This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
The aim of the present study was to evaluate preoperative acute urinary retention (AUR) as a factor affecting the outcomes of patients who underwent photoselective vaporization of the prostate (PVP), both in terms of overall effectiveness and the postoperative incidence of AUR.
Materials and Methods
Baseline prostate characteristics were obtained for patients who underwent PVP, including prostate-specific antigen (PSA) levels, transrectal ultrasound findings, voiding diary parameters, the International Prostate Symptoms Score (IPSS), and uroflowmetry parameters. These parameters were assessed two weeks, one month, three months, six months, and three years postoperatively. Subjects were divided into AUR and non-AUR groups based on the preoperative occurrence of AUR.
Results
Of the 476 patients, 91 had at least one episode of preoperative AUR. The AUR group was found to be significantly older and to have significantly higher PSA levels, lower body mass indices, and larger prostates. At one year of follow-up, the total IPSS was 7.6±6.8 in the AUR group and 11.4±8.2 in the non-AUR group, with the AUR group showing a more significant improvement. In the non-AUR group, 17 of the 385 patients (4.4%) experienced postoperative retention, compared to 16 of the 91 patients (17.6%) patients in the AUR group.
Conclusions
Almost all patients exhibited improvements in subjective and objective voiding parameters following PVP, regardless of the presence of preoperative urinary retention. Patients with a preoperative history of AUR had a higher risk of postoperative retention.
Go to :

Keywords: Laser therapy, Lower urinary tract symptoms, Prostate, Urinary retention
INTRODUCTION
Benign prostatic hyperplasia (BPH) is highly prevalent in elderly men and is the most common cause of lower urinary tract symptoms (LUTS) [
12]. BPH is also the most common disorder that reduces men's quality of life (QoL) [
3]. Urinary symptoms from BPH become more frequent with advanced age, and approximately 80% of men in their 70s suffer from BPH-related LUTS [
4]. As Korea is quickly becoming an aging society, the incidence of LUTS caused by BPH is expected to rise accordingly.
Acute urinary retention (AUR) is a serious and common complication of BPH that often requires painful emergency urinary drainage via catheterization, directly affecting patients' QoL. Longstanding or repeated urinary retention can even potentially lead to the development of chronic renal failure [
5]. Factors related to AUR include old age, urinary tract infections, low peak urinary flow rate, and large prostate volume [
6]. AUR is an indication for surgery, including a reported 25% to 30% of patients undergoing transurethral resection of the prostate [
7].
The objective of this study was to retrospectively evaluate the effect of AUR on the outcomes of patients who underwent photovaporization of the prostate (PVP). We also analyzed urodynamic parameters capable of affecting long-term voiding symptoms and QoL in the same cohort, with the goal of improving the preoperative counseling of patients.
Go to :

MATERIALS AND METHODS
We retrospectively analyzed 476 men who underwent PVP between January 2008 and July 2012. All operations were performed by a single surgeon. The study protocol was approved by the Institutional Review Board of Seoul National University College of Medicine (06-2011-189). The procedure in the present study complies with the Declaration of Helsinki (Edinburgh revision, 2000).
All procedures were performed using a 120-W Green-Light high performance system laser. Medical histories and physical examinations were performed, as well as preoperative evaluations including transrectal ultrasound (TRUS) and multichannel video urodynamics (MMS UD-2000; Medical Measurement System, Enscheded, The Netherlands). Age, serum prostate-specific antigen (PSA), International Prostate Symptom Score (IPSS), maximal flow rate (Qmax), postvoid urine volume (PVR), voiding diary parameters, urodynamic parameters, and surgical methods were analyzed. Data from IPSS, uroflowmetry, and PVR were collected preoperatively and two weeks, one month, three months, six months, and up to three years postoperatively. In some cases, IPSS data were collected through a telephone survey. We only included patients who underwent at least three months of follow-up. Patients who had a preoperative history of AUR and urethral catheterization using an indwelling Foley catheter or intermittent catheterization were categorized into the AUR group. Patients with no history of AUR were categorized into the non-AUR group. Treatment success was defined as improvement in the IPSS score one year postoperatively.
Variables are presented as mean±standard deviation. All preoperative and postoperative variables were analyzed for statistically significant differences using the independent t-test. Analysis of variance or the paired t-test was used to compare preoperative and postoperative clinical parameters. Logistic regression analysis was used to evaluate predictors of response to treatment. p<0.05 were considered to indicate statistical significance, and statistical analyses were performed using PASW Statistics ver. 18.0 (IBM Co., Armonk, NY, USA).
Go to :

RESULTS
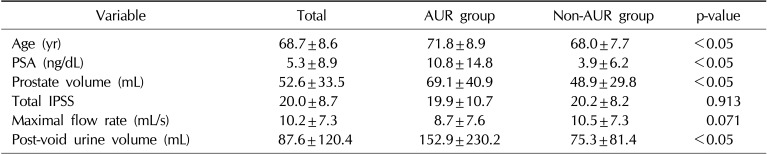
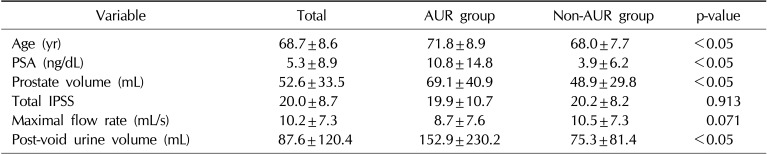
Of the 476 patients analyzed, 91 had at least one episode of AUR before undergoing surgery. The mean age of the total population was 68.7±8.6 years and the mean PSA was 5.3±8.9 ng/mL. The mean prostate volume as measured by TRUS was 52.6±33.5 mL. The mean total IPSS was 20.0±8.7, and the mean Qmax was 10.2±7.3 mL/s. The mean PVR was 87.6±120.4 mL. The mean period from the most recent AUR episode to PVP was 10.8±2.9 days. Baseline characteristics according to whether patients had a history of AUR are presented in
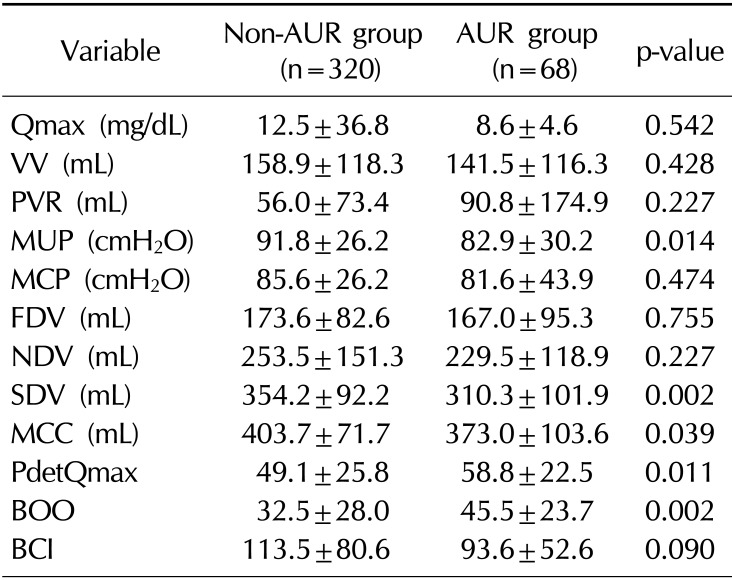
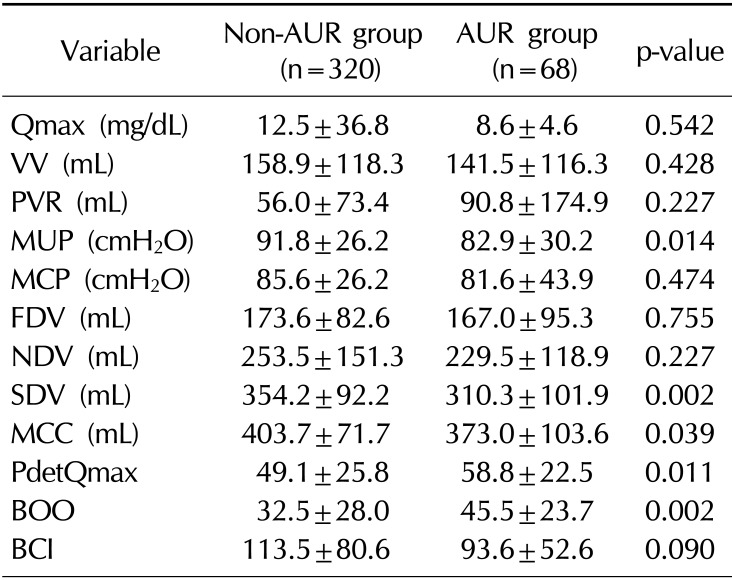
Table 1. The following urodynamic parameters showed significant differences between the AUR and non-AUR groups: maximal urethral closing pressure (82.9±30.2 cmH
2O vs. 91.8±26.2 cmH
2O; p=0.014), maximal cystometric capacity (373.0±103.6 mL vs. 403.7±71.7 mL; p=0.039), detrusor pressure at Qmax (58.8±22.5 cmH
2O vs. 49.1±25.8 cmH
2O; p=0.011), and the bladder outlet obstruction index (45.5±23.7 vs. 32.5±28.0; p=0.002).
Table 1
Preoperative characteristics of the patients
|
Variable |
Total |
AUR group |
Non-AUR group |
p-value |
|
Age (yr) |
68.7±8.6 |
71.8±8.9 |
68.0±7.7 |
<0.05 |
|
PSA (ng/dL) |
5.3±8.9 |
10.8±14.8 |
3.9±6.2 |
<0.05 |
|
Prostate volume (mL) |
52.6±33.5 |
69.1±40.9 |
48.9±29.8 |
<0.05 |
|
Total IPSS |
20.0±8.7 |
19.9±10.7 |
20.2±8.2 |
0.913 |
|
Maximal flow rate (mL/s) |
10.2±7.3 |
8.7±7.6 |
10.5±7.3 |
0.071 |
|
Post-void urine volume (mL) |
87.6±120.4 |
152.9±230.2 |
75.3±81.4 |
<0.05 |

At one year of follow-up, the mean postoperative IPSS was reduced to 10.8±8.1, and the mean Qmax increased to 16.3±20.0 mL/s. The mean PVR was 34.0±49.5 mL. Statistically significant differences were found between the AUR and non-AUR groups in the following parameters: mean age (71.8±8.9 years vs. 68.0±7.7 years), PSA levels (10.8±14.8 ng/mL vs. 3.9±6.2 ng/mL), body mass index (22.7±3.2 kg/m2 vs. 24.2±3.0 kg/m2), and prostate size (69.1±40.9 mL vs. 48.9±29.8 mL), showing that the AUR group was older, had higher PSA levels, lower body mass indices, and larger prostates. No significant differences in voiding diary parameters were observed. Furthermore, the AUR group had longer mean operation times (85.7±50.2 minutes vs. 69.2±45.4 minutes) and lasing times (32.4±18.2 minutes vs. 26.8±24.6 minutes). Uroflowmetry reports in the first two weeks of follow-up showed that the AUR group had lower Qmax values (11.4±5.5 mL/s vs. 14.4±7.8 mL/s) and a higher PVR; however, no significant differences in PVR were observed in later follow-up.
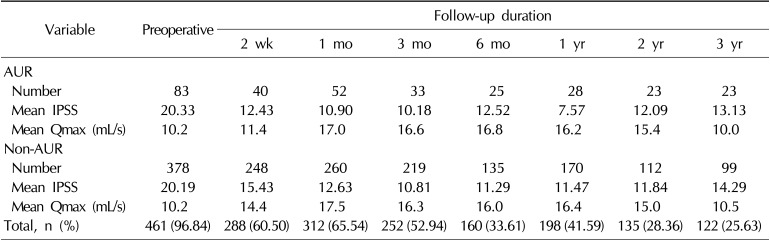
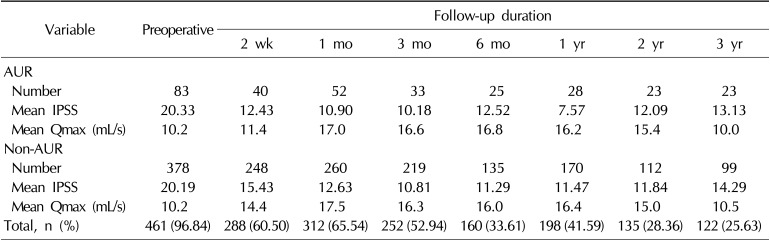
At the one-year follow-up, the mean IPSS was 10.9±8.1 (n=198, 41.6%) and the mean Qmax was 16.3±20.1 mL/s (n=203, 42.6%). At the two-year follow-up, the mean IPSS was 11.9±7.8 (n=134, 28.2%) and the mean Qmax was 15.2±14.4 mL/s (n=100, 21%). At the three-year follow-up, the mean IPSS was 14.1±8.9 (n=122, 25.6%) and the mean Qmax was 10.3±5.8 mL/s (n=10, 2.1%). The follow-up percentages by group are shown in
Table 2.
Table 2
Mean IPSS and Qmax values at various follow-up durations
|
Variable |
Preoperative |
Follow-up duration |
|
2 wk |
1 mo |
3 mo |
6 mo |
1 yr |
2 yr |
3 yr |
|
AUR |
|
|
|
|
|
|
|
|
|
Number |
83 |
40 |
52 |
33 |
25 |
28 |
23 |
23 |
|
Mean IPSS |
20.33 |
12.43 |
10.90 |
10.18 |
12.52 |
7.57 |
12.09 |
13.13 |
|
Mean Qmax (mL/s) |
10.2 |
11.4 |
17.0 |
16.6 |
16.8 |
16.2 |
15.4 |
10.0 |
|
Non-AUR |
|
|
|
|
|
|
|
|
|
Number |
378 |
248 |
260 |
219 |
135 |
170 |
112 |
99 |
|
Mean IPSS |
20.19 |
15.43 |
12.63 |
10.81 |
11.29 |
11.47 |
11.84 |
14.29 |
|
Mean Qmax (mL/s) |
10.2 |
14.4 |
17.5 |
16.3 |
16.0 |
16.4 |
15.0 |
10.5 |
|
Total, n (%) |
461 (96.84) |
288 (60.50) |
312 (65.54) |
252 (52.94) |
160 (33.61) |
198 (41.59) |
135 (28.36) |
122 (25.63) |

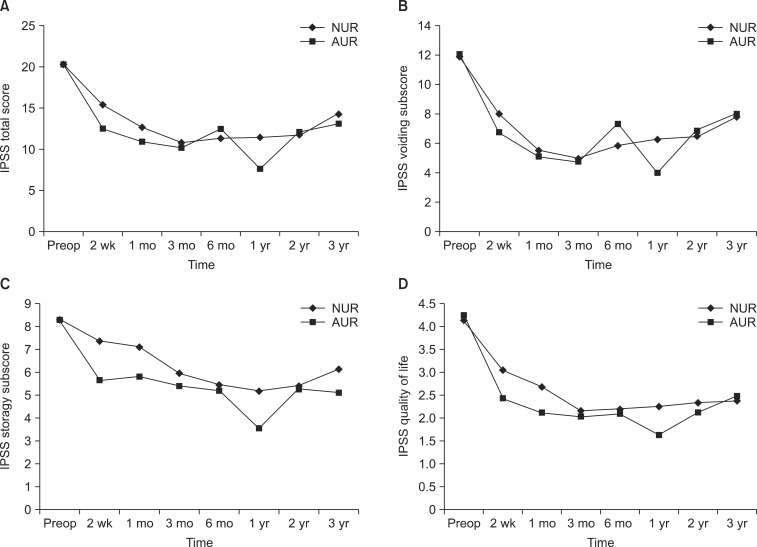
At one year of follow-up, the mean IPSS was 7.6±6.8 in the AUR group and 11.4±8.2 in the non-AUR group, with significantly more improvement observed in the AUR group than in the non-AUR group.
Fig. 1 shows changes in the total IPSS from baseline to three years of follow-up, divided into scores for voiding symptoms, storage symptoms, and QoL. Seventeen patients in the non-AUR group (4.4%) and 16 of the 91 (17.6%) patients in the AUR group presented with postoperative AUR. The chi-square test revealed that the AUR group had a 4.6 times higher risk of retention than the non-AUR group.
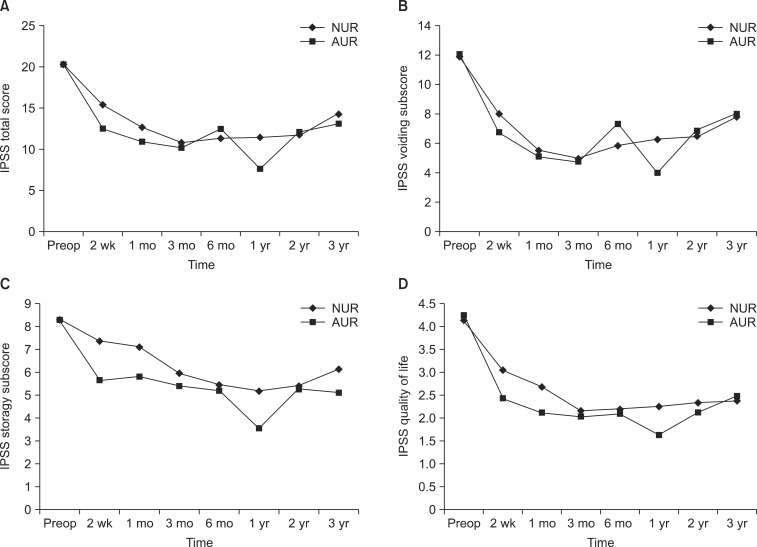 | Fig. 1Changes in International Prostate Symptom Scores (IPSS). (A) Total scores, reflecting all symptoms. (B) Subscores reflecting voiding symptoms. (C) Subscores reflecting storage symptoms. (D) Quality of life scores. NUR: no urinary retention, AUR: acute urinary retention, Preop: preoperative.
|
Multivariate logistic regression analysis showed that old age (>70 years) (odds ratio [OR]=1.5, 95% confidence interval [CI]=1.20~1.78), maximal cystometric capacity (OR=1.1, 95% CI=1.05~1.35) and a history of AUR (OR=2.5, 95% CI=1.89~3.75) were significant predictors of IPSS improvement one year postoperatively, as shown in
Table 3.
Table 3
Comparison of urodynamic parameters according to the presence of preoperative AUR
|
Variable |
Non-AUR group (n=320) |
AUR group (n=68) |
p-value |
|
Qmax (mg/dL) |
12.5±36.8 |
8.6±4.6 |
0.542 |
|
VV (mL) |
158.9±118.3 |
141.5±116.3 |
0.428 |
|
PVR (mL) |
56.0±73.4 |
90.8±174.9 |
0.227 |
|
MUP (cmH2O) |
91.8±26.2 |
82.9±30.2 |
0.014 |
|
MCP (cmH2O) |
85.6±26.2 |
81.6±43.9 |
0.474 |
|
FDV (mL) |
173.6±82.6 |
167.0±95.3 |
0.755 |
|
NDV (mL) |
253.5±151.3 |
229.5±118.9 |
0.227 |
|
SDV (mL) |
354.2±92.2 |
310.3±101.9 |
0.002 |
|
MCC (mL) |
403.7±71.7 |
373.0±103.6 |
0.039 |
|
PdetQmax |
49.1±25.8 |
58.8±22.5 |
0.011 |
|
BOO |
32.5±28.0 |
45.5±23.7 |
0.002 |
|
BCI |
113.5±80.6 |
93.6±52.6 |
0.090 |

Go to :

DISCUSSION
PVP is one of the surgical treatments available for BPH. Several studies have asserted the efficacy and safety of PVP with a GreenLight laser, including among the Korean male population [
891011121314]. In 2005, Malek et al [
13] reported excellent clinical outcomes involving sustained symptomatic and urodynamic improvements with a minimum necessity for reintervention during a five-year period of postoperative follow-up. In another five-year follow-up study, Hai [
14] reported improvement in IPSS, QoL scores, Qmax, TRUS findings, and PVR. Our data also showed improvement in clinical parameters in both the AUR and non-AUR groups. Although some differences between these two groups were observed regarding age, PSA, body mass index, and prostate size, immediate and sustained improvements in IPSS, QoL, PVR and Qmax were reported.
At the second postoperative week, the AUR group had significantly lower Qmax and higher PVR values. However, no significant differences were observed in these uroflowmetric parameters on subsequent follow-up visits. This possibly means that patients with preoperative retention require more time to recover than those without preoperative retention. Another interesting point in our study is that the AUR group had better IPSS results than the non-AUR group at one year of follow-up. This suggests that PVP is an efficient method for treating BPH regardless of whether a patient has a history of AUR. Jacobsen et al [
6] found that AUR had a direct relationship with LUTS, old age, low Qmax, and enlarged prostate. In our study, the same parameters were also found to be associated with the AUR group.
The hemostatic properties of the GreenLight laser stem from the selective absorption of energy in vessels containing hemoglobin with minimal energy propagation through water. Since bleeding can be easily controlled during the operation, operators can obtain a better visual field than in conventional transurethral prostate surgery. The excellent clinical outcomes, low morbidity, technical simplicity, and cost-effectiveness of GreenLight laser PVP have made this technology a valid and efficacious clinical alternative to the conventional transurethral resection of the prostate [
1516]. In our experience, patients undergoing PVP have low complication rates, and the procedure has been found to have remained effective in 60% of patients three years postoperatively [
11].
Our analysis of preoperative urodynamic parameters showed that the AUR group had lower maximal urethral closing pressure and maximal cystometric capacity, but higher detrusor pressure at the Qmax and a higher bladder outlet obstruction index. Furthermore, maximal cystometric capacity was a significant predictor in the multivariate logistic regression analysis. Although a higher bladder outlet obstruction index is expected to occur in patients with AUR to some extent, the finding of a lower maximal cystometric capacity was less expected, and may have been due to the fact that AUR patients who were unable to void did not complete the study, and no data on bladder capacity were included [
17]. Djavan et al [
18] suggested that a history of AUR and low maximal detrusor pressure were the most important factors accounting for a high risk of treatment failure after conventional transurethral resection of the prostate. However, since the detrusor may recover in some patients, the authors recommended prostate surgery in such patients even if preoperative urodynamics suggest an unfavorable outcome. Even though our study did not focus on the treatment failure rate, only three patients with low maximal detrusor pressure (<28 cm of water) exhibited postoperative retention.
This study has several limitations. First, as a retrospective study based on electronic medical records, it was susceptible to bias and dependent on the integrity of the record keeping. Second, the data might have been biased since some of the uroflowmetry measurements were taken during episodes of retention or when the patients complained of voiding difficulty. Lastly, this study did not analyze the use of drugs such as alpha agonists, 5-alpha reductase inhibitors, or anticholinergics. Such drugs might have had an impact on the presence of AUR both preoperatively and postoperatively. However, clinicians prescribed these medications according to the same criteria regardless of the presence of preoperative AUR.
Go to :

CONCLUSIONS
In this study, almost all patients experienced improvements in subjective and objective voiding parameters following PVP, regardless of the presence of preoperative urinary retention. Patients with a history of AUR had a higher risk of postoperative retention. This information may be useful when counseling patients who are scheduled to undergo PVP operations about their prognosis and further management options.
Go to :





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download