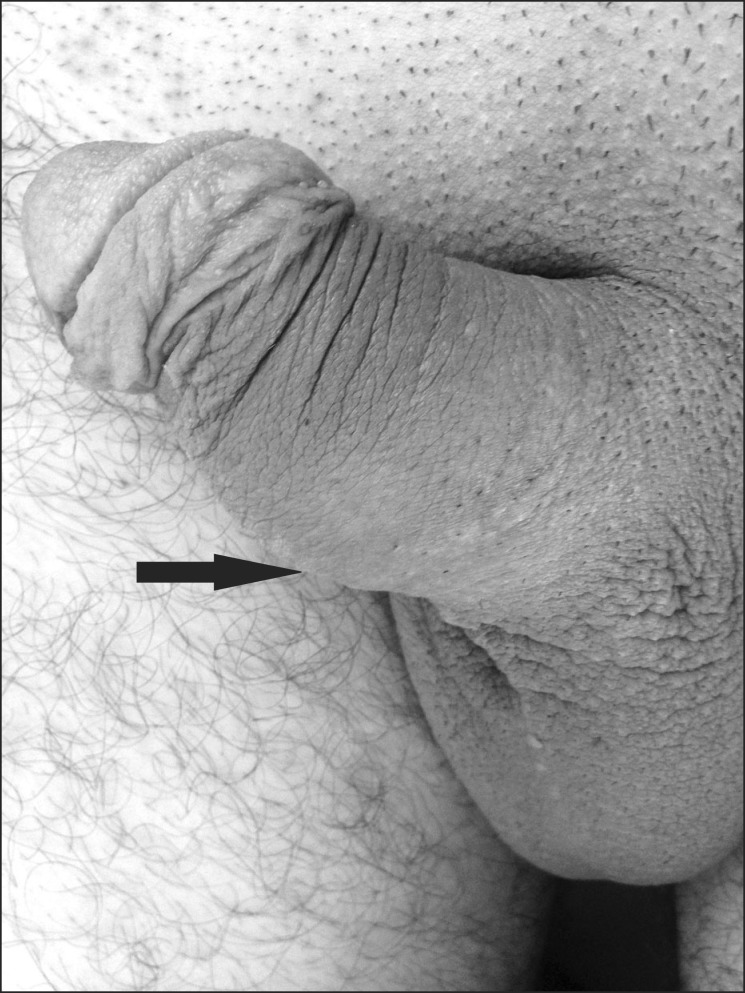
The patient was subfebrile (37.5℃) but hemodynamically stable on admission. Physical examination revealed edema, induration, enlargement, and tenderness in the mid-penile shaft, predominantly on the left side (Fig. 1). Systemic examination did not reveal any finding for an infection focus. Urine analysis showed no abnormalities. The white blood cell count was 12,000 cells/mm3, C-reactive protein level was 1.19 mg/dL (up to 0.5 mg/dL is normal), and total testosterone was remarkably decreased (0.47 ng/dL). Other blood investigations were all within their normal range. Human immunodeficiency virus serology and an rapid plasma reagin test for syphilis were negative. Ultrasound demonstrated a well-circumscribed and heterogeneous area measuring 3.2×2.4 cm, within the middle part of the left corpus cavernosum, with no involvement of the corpus spongiosum or urethra (Fig. 2). No blood flow was detected by Doppler ultrasound. The lesion's appearance was consistent with an abscess.
Initially, blood and urine cultures were obtained. Upon the patient's consent, he underwent immediate surgical intervention. Exploration of the left penile shaft by midline incision revealed an abscess of the corpus cavernosum. The tunica albuginea was opened longitudinally, and about 10 mL of pus was drained. The patient's symptoms disappeared after the removal of purulent material with the placement of a small Penrose drain and injection of broad-spectrum antibiotics for a week. Abscess material was sent for Gram and Ziehl-Neelsen staining, as well as aerobic and anaerobic cultures. Direct microscopic findings were negative for fungal elements. The blood culture did not reveal any pathogen. The pus grew Gram-positive Staphylococcus epidermidis. On 3-month postoperativereview, the patient had good urinary stream, minimal induration, and mild left-sided penile deviation on erection without any sexual dysfunction.
The most commonly identified organisms from cultures of cavernosal abscess materials were reported to be Staphylococcus aureus, streptococci, bacteroides, and fusobacteria [4]. In the present patient, culture of the abscess yielded S. epidermidis, which is a part of the skin microflora. S. epidermidis is a gram-positive, coagulase negative skin colonizing coccus, which does not usually produce aggressive virulence determinants and usually requires an obvious breach in the host's defense mechanism to cause severe infection [6]. Our patient was an otherwise healthy 38-year-old non-athlete weightlifter, and his only notable immunomodulating risk factor was hislong-term use of AAS.
Athletes, bodybuilders, and some other sporting professionals have been using AAS for several decades now as an aid to build muscle mass and strength [5]. AAS helps to achieve a supraphysiological testosterone state, prolonging its action in vivo [5]. At supraphysiological concentrations, AAS has been considered to be immunosuppressive [7]. The results from both animal and human studies suggest that AAS use decreases antibody formation, natural killer cell activity, and T and B lymphocyte maturation and stimulation, resulting in immunosuppression [7]. Further, supraphysiological doses of common AAS have been shown to directly influence the production of certain cytokines, altering the immune function [7]. In a recent study that analyzed the immunological effects of AAS on bodybuilders, it was demonstrated that bodybuilders using AAS had significantly reduced serum immunoglobulin levels as compared to those who did not use AAS [8]. Unsafe needle practices or frequent injections may be possible risk factors for hematogenous seeding of the microorganism in our patient. Because no cause of infectious risks was identified other than long-term use of AAS injections, it is possible to speculate that AAS injections may have contributed to the occurrence of the corpus cavernosum abscess both by suppressing the immune system and by inoculating the organism in this case.
Supraphysiological doses of AAS may mimic medical castration by suppressing serum levels of testosterone, as found in our case. Our patient had low testosterone levels, because exogenous AAS suppresses hypothalamic-pituitary-testicular (HPT) function and users gradually develop suppressed testosterone levels. Upon discontinuation of AAS use after a lengthy course of use, HPT activity may be suppressed for months or years, and some individuals may never regain normal testosterone levels [9]. The present patient had stopped taking AAS injections, but his serum testosterone remained at suppressed levels at follow-up.
In order to prevent the development of serious complications such as necrotizing fasciitis or a bacterial persistence resulting in total penectomy, early surgical intervention is recommended in the case of cavernosal abscess [1,3,4]. Usually, the recovery is well, with the help of postoperative antibiotics. The common complications include poor erectile function affecting sexual activity and secondary fibrosis leading to penile deviation [3,4,10]. Our patient had complete recovery from this abscess and was able to attain satisfactory erectile function at follow-up.
To the best of our knowledge, this is the first reported case of an association between AAS use and cavernosal abscess due to an S. epidermidis infection. In this case, surgical debridement and prompt antimicrobial treatment achieved a cure. Although further research is needed to determine the exact mechanism that AAS has in modulating the immune system, our case illustrates the potential danger of AAS suppressing the immune system and causing a serious infection.
References
1. Ehara H, Kojima K, Hagiwara N, Phuoc NB, Deguchi T. Abscess of the corpus cavernosum. Int J Infect Dis. 2007; 11:553–554. PMID: 17398131.

2. Song W, Ko KJ, Shin SJ, Ryu DS. Penile abscess secondary to neglected penile fracture after intracavernosal vasoactive drug injection. World J Mens Health. 2012; 30:189–191. PMID: 23596611.

3. Köksal T, Kadioğlu A, Tefekli A, Usta M, Beşişik A, Erol B. Spontaneous bacterial abscess of bilateral cavernosal bodies. BJU Int. 1999; 84:1107–1108. PMID: 10571649.

4. Dugdale CM, Tompkins AJ, Reece RM, Gardner AF. Cavernosal abscess due to Streptococcus anginosus: a case report and comprehensive review of the literature. Curr Urol. 2013; 7:51–56. PMID: 24917758.
5. Pope HG Jr, Wood RI, Rogol A, Nyberg F, Bowers L, Bhasin S. Adverse health consequences of performance-enhancing drugs: an Endocrine Society scientific statement. Endocr Rev. 2014; 35:341–375. PMID: 24423981.

6. Otto M. Staphylococcus epidermidis: the accidental pathogen. Nat Rev Microbiol. 2009; 7:555–567. PMID: 19609257.
7. Marshall-Gradisnik S, Green R, Brenu EW, Weatherby RP. Anabolic androgenic steroids effects on the immune system. Cent Eur J Biol. 2009; 4:19–33.
8. Calabrese LH, Kleiner SM, Barna BP, Skibinski CI, Kirkendall DT, Lahita RG, et al. The effects of anabolic steroids and strength training on the human immune response. Med Sci Sports Exerc. 1989; 21:386–392. PMID: 2674590.

9. van Breda E, Keizer HA, Kuipers H, Wolffenbuttel BH. Androgenic anabolic steroid use and severe hypothalamic-pituitary dysfunction: a case study. Int J Sports Med. 2003; 24:195–196. PMID: 12740738.

10. Park SM, Hwang CH, Heo C, Woo JH, Lee TH, Hong SJ, et al. Abscess of the penile corpus cavernosum. Korean J Urol. 2005; 46:1224–1227.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download