Abstract
Purpose
To examine the possibility of reducing the number of cores per prostate biopsy in elderly patients with high levels of prostate-specific antigen (PSA) without significantly lowering the detection rate of prostate cancer.
Materials and Methods
Two hundreds sixteen men with PSA levels >20 ng/mL who underwent prostate biopsies from May 2009 to April 2013 were retrospectively reviewed. With the help of magnetic resonance imaging (MRI), the laterality of the dominant tumor burden in patients was determined. The results of targeted biopsies were compared with those of conventional biopsy procedures.
Results
The mean age and PSA level were 79.5 years and 81.3 ng/mL, respectively, and the overall diagnostic rate of sextant biopsies was 81.9% (177/216). MRI was able to show the tumor burden in 189 of the 216 patients. The detection rate of transrectal ultrasonography (TRUS)-guided targeted biopsies was 87.3% (165/189). Detection rates were comparable with conventional biopsies (81.9% [177/216]) (p=0.23). Of the 177 men in whom the results of the sextant biopsy were positive, 12 men (6.8%) with PSA levels <29 ng/mL did not have any cancer cells according to targeted biopsies. However, all other patients were diagnosed with prostate cancer using the abovementioned techniques.
Conclusions
We believe that TRUS-guided targeted biopsies of the prostate in elderly men with high PSA levels could reduce the number of unnecessary cores per biopsy. However, a risk of detection loss remains. Therefore, we recommend that at least a sextant biopsy should be performed, even in elderly patients, in order to detect prostate cancer.
Patients with high levels of prostate-specific antigen (PSA) have a high likelihood of being diagnosed with advanced prostate cancer.
Prostate biopsy is the most common procedure used to confirm prostate cancer [1], although it is not always a very safe and comfortable procedure. Some complications are associated with prostate biopsy procedures in elderly patients, including various comorbidities and increased anxiety following the procedures [2]. We believe that patients require more carefully managed pre-biopsy procedures in order to reduce the rate of complications. Some researchers have argued that problematic post-biopsy symptoms can be induced through a patient's discomfort caused by anxiety. Wade et al [3] evaluated the psychological impact of prostate biopsies. They reported that minor complications, such as hematuria and hematochezia, can result in increased anxiety in the absence of major complications that require hospitalization. Therefore, we believe that post-biopsy complications should be reduced regardless of their severity. Multiple studies have reported high success rates in the discovery of localized prostate cancer through magnetic resonance imaging (MRI) [45]. MRI can help determine which region of a patient's prostate has the dominant tumor burden. Performing a target biopsy on the dominant region, as determined by MRI, may be able to reduce the rate of complications due to biopsy procedures. Accordingly, we examined the possibility of reducing the number of cores per prostate biopsy in elderly patients with high PSA levels without significantly lowering the rate of detection of prostate cancer.
From May 2009 to April 2013, 216 consecutive men over the age of 75 years with PSA levels >20 ng/mL underwent prostate biopsy at Jeju National University Hospital, and their medical records were reviewed. Of these men, 189 had a suspicious lesion on pre-biopsy diffusion-weighted (DW) MRI, and prostate cancer was confirmed in 177 patients after the full analysis of systemic and targeted biopsies. The exclusion criteria were patients with a history of taking 5-α reductase inhibitors within three months of the biopsy and patients who underwent prostrate biopsy in another hospital.
All anticoagulant therapies were discontinued seven days before the prostate biopsy. Prophylactic oral ciprofloxacin (500 mg) was administered once daily, 30 minutes before the biopsy, and two days after the procedure. Patients performed an enema the night before the biopsy. For the procedure, patients were placed in the left lateral decubitus position. An intrarectal lidocaine jelly injection was administered. A spring-driven 18-gauge needle-core biopsy gun was used. Ultrasound imaging was used to guide a systematic core biopsy and additional three-core targeted biopsies were performed on each patient by urologists with more than six years of experience.
Targeted biopsies were performed based on the information provided by MRI imaging about the tumor burden. The main tumor location was determined using transrectal ultrasound (TRUS), and three cores were then taken of the suspicious lesion. After the targeted biopsy, a systemic biopsy was performed and the number of cores was determined according to the Vienna nomogram, which recommends a different number of prostate biopsy cores according to the age of the patient and prostate volume [6].
MRI was performed with a 3.0-T MRI system (Intera Achieva; Philips Medical Systems, Best, Netherlands) with a pelvic phased-array coil before the prostate biopsy. The imaging protocol included T2-weighted turbo spin-echo imaging and DW imaging. T2-weighted turbo spin-echo images were acquired in three orthogonal planes. DW images were obtained by using the single-shot echo planar imaging technique, with b values of 0 and 500 s/mm2. Apparent diffusion coefficient DW maps were automatically constructed on a pixel-by-pixel basis.
All images were reviewed by two radiologists with four and 11 years of experience in interpreting prostate MRI results (J.S.L. and B.S.K, respectively) and four years of experience in DW imaging. Two radiologists conducted a consensus review of the three axial MR images obtained from all patients to determine which regions had the dominant tumor burden. Each prostate region was scored on a scale of 0 to 2, as follows: 0=no estimated tumor, 1=recessive burden of the estimated tumor, and 2=dominant burden of the estimated tumor.
We recorded the numbers and the locations of positive cores and the Gleason scores of each positive core in each patient's pathology report.
The PSA-adjusted positive core rates for the systemic and targeted biopsies were compared using analysis of covariation. These two groups were subdivided into five groups according to PSA levels and subjected to further statistical tests using SAS version 9.0 (SAS Institute, Cary, NC, USA). All of the tests were two-sided, and p<0.05 were considered to indicate statistical significance.
The Institutional Review Board of Jeju National University Hospital approved this clinical study.
The mean age of the patients was 79.5 years, and their mean PSA level was 81.3 ng/mL. The overall cancer-positive rate of sextant prostate biopsies was 81.9% (177/216), with a rate of 73.9% (51/69) in patients with PSA levels of 20 to 29.9 ng/mL, 81.8% (27/33) in patients with PSA levels of 30 to 39.9 ng/mL, 85.7% (18/21) in patients with PSA levels of 40 to 49.9 ng/mL, and 97.9% (95/97) in patients with PSA levels >50 ng/mL. All men with PSA levels >42 ng/mL had a hard nodule in the prostate that was palpable in a digital rectal examination (Table 1). Radiologists estimated the tumor burden based on MRI results. In 85.6% of the cases (185/216), an area with a dominant tumor burden could be observed, in 12.5% of the cases (27/216), no well-defined areas exhibited a tumor burden, and in 1.9% of the cases (4/216), a suspicious area was found. The overall cancer detection rate of the biopsies was 87.3% (165/189) in the targeted biopsy group and 81.9% (177/216) in the sextant biopsy group. The sensitivity and specificity of MRI were 94.5% and 38.5%, respectively. Its positive predictive value was 87.3% and its negative predictive value was 55.6%. In 12 cases (6.8%), targeted biopsies could not find any signs of cancer. In these cases, the patients had a mean value of PSA less than 29 ng/mL or a prostate volume higher than 70 mL. MRI could not fully detect the dominancy of the tumors, although consistency was observed between areas of recessive burden as indicated by MRI and positive core regions found through biopsy in 58.3% of patients (7/12) (Table 2). In two cases (0.92%), targeted biopsies found cancer that was not detected by the sextant biopsy, and MRI indicated a small tumor burden in two transitional cases. In all patients with PSA levels >30 ng/mL, a targeted biopsy alone was able to detect prostate cancer. Targeted biopsies (8.5%) significantly reduced the proportion of pathologically confirmed benign cores in comparison to bilateral sextant biopsies (22.3%) in patients with PSA levels >20 ng/mL (p<0.001) (Fig. 1). The overall complication rate was 47.4%; nine enrolled patients (4.5%) experienced a major complication requiring hospitalization (rectal bleeding, n=2; sepsis, n=7), and 93 patients (43%) experienced self-limited adverse events after the biopsy (transient hematuria, n=64; hematospermia, n=15; transient rectal bleeding, n=14).
Targeted biopsy effectively targets prostate cancer cells and reduces unnecessary biopsy cores in men with higher PSA levels. However, some risk of false negatives remains. In this study, prostate cancer was not successfully detected via targeted biopsy in 12 out of 177 patients (6.8%) with PSA levels of 20 to 30 ng/mL. We believe that this loss of detection via targeted biopsy was relatively small; however, if these losses are added to the existing rate of false negatives in men with PSA levels between 20 and 30 ng/mL, the overall loss of detection becomes larger. Gerstenbluth et al [1] studied 187 men from a database of 1,250 consecutive TRUS-guided prostate biopsies in patients who presented with PSA levels of at least 20 ng/mL. The overall detection rate was 84.0% (157/187). Of these 187 men, 72 presented with PSA levels of 20 to 30 ng/mL, and 53 (73.6%) were diagnosed with prostate cancer. Nomikos et al [7] found that 85 of 108 men (78.7%) with PSA levels of at least 20 ng/mL were diagnosed with prostate cancer. Our results were similar; we diagnosed prostate cancer in 51 of 69 men (73.9%) presenting with PSA levels of 20 to 29.9 ng/mL.
Patients with high PSA levels have a high likelihood of developing prostate cancer and exhibiting an increasing tumor volume [18]. As a result, we hypothesized that tumor estimation through MRI would be easier in men with high PSA levels than in men with low to intermediate PSA levels. However, MRI-targeted biopsy did not have a positive predictive value of 100% in detecting prostate cancer, even in cases where a large prostate tumor burden was suspected.
Prostate biopsy is a relatively safe method for detecting prostate cancer. Regardless, we believe in the necessity of the informed choice of patients, along with proper pre-biopsy management, because some major complications related to biopsies are still reported. Pinkhasov et al [9] reported that 2.5% of a contemporary cohort required hospitalization or emergency department visits to manage post-biopsy complications. Loeb et al [10] also reported an increasing trend of infectious complications following prostate biopsies. Accordingly, complications following biopsies should be reduced however possible.
Modifying the number of biopsy cores helps to reduce the number of complications associated with biopsy procedures. Berger et al [11] reported that an increased number of cores in prostate biopsy did not result in an increased incidence of major complications after prostate biopsy, however, the incidence of hematospermia was significantly higher in patients with 10 to 15 core samples than in patients who underwent six cores. Madej et al [12] likewise reported no overall relationship between the number of cores and complication rates. However, hematuria and hematochezia were higher in the group with ≥12-core biopsies than in the group whose biopsies involved five to eight cores. Recent research has found that self-limited post-biopsy symptoms such as pain, hematuria, and hematochezia can lead to increased anxiety after biopsy [3]. Therefore, in order to reduce the complication rate and patient anxiety, it is necessary to reduce the number of cores per biopsy procedure when attempting to detect prostate cancer. Simultaneously, the accuracy of each biopsy core should be increased, or at least maintained.
Many authors have reported the advantages of targeted biopsy in identifying prostate cancer. Moore et al [13] performed a systemic review evaluating significant recent improvements in detecting clinically significant prostate cancer through MRI. They argued that MRI-guided biopsy productively detects clinically significant prostate cancer. Non-significant cancer, however, is not fully detected by MRI-targeted biopsy. MRI-targeted prostate biopsy has a high specificity and sensitivity for the detection of significant prostate cancer. They also stated that an average of 3.8 targeted cores were needed to achieve the same rate of detection as 12 cores in conventional biopsy. MRI-based targeted biopsy has recently been suggested to have meaningful results in middle-aged patients with PSA levels <20 ng/mL [14]. Recently, Baco et al [15] reported non-inferiority results of two-core prostate biopsies guided by fused MRI and TRUS images. They conducted a two-core targeted biopsy guided by the computer-assisted fusion of MRI/TRUS images and then a 12-core random biopsy in 175 biopsy-naïve patients. They argued that the two-core targeted biopsy was comparable with the 12-core random biopsy based on the detection rate of clinically significant prostate cancer, which was 38.4% (33/86) in the target biopsy group and 49.4% (44/89) in the 12-core random biopsy group (p=0.2). These results suggest that limited core biopsy may be a viable option.
Our results indicate that TRUS-guided prostate biopsies were still effective in elderly patients with higher PSA levels. In patients with PSA levels >30 ng/mL, a targeted biopsy was able to detect the cancer. However, a targeted biopsy alone was not able to detect prostate cancer in some patients with PSA levels <30 ng/mL. Thus, for elderly men with high PSA levels, we recommend that sextant biopsy be performed, rather than relying exclusively on targeted biopsy with a reduced number of cores, despite the assistance of MRI.
Our study had some limitations. The number of complications was not compared between patients who underwent targeted biopsies and those who underwent wholegland biopsies. Further studies are necessary to evaluate this issue. Second, although we know that good evidence supports the increased detection rate of the 10 to 12-core TRUS-guided biopsy technique in peripheral zone directed biopsies [1617], we generally used traditional sextant biopsy according to the age and prostate volume of each patient. We made this choice because no significant and consistent differences were observed between the results of real-world practice and those suggested in the literature for elderly patients with high PSA levels, and we believe that an overall detection rate of approximately 74% to 84% is sufficient to find clinically significant prostate cancer in the elderly. However, we also used the 12-core biopsy technique in patients who did not fit the profile of elderly patients with high PSA levels.
We observed that MRI-assisted targeted biopsy in elderly patients with high PSA levels was able to reduce the number of unnecessary biopsy cores. However, the detection rate of this technique was not completely satisfactory in these patients. Therefore, we suggest that sextant biopsies are still necessary to ensure the detection of prostate cancer, and that TRUS-guided targeted biopsy after MRI analysis should be used as a supplementary method.
Figures and Tables
Fig. 1
Comparison of positive core rates between bilateral sextant and targeted biopsies according to prostate-specific antigen (PSA) levels.

Table 1
Characteristics of patients confirmed to have prostate cancer and the results of their prostate cores
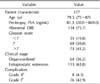
Values are presented as number only, median (range), number (%).
PSA: prostate-specific antigen, DRE: digital rectal examination.
aRequiring pharmacological treatment with drugsor surgical and endoscopic intervention. bAny deviation from the normal postoperative course without the need for pharmacological treatment or surgical, endoscopic,and radiological interventions.
Table 2
Characteristics of patients in whom targeted prostate biopsy failed to detect prostate cancer

ACKNOWLEDGEMENTS
This research was supported by the 2015 scientific promotion program funded by Jeju National University.
References
1. Gerstenbluth RE, Seftel AD, Hampel N, Oefelein MG, Resnick MI. The accuracy of the increased prostate specific
antigen level (greater than or equal to 20 ng./ml.) in predicting
prostate cancer: is biopsy always required? J Urol. 2002; 168:1990–1993.
2. Anastasiadis A, Zapała L, Cordeiro E, Antoniewicz A, Dimitriadis G, De Reijke T. Complications of prostate biopsy. Expert Rev Anticancer Ther. 2013; 13:829–837.

3. Wade J, Rosario DJ, Macefield RC, Avery KN, Salter CE, Goodwin ML, et al. Psychological impact of prostate biopsy: physical symptoms, anxiety, and depression. J Clin Oncol. 2013; 31:4235–4241.

4. Isebaert S, Van den Bergh L, Haustermans K, Joniau S, Lerut E, De Wever L, et al. Multiparametric MRI for prostate cancer localization in correlation to whole-mount histopathology. J Magn Reson Imaging. 2013; 37:1392–1401.

5. Shigemura K, Yamanaka N, Yamashita M. Can diffusion-weighted magnetic resonance imaging predict a high Gleason score of prostate cancer? Korean J Urol. 2013; 54:234–238.

7. Nomikos M, Mariappan P, Zachou A, McNeill A, Bollina PR. Could prostate biopsies be avoided in men older than 75 years with raised PSA? Urol Int. 2010; 85:410–414.

8. Carvalhal GF, Daudi SN, Kan D, Mondo D, Roehl KA, Loeb S, et al. Correlation between serum prostate-specific antigen and cancer volume in prostate glands of different sizes. Urology. 2010; 76:1072–1076.

9. Pinkhasov GI, Lin YK, Palmerola R, Smith P, Mahon F, Kaag MG, et al. Complications following prostate needle biopsy requiring hospital admission or emergency department visits - experience from 1000 consecutive cases. BJU Int. 2012; 110:369–374.

10. Loeb S, van den Heuvel S, Zhu X, Bangma CH, Schröder FH, Roobol MJ. Infectious complications and hospital admissions after prostate biopsy in a European randomized trial. Eur Urol. 2012; 61:1110–1114.

11. Berger AP, Gozzi C, Steiner H, Frauscher F, Varkarakis J, Rogatsch H, et al. Complication rate of transrectal ultrasound guided prostate biopsy: a comparison among 3 protocols with 6, 10 and 15 cores. J Urol. 2004; 171:1478–1480. discussion 1480-1

12. Madej A, Wilkosz J, Różański W, Lipiński M. Complication rates after prostate biopsy according to the number of sampled cores. Cent European J Urol. 2012; 65:116–118.
13. Moore CM, Robertson NL, Arsanious N, Middleton T, Villers A, Klotz L, et al. Image-guided prostate biopsy using magnetic resonance imaging-derived targets: a systematic review. Eur Urol. 2013; 63:125–140.

14. Pokorny MR, de Rooij M, Duncan E, Schröder FH, Parkinson R, Barentsz JO, et al. Prospective study of diagnostic accuracy comparing prostate cancer detection by transrectal ultrasound-guided biopsy versus magnetic resonance (MR) imaging with subsequent MR-guided biopsy in men without previous prostate biopsies. Eur Urol. 2014; 66:22–29.

15. Baco E, Rud E, Eri LM, Moen G, Vlatkovic L, Svindland A, et al. A randomized controlled trial to assess and compare the outcomes of two-core prostate biopsy guided by fused magnetic resonance and transrectal ultrasound images and traditional 12-core systematic biopsy. Eur Urol. 2015; DOI: 10.1016/j.eururo.2015.03.341. [Epub].





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download