1. Zhang ZH, Zhu HB, Li LL, Yu Y, Zhang HG, Liu RZ. Decline of semen quality and increase of leukocytes with cigarette smoking in infertile men. Iran J Reprod Med. 2013; 11:589–596. PMID:
24639795.
2. Saleh RA, Agarwal A, Sharma RK, Nelson DR, Thomas AJ Jr. Effect of cigarette smoking on levels of seminal oxidative stress in infertile men: a prospective study. Fertil Steril. 2002; 78:491–499. PMID:
12215323.

3. Trummer H, Habermann H, Haas J, Pummer K. The impact of cigarette smoking on human semen parameters and hormones. Hum Reprod. 2002; 17:1554–1559. PMID:
12042277.

4. Ng M, Freeman MK, Fleming TD, Robinson M, Dwyer-Lindgren L, Thomson B, et al. Smoking prevalence and cigarette consumption in 187 countries, 1980-2012. JAMA. 2014; 311:183–192. PMID:
24399557.

5. World Health Organization. Infections, pregnancies, and infertility: perspectives on prevention. Fertil Steril. 1987; 47:964–968. PMID:
3595902.
6. Odisho AY, Nangia AK, Katz PP, Smith JF. Temporal and geospatial trends in male factor infertility with assisted reproductive technology in the United States from 1999-2010. Fertil Steril. 2014; 102:469–475. PMID:
24931206.

7. Zinaman MJ, Brown CC, Selevan SG, Clegg ED. Semen quality and human fertility: a prospective study with healthy couples. J Androl. 2000; 21:145–153. PMID:
10670528.
8. Lewin A, Gonen O, Orvieto R, Schenker JG. Effect of smoking on concentration, motility and zona-free hamster test on human sperm. Arch Androl. 1991; 27:51–54. PMID:
1772308.

9. Chia SE, Lim ST, Tay SK, Lim ST. Factors associated with male infertility: a case-control study of 218 infertile and 240 fertile men. BJOG. 2000; 107:55–61. PMID:
10645862.

10. Künzle R, Mueller MD, Hänggi W, Birkhäuser MH, Drescher H, Bersinger NA. Semen quality of male smokers and nonsmokers in infertile couples. Fertil Steril. 2003; 79:287–291. PMID:
12568836.

11. Adelusi B, al-Twaijiri MH, al-Meshari A, Kangave D, al-Nuaim LA, Younnus B. Correlation of smoking and coffee drinking with sperm progressive motility in infertile males. Afr J Med Med Sci. 1998; 27:47–50. PMID:
10456129.
12. Sergerie M, Ouhilal S, Bissonnette F, Brodeur J, Bleau G. Lack of association between smoking and DNA fragmentation in the spermatozoa of normal men. Hum Reprod. 2000; 15:1314–1321. PMID:
10831562.

13. Hoidas S, Williams AE, Tocher JL, Hargreave TB. Scoring sperm morphology from fertile and infertile cigarette smokers using the scanning electron microscope and image analysis. Fertil Steril. 1985; 43:595–598. PMID:
3987928.

14. Vogt HJ, Heller WD, Borelli S. Sperm quality of healthy smokers, ex-smokers, and never-smokers. Fertil Steril. 1986; 45:106–110. PMID:
3943641.

15. Brugo-Olmedo S, Chillik C, Kopelman S. Definition and causes of infertility. Reprod Biomed Online. 2001; 2:41–53. PMID:
12537824.

16. Marinelli D, Gaspari L, Pedotti P, Taioli E. Mini-review of studies on the effect of smoking and drinking habits on semen parameters. Int J Hyg Environ Health. 2004; 207:185–192. PMID:
15330386.

17. Practice Committee of American Society for Reproductive Medicine. Smoking and infertility. Fertil Steril. 2008; 90:S254–S259. PMID:
19007641.
18. Hammond D, Fong GT, Cummings KM, O'Connor RJ, Giovino GA, McNeill A. Cigarette yields and human exposure: a comparison of alternative testing regimens. Cancer Epidemiol Biomarkers Prev. 2006; 15:1495–1501. PMID:
16896039.

19. Colagar AH, Jorsaraee GA, Marzony ET. Cigarette smoking and the risk of male infertility. Pak J Biol Sci. 2007; 10:3870–3874. PMID:
19090244.
20. Richthoff J, Elzanaty S, Rylander L, Hagmar L, Giwercman A. Association between tobacco exposure and reproductive parameters in adolescent males. Int J Androl. 2008; 31:31–39. PMID:
17376217.

21. Zhu AZ, Zhou Q, Cox LS, Ahluwalia JS, Benowitz NL, Tyndale RF. Variation in trans-3'-hydroxycotinine glucuronidation does not alter the nicotine metabolite ratio or nicotine intake. PLoS One. 2013; 8:e70938. PMID:
23936477.

22. Pacifici R, Altieri I, Gandini L, Lenzi A, Pichini S, Rosa M, et al. Nicotine, cotinine, and trans-3-hydroxycotinine levels in seminal plasma of smokers: effects on sperm parameters. Ther Drug Monit. 1993; 15:358–363. PMID:
8249041.
23. Oliveira H, Spanò M, Santos C, Pereira Mde L. Adverse effects of cadmium exposure on mouse sperm. Reprod Toxicol. 2009; 28:550–555. PMID:
19695322.

24. Oldereid NB, Thomassen Y, Purvis K. Seminal plasma lead, cadmium and zinc in relation to tobacco consumption. Int J Androl. 1994; 17:24–28. PMID:
8005705.

25. Chia SE, Xu B, Ong CN, Tsakok FM, Lee ST. Effect of cadmium and cigarette smoking on human semen quality. Int J Fertil Menopausal Stud. 1994; 39:292–298. PMID:
7820163.
26. Pant N, Kumar G, Upadhyay AD, Gupta YK, Chaturvedi PK. Correlation between lead and cadmium concentration and semen quality. Andrologia. 2015; 47:887–891. PMID:
25228328.

27. Stillman RJ, Rosenberg MJ, Sachs BP. Smoking and reproduction. Fertil Steril. 1986; 46:545–566. PMID:
3530822.

28. Sofikitis N, Miyagawa I, Dimitriadis D, Zavos P, Sikka S, Hellstrom W. Effects of smoking on testicular function, semen quality and sperm fertilizing capacity. J Urol. 1995; 154:1030–1034. PMID:
7637048.

29. Vine MF, Tse CK, Hu P, Truong KY. Cigarette smoking and semen quality. Fertil Steril. 1996; 65:835–842. PMID:
8654648.

30. Merino G, Lira SC, Martínez-Chéquer JC. Effects of cigarette smoking on semen characteristics of a population in Mexico. Arch Androl. 1998; 41:11–15. PMID:
9642454.

31. Meeker JD, Benedict MD. Infertility, pregnancy loss and adverse birth outcomes in relation to maternal secondhand tobacco smoke exposure. Curr Womens Health Rev. 2013; 9:41–49. PMID:
23888128.

32. Pirkle JL, Bernert JT, Caudill SP, Sosnoff CS, Pechacek TF. Trends in the exposure of nonsmokers in the U.S. population to secondhand smoke: 1988-2002. Environ Health Perspect. 2006; 114:853–858. PMID:
16759984.

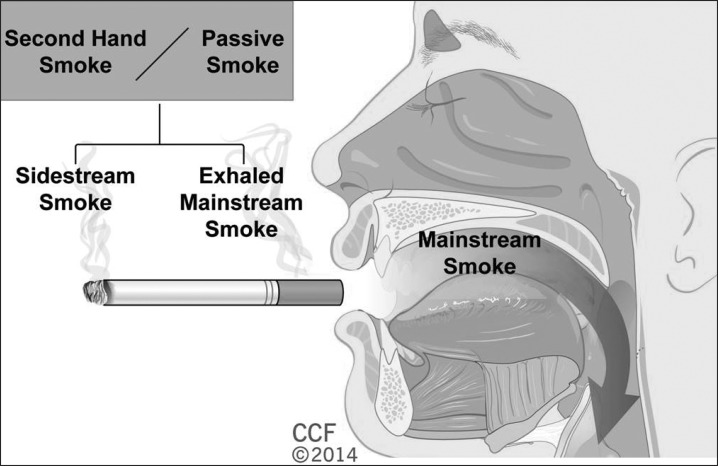
33. Polyzos A, Schmid TE, Piña-Guzmán B, Quintanilla-Vega B, Marchetti F. Differential sensitivity of male germ cells to mainstream and sidestream tobacco smoke in the mouse. Toxicol Appl Pharmacol. 2009; 237:298–305. PMID:
19345701.

34. Office on Smoking and Health (US). The health consequences of involuntary exposure to tobacco smoke: a report of the surgeon general. Atlanta (GA): Centers for Disease Control and Prevention (US);2006.
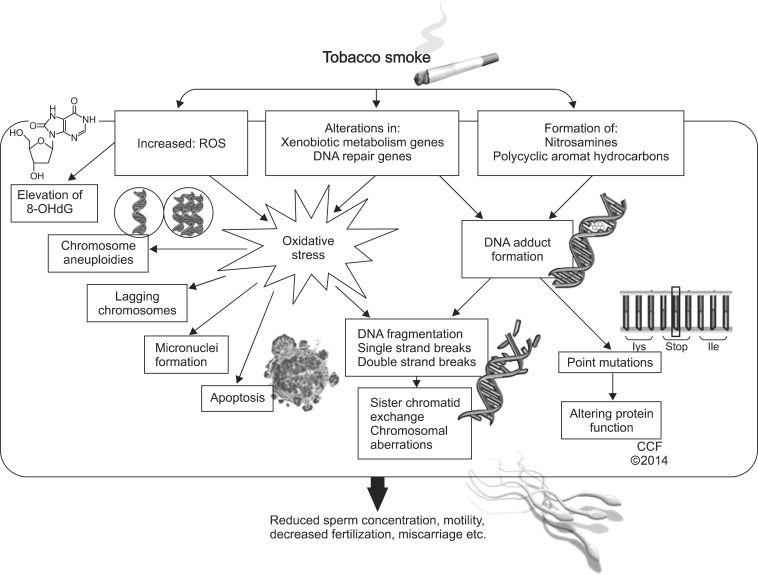
35. Tremellen K. Oxidative stress and male infertility: a clinical perspective. Hum Reprod Update. 2008; 14:243–258. PMID:
18281241.

36. Kao SH, Chao HT, Chen HW, Hwang TI, Liao TL, Wei YH. Increase of oxidative stress in human sperm with lower motility. Fertil Steril. 2008; 89:1183–1190. PMID:
17669405.

37. Xu LC, Wang SY, Yang XF, Wang XR. Effects of cadmium on rat sperm motility evaluated with computer assisted sperm analysis. Biomed Environ Sci. 2001; 14:312–317. PMID:
11862611.
38. Kumosani TA, Elshal MF, Al-Jonaid AA, Abduljabar HS. The influence of smoking on semen quality, seminal microelements and Ca2+-ATPase activity among infertile and fertile men. Clin Biochem. 2008; 41:1199–1203. PMID:
18708043.

39. Besaratinia A, Tommasi S. Electronic cigarettes: the road ahead. Prev Med. 2014; 66:65–67. PMID:
24952095.

40. Goniewicz ML, Knysak J, Gawron M, Kosmider L, Sobczak A, Kurek J, et al. Levels of selected carcinogens and toxicants in vapour from electronic cigarettes. Tob Control. 2014; 23:133–139. PMID:
23467656.

41. Kim HJ, Shin HS. Determination of tobacco-specific nitrosamines in replacement liquids of electronic cigarettes by liquid chromatography-tandem mass spectrometry. J Chromatogr A. 2013; 1291:48–55. PMID:
23602640.

42. Harrell PT, Simmons VN, Correa JB, Padhya TA, Brandon TH. Electronic nicotine delivery systems ("e-cigarettes"): review of safety and smoking cessation efficacy. Otolaryngol Head Neck Surg. 2014; 151:381–393. PMID:
24898072.
43. Burstyn I. Peering through the mist: systematic review of what the chemistry of contaminants in electronic cigarettes tells us about health risks. BMC Public Health. 2014; 14:18. PMID:
24406205.

44. Nair U, Bartsch H, Nair J. Alert for an epidemic of oral cancer due to use of the betel quid substitutes gutkha and pan masala: a review of agents and causative mechanisms. Mutagenesis. 2004; 19:251–262. PMID:
15215323.

45. Burkey MD, Feirman S, Wang H, Choudhury SR, Grover S, Johnston FM. The association between smokeless tobacco use and pancreatic adenocarcinoma: a systematic review. Cancer Epidemiol. 2014; 38:647–653. PMID:
25262376.

46. Connolly GN, Alpert HR. Trends in the use of cigarettes and other tobacco products, 2000-2007. JAMA. 2008; 299:2629–2630. PMID:
18544722.

47. Bates C, Fagerström K, Jarvis MJ, Kunze M, McNeill A, Ramström L. European Union policy on smokeless tobacco: a statement in favour of evidence based regulation for public health. Tob Control. 2003; 12:360–367. PMID:
14660767.

48. Benowitz NL, Porchet H, Sheiner L, Jacob P 3rd. Nicotine absorption and cardiovascular effects with smokeless tobacco use: comparison with cigarettes and nicotine gum. Clin Pharmacol Ther. 1988; 44:23–28. PMID:
3391001.

49. Thomas G, Hashibe M, Jacob BJ, Ramadas K, Mathew B, Sankaranarayanan R, et al. Risk factors for multiple oral premalignant lesions. Int J Cancer. 2003; 107:285–291. PMID:
12949809.

50. Amagasa T, Yamashiro M, Uzawa N. Oral premalignant lesions: from a clinical perspective. Int J Clin Oncol. 2011; 16:5–14. PMID:
21225307.

51. Rodu B, Cole P. Smokeless tobacco use and cancer of the upper respiratory tract. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002; 93:511–515. PMID:
12075196.

52. Said TM, Ranga G, Agarwal A. Relationship between semen quality and tobacco chewing in men undergoing infertility evaluation. Fertil Steril. 2005; 84:649–653. PMID:
16169398.

53. Sunanda P, Panda B, Dash C, Ray PK, Padhy RN, Routray P. Prevalence of abnormal spermatozoa in tobacco chewing sub-fertile males. J Hum Reprod Sci. 2014; 7:136–142. PMID:
25191028.

54. Stead LF, Perera R, Bullen C, Mant D, Hartmann-Boyce J, Cahill K, et al. Nicotine replacement therapy for smoking cessation. Cochrane Database Syst Rev. 2012; 11:CD000146. PMID:
23152200.

55. Joseph AM, Fu SS. Safety issues in pharmacotherapy for smoking in patients with cardiovascular disease. Prog Cardiovasc Dis. 2003; 45:429–441. PMID:
12800126.

56. Greenland S, Satterfield MH, Lanes SF. A meta-analysis to assess the incidence of adverse effects associated with the transdermal nicotine patch. Drug Saf. 1998; 18:297–308. PMID:
9565740.

57. Cooper S, Taggar J, Lewis S, Marlow N, Dickinson A, Whitemore R, et al. Effect of nicotine patches in pregnancy on infant and maternal outcomes at 2 years: follow-up from the randomised, double-blind, placebo-controlled SNAP trial. Lancet Respir Med. 2014; 2:728–737. PMID:
25127405.

58. Osser S, Beckman-Ramirez A, Liedholm P. Semen quality of smoking and non-smoking men in infertile couples in a Swedish population. Acta Obstet Gynecol Scand. 1992; 71:215–218. PMID:
1317645.

59. Chia SE, Tay SK, Lim ST. What constitutes a normal seminal analysis? Semen parameters of 243 fertile men. Hum Reprod. 1998; 13:3394–3398. PMID:
9886521.

60. Dikshit RK, Buch JG, Mansuri SM. Effect of tobacco consumption on semen quality of a population of hypofertile males. Fertil Steril. 1987; 48:334–336. PMID:
3609347.
61. Dunphy BC, Barratt CL, von Tongelen BP, Cooke ID. Male cigarette smoking and fecundity in couples attending an infertility clinic. Andrologia. 1991; 23:223–225. PMID:
1741486.

62. Gerhard I, Lenhard K, Eggert-Kruse W, Runnebaum B. Clinical data which influence semen parameters in infertile men. Hum Reprod. 1992; 7:830–837. PMID:
1323572.

63. Hassa H, Yildirim A, Can C, Turgut M, Tanir HM, Senses T, et al. Effect of smoking on semen parameters of men attending an infertility clinic. Clin Exp Obstet Gynecol. 2006; 33:19–22. PMID:
16761532.
64. Jeng HA, Chen YL, Kantaria KN. Association of cigarette smoking with reproductive hormone levels and semen quality in healthy adult men in Taiwan. J Environ Sci Health A Tox Hazard Subst Environ Eng. 2014; 49:262–268. PMID:
24279617.

65. Liu RZ, Gao JC, Zhang HG, Wang RX, Zhang ZH, Liu XY. Seminal plasma zinc level may be associated with the effect of cigarette smoking on sperm parameters. J Int Med Res. 2010; 38:923–928. PMID:
20819428.

66. Mak V, Jarvi K, Buckspan M, Freeman M, Hechter S, Zini A. Smoking is associated with the retention of cytoplasm by human spermatozoa. Urology. 2000; 56:463–466. PMID:
10962316.

67. Ochedalski T, Lachowicz-Ochedalska A, Dec W, Czechowski B. Evaluating the effect of smoking tobacco on some semen parameters in men of reproductive age. Ginekol Pol. 1994; 65:80–86. PMID:
8070715.
68. Oldereid NB, Rui H, Clausen OP, Purvis K. Cigarette smoking and human sperm quality assessed by laser-Doppler spectroscopy and DNA flow cytometry. J Reprod Fertil. 1989; 86:731–736. PMID:
2760898.

69. Sepaniak S, Forges T, Gerard H, Foliguet B, Bene MC, Monnier-Barbarino P. The influence of cigarette smoking on human sperm quality and DNA fragmentation. Toxicology. 2006; 223:54–60. PMID:
16621218.

70. Zavos PM, Correa JR, Antypas S, Zarmakoupis-Zavos PN, Zarmakoupis CN. Effects of seminal plasma from cigarette smokers on sperm viability and longevity. Fertil Steril. 1998; 69:425–429. PMID:
9531871.
71. Zhang JP, Meng QY, Wang Q, Zhang LJ, Mao YL, Sun ZX. Effect of smoking on semen quality of infertile men in Shandong, China. Asian J Androl. 2000; 2:143–146. PMID:
11232793.
72. Kiziler AR, Aydemir B, Onaran I, Alici B, Ozkara H, Gulyasar T, et al. High levels of cadmium and lead in seminal fluid and blood of smoking men are associated with high oxidative stress and damage in infertile subjects. Biol Trace Elem Res. 2007; 120:82–91. PMID:
17916958.

73. Shaarawy M, Mahmoud KZ. Endocrine profile and semen characteristics in male smokers. Fertil Steril. 1982; 38:255–257. PMID:
6809501.

74. Shen HM, Chia SE, Ni ZY, New AL, Lee BL, Ong CN. Detection of oxidative DNA damage in human sperm and the association with cigarette smoking. Reprod Toxicol. 1997; 11:675–680. PMID:
9311575.

75. Yu B, Qi Y, Liu D, Gao X, Chen H, Bai C, et al. Cigarette smoking is associated with abnormal histone-to-protamine transition in human sperm. Fertil Steril. 2014; 101:51–57. PMID:
24112532.

76. Taha EA, Ez-Aldin AM, Sayed SK, Ghandour NM, Mostafa T. Effect of smoking on sperm vitality, DNA integrity, seminal oxidative stress, zinc in fertile men. Urology. 2012; 80:822–825. PMID:
23021663.

77. Martini AC, Molina RI, Estofán D, Senestrari D, Fiol de Cuneo M, Ruiz RD. Effects of alcohol and cigarette consumption on human seminal quality. Fertil Steril. 2004; 82:374–377. PMID:
15302286.

78. Meri ZB, Irshid IB, Migdadi M, Irshid AB, Mhanna SA. Does cigarette smoking affect seminal fluid parameters? A comparative study. Oman Med J. 2013; 28:12–15. PMID:
23386938.

79. Pasqualotto FF, Sobreiro BP, Hallak J, Pasqualotto EB, Lucon AM. Cigarette smoking is related to a decrease in semen volume in a population of fertile men. BJU Int. 2006; 97:324–326. PMID:
16430638.

80. Ramlau-Hansen CH, Thulstrup AM, Aggerholm AS, Jensen MS, Toft G, Bonde JP. Is smoking a risk factor for decreased semen quality? A cross-sectional analysis. Hum Reprod. 2007; 22:188–196. PMID:
16966350.

81. Vine MF, Margolin BH, Morrison HI, Hulka BS. Cigarette smoking and sperm density: a meta-analysis. Fertil Steril. 1994; 61:35–43. PMID:
8293842.
82. Practice Committee of the American Society for Reproductive Medicine. Smoking and infertility: a committee opinion. Fertil Steril. 2012; 98:1400–1406. PMID:
22959451.
83. Vine MF. Smoking and male reproduction: a review. Int J Androl. 1996; 19:323–337. PMID:
9051418.

84. Gaur DS, Talekar M, Pathak VP. Effect of cigarette smoking on semen quality of infertile men. Singapore Med J. 2007; 48:119–123. PMID:
17304390.
85. Hassan MA, Killick SR. Negative lifestyle is associated with a significant reduction in fecundity. Fertil Steril. 2004; 81:384–392. PMID:
14967378.

86. Benowitz NL, Jacob P 3rd, Kozlowski LT, Yu L. Influence of smoking fewer cigarettes on exposure to tar, nicotine, and carbon monoxide. N Engl J Med. 1986; 315:1310–1313. PMID:
3773954.

87. Zavos PM, Correa JR, Karagounis CS, Ahparaki A, Phoroglou C, Hicks CL, et al. An electron microscope study of the axonemal ultrastructure in human spermatozoa from male smokers and nonsmokers. Fertil Steril. 1998; 69:430–434. PMID:
9531872.
88. Yeung CH, Tüttelmann F, Bergmann M, Nordhoff V, Vorona E, Cooper TG. Coiled sperm from infertile patients: characteristics, associated factors and biological implication. Hum Reprod. 2009; 24:1288–1295. PMID:
19221095.

89. Miyaji K, Kaneko S, Ishikawa H, Aoyagi T, Hayakawa K, Hata M, et al. Creatine kinase isoforms in the seminal plasma and the purified human sperm. Arch Androl. 2001; 46:127–134. PMID:
11297066.

90. Ghaffari MA, Rostami M. The effect of cigarette smoking on human sperm creatine kinase activity: as an ATP buffering system in sperm. Int J Fertil Steril. 2013; 6:258–265. PMID:
24520449.
91. Gerhard I, Fröhlich E, Eggert-Kruse W, Klinga K, Runnebaum B. Relationship of sperm acrosin activity to semen and clinical parameters in infertile patients. Andrologia. 1989; 21:146–154. PMID:
2712369.
92. El Mulla KF, Köhn FM, El Beheiry AH, Schill WB. The effect of smoking and varicocele on human sperm acrosin activity and acrosome reaction. Hum Reprod. 1995; 10:3190–3194. PMID:
8822441.
93. Sofikitis N, Takenaka M, Kanakas N, Papadopoulos H, Yamamoto Y, Drakakis P, et al. Effects of cotinine on sperm motility, membrane function, and fertilizing capacity in vitro. Urol Res. 2000; 28:370–375. PMID:
11221915.

94. Close CE, Roberts PL, Berger RE. Cigarettes, alcohol and marijuana are related to pyospermia in infertile men. J Urol. 1990; 144:900–903. PMID:
2398564.

95. La Maestra S, De Flora S, Micale RT. Effect of cigarette smoke on DNA damage, oxidative stress, and morphological alterations in mouse testis and spermatozoa. Int J Hyg Environ Health. 2015; 218:117–122. PMID:
25260855.

96. Sharma RK, Pasqualotto FF, Nelson DR, Thomas AJ Jr, Agarwal A. The reactive oxygen species-total antioxidant capacity score is a new measure of oxidative stress to predict male infertility. Hum Reprod. 1999; 14:2801–2807. PMID:
10548626.

97. Alvarez JG, Storey BT. Differential incorporation of fatty acids into and peroxidative loss of fatty acids from phospholipids of human spermatozoa. Mol Reprod Dev. 1995; 42:334–346. PMID:
8579848.

98. de Lamirande E, Gagnon C. Impact of reactive oxygen species on spermatozoa: a balancing act between beneficial and detrimental effects. Hum Reprod. 1995; 10(Suppl 1):15–21. PMID:
8592032.

99. Murphy MP, Holmgren A, Larsson NG, Halliwell B, Chang CJ, Kalyanaraman B, et al. Unraveling the biological roles of reactive oxygen species. Cell Metab. 2011; 13:361–366. PMID:
21459321.

100. Logan-Garbisch T, Bortolazzo A, Luu P, Ford A, Do D, Khodabakhshi P, et al. Developmental ethanol exposure leads to dysregulation of lipid metabolism and oxidative stress in Drosophila. G3 (Bethesda). 2014; 5:49–59. PMID:
25387828.

101. Cho DY, Le W, Bravo DT, Hwang PH, Illek B, Fischer H, et al. Air pollutants cause release of hydrogen peroxide and interleukin-8 in a human primary nasal tissue culture model. Int Forum Allergy Rhinol. 2014; 4:966–971. PMID:
25400124.

102. Agarwal A, Prabakaran SA. Mechanism, measurement, and prevention of oxidative stress in male reproductive physiology. Indian J Exp Biol. 2005; 43:963–974. PMID:
16315393.
103. Griveau JF, Le Lannou D. Reactive oxygen species and human spermatozoa: physiology and pathology. Int J Androl. 1997; 20:61–69. PMID:
9292315.

104. Shen HM, Chia SE, Ong CN. Evaluation of oxidative DNA damage in human sperm and its association with male infertility. J Androl. 1999; 20:718–723. PMID:
10591610.
105. Kim JG, Parthasarathy S. Oxidation and the spermatozoa. Semin Reprod Endocrinol. 1998; 16:235–239. PMID:
10101805.

106. Comhaire FH, Mahmoud AM, Depuydt CE, Zalata AA, Christophe AB. Mechanisms and effects of male genital tract infection on sperm quality and fertilizing potential: the andrologist's viewpoint. Hum Reprod Update. 1999; 5:393–398. PMID:
10582779.

107. Aitken RJ, Buckingham DW, Brindle J, Gomez E, Baker HW, Irvine DS. Analysis of sperm movement in relation to the oxidative stress created by leukocytes in washed sperm preparations and seminal plasma. Hum Reprod. 1995; 10:2061–2071. PMID:
8567843.
108. Stone KK, Bermúdez E, Pryor WA. Aqueous extracts of cigarette tar containing the tar free radical cause DNA nicks in mammalian cells. Environ Health Perspect. 1994; 102(Suppl 10):173–178. PMID:
7705294.

109. Iwasaki A, Gagnon C. Formation of reactive oxygen species in spermatozoa of infertile patients. Fertil Steril. 1992; 57:409–416. PMID:
1735495.
110. Alvarez JG, Storey BT. Role of glutathione peroxidase in protecting mammalian spermatozoa from loss of motility caused by spontaneous lipid peroxidation. Gamete Res. 1989; 23:77–90. PMID:
2545584.

111. Dawson EB, Harris WA, Teter MC, Powell LC. Effect of ascorbic acid supplementation on the sperm quality of smokers. Fertil Steril. 1992; 58:1034–1039. PMID:
1426355.
112. Smith JL, Hodges RE. Serum levels of vitamin C in relation to dietary and supplemental intake of vitamin C in smokers and nonsmokers. Ann N Y Acad Sci. 1987; 498:144–152. PMID:
3475996.

113. Dacheux JL, Dacheux F. New insights into epididymal function in relation to sperm maturation. Reproduction. 2013; 147:R27–R42. PMID:
24218627.

114. Bornman MS, Kok EL, du Plessis DJ, Otto BS. Clinical features of patients with detached ciliary tufts in semen. Andrologia. 1989; 21:18–22. PMID:
2712358.
115. Jarow JP. Effects of varicocele on male fertility. Hum Reprod Update. 2001; 7:59–64. PMID:
11212076.

116. Masson P, Brannigan RE. The varicocele. Urol Clin North Am. 2014; 41:129–144. PMID:
24286772.

117. Klaiber EL, Broverman DM, Pokoly TB, Albert AJ, Howard PJ Jr, Sherer JF Jr. Interrelationships of cigarette smoking, testicular varicoceles, and seminal fluid indexes. Fertil Steril. 1987; 47:481–486. PMID:
3556626.
118. Hiremagalur B, Sabban EL. Nicotine elicits changes in expression of adrenal catecholamine biosynthetic enzymes, neuropeptide Y and immediate early genes by injection but not continuous administration. Brain Res Mol Brain Res. 1995; 32:109–115. PMID:
7494448.

119. Polsky JY, Aronson KJ, Heaton JP, Adams MA. Smoking and other lifestyle factors in relation to erectile dysfunction. BJU Int. 2005; 96:1355–1359. PMID:
16287457.

120. Kupelian V, Link CL, McKinlay JB. Association between smoking, passive smoking, and erectile dysfunction: results from the Boston Area Community Health (BACH) Survey. Eur Urol. 2007; 52:416–422. PMID:
17383811.

121. Cao S, Yin X, Wang Y, Zhou H, Song F, Lu Z. Smoking and risk of erectile dysfunction: systematic review of observational studies with meta-analysis. PLoS One. 2013; 8:e60443. PMID:
23573257.

122. Maiorino MI, Bellastella G, Esposito K. Lifestyle modifications and erectile dysfunction: what can be expected? Asian J Androl. 2015; 17:5–10. PMID:
25248655.

123. Pourmand G, Alidaee MR, Rasuli S, Maleki A, Mehrsai A. Do cigarette smokers with erectile dysfunction benefit from stopping?: a prospective study. BJU Int. 2004; 94:1310–1313. PMID:
15610111.

124. O WS, Chen H, Chow PH. Male genital tract antioxidant enzymes--their ability to preserve sperm DNA integrity. Mol Cell Endocrinol. 2006; 250:80–83. PMID:
16442705.

125. Pakrashi A, Chatterjee S. Effect of tobacco consumption on the function of male accessory sex glands. Int J Androl. 1995; 18:232–236. PMID:
8567092.

126. Arabi M, Moshtaghi H. Influence of cigarette smoking on spermatozoa via seminal plasma. Andrologia. 2005; 37:119–124. PMID:
16164428.

127. Mehran A. The toxic effect of seminal plasma from smokers on sperm function in non-smokers. Zhonghua Nan Ke Xue. 2005; 11:647–651. PMID:
16209200.
128. Weisberg E. Smoking and reproductive health. Clin Reprod Fertil. 1985; 3:175–186. PMID:
3910212.
129. Ochedalski T, Lachowicz-Ochedalska A, Dec W, Czechowski B. Examining the effects of tobacco smoking on levels of certain hormones in serum of young men. Ginekol Pol. 1994; 65:87–93. PMID:
8070716.
130. Jurasović J, Cvitković P, Pizent A, Colak B, Telisman S. Semen quality and reproductive endocrine function with regard to blood cadmium in Croatian male subjects. Biometals. 2004; 17:735–743. PMID:
15689116.

131. Jensen JA, Goodson WH, Hopf HW, Hunt TK. Cigarette smoking decreases tissue oxygen. Arch Surg. 1991; 126:1131–1134. PMID:
1929845.

132. Perrin J, Tassistro V, Mandon M, Grillo JM, Botta A, Sari-Minodier I. Tobacco consumption and benzo(a)pyrene-diol-epoxide-DNA adducts in spermatozoa: in smokers, swim-up procedure selects spermatozoa with decreased DNA damage. Fertil Steril. 2011; 95:2013–2017. PMID:
21406302.

133. Phillips DH, Venitt S. DNA and protein adducts in human tissues resulting from exposure to tobacco smoke. Int J Cancer. 2012; 131:2733–2753. PMID:
22961407.

134. Zenzes MT, Puy LA, Bielecki R, Reed TE. Detection of benzo[a]pyrene diol epoxide-DNA adducts in embryos from smoking couples: evidence for transmission by spermatozoa. Mol Hum Reprod. 1999; 5:125–131. PMID:
10065867.

135. Begum S. Molecular changes in smoking-related lung cancer. Expert Rev Mol Diagn. 2012; 12:93–106. PMID:
22133122.

136. Horak S, Polanska J, Widlak P. Bulky DNA adducts in human sperm: relationship with fertility, semen quality, smoking, and environmental factors. Mutat Res. 2003; 537:53–65. PMID:
12742507.

137. Gaspari L, Chang SS, Santella RM, Garte S, Pedotti P, Taioli E. Polycyclic aromatic hydrocarbon-DNA adducts in human sperm as a marker of DNA damage and infertility. Mutat Res. 2003; 535:155–160. PMID:
12581533.

138. Gallagher J, Mumford J, Li X, Shank T, Manchester D, Lewtas J. DNA adduct profiles and levels in placenta, blood and lung in relation to cigarette smoking and smoky coal emissions. IARC Sci Publ. 1993; (124):283–292. PMID:
8225497.
139. Trková M, Kapras J, Bobková K, Stanková J, Mejsnarová B. Increased micronuclei frequencies in couples with reproductive failure. Reprod Toxicol. 2000; 14:331–335. PMID:
10908836.

140. Lähdetie J. Micronucleated spermatids in the seminal fluid of smokers and nonsmokers. Mutat Res. 1986; 172:255–263. PMID:
3785273.

141. Fenech M. Micronuclei and their association with sperm abnormalities, infertility, pregnancy loss, pre-eclampsia and intra-uterine growth restriction in humans. Mutagenesis. 2011; 26:63–67. PMID:
21164184.

142. Papachristou F, Simopoulou M, Touloupidis S, Tsalikidis C, Sofikitis N, Lialiaris T. DNA damage and chromosomal aberrations in various types of male factor infertility. Fertil Steril. 2008; 90:1774–1781. PMID:
18082736.

143. El Ghamrasni S, Cardoso R, Halaby MJ, Zeegers D, Harding S, Kumareswaran R, et al. Cooperation of Blm and Mus81 in development, fertility, genomic integrity and cancer suppression. Oncogene. 2015; 34:1780–1789. PMID:
24858046.

144. Yarosh SL, Kokhtenko EV, Churnosov MI, Solodilova MA, Polonikov AV. Joint effect of glutathione S-transferase genotypes and cigarette smoking on idiopathic male infertility. Andrologia. 2015; 47:980–986. PMID:
25348056.

145. Yarosh SL, Kokhtenko EV, Churnosov MI, Ataman AV, Solodilova MA, Polonikov AV. Synergism between the N-acetyltransferase 2 gene and oxidant exposure increases the risk of idiopathic male infertility. Reprod Biomed Online. 2014; 29:362–369. PMID:
24928356.

146. Yarosh SL, Kokhtenko EV, Starodubova NI, Churnosov MI, Polonikov AV. Smoking status modifies the relation between CYP1A1*2C gene polymorphism and idiopathic male infertility: the importance of gene-environment interaction analysis for genetic studies of the disease. Reprod Sci. 2013; 20:1302–1307. PMID:
23548414.
147. Demirhan O, Demir C, Tunç E, nandıklıoğlu N, Sütcü E, Sadıkoğlu N, et al. The genotoxic effect of nicotine on chromosomes of human fetal cells: the first report described as an important study. Inhal Toxicol. 2011; 23:829–834. PMID:
22035122.

148. Hassold T, Hunt P. To err (meiotically) is human: the genesis of human aneuploidy. Nat Rev Genet. 2001; 2:280–291. PMID:
11283700.

149. Pereira CS, Juchniuk de Vozzi MS, Dos Santos SA, Vasconcelos MA, de Paz CC, Squire JA, et al. Smoking-induced chromosomal segregation anomalies identified by FISH analysis of sperm. Mol Cytogenet. 2014; 7:58. PMID:
25264457.

150. Boissonnas CC, Jouannet P, Jammes H. Epigenetic disorders and male subfertility. Fertil Steril. 2013; 99:624–631. PMID:
23714437.

151. Kotaja N. MicroRNAs and spermatogenesis. Fertil Steril. 2014; 101:1552–1562. PMID:
24882619.

152. Shenker NS, Ueland PM, Polidoro S, van Veldhoven K, Ricceri F, Brown R, et al. DNA methylation as a long-term biomarker of exposure to tobacco smoke. Epidemiology. 2013; 24:712–716. PMID:
23867811.

153. Joubert BR, Håberg SE, Nilsen RM, Wang X, Vollset SE, Murphy SK, et al. 450K epigenome-wide scan identifies differential DNA methylation in newborns related to maternal smoking during pregnancy. Environ Health Perspect. 2012; 120:1425–1431. PMID:
22851337.

154. Monick MM, Beach SR, Plume J, Sears R, Gerrard M, Brody GH, et al. Coordinated changes in AHRR methylation in lymphoblasts and pulmonary macrophages from smokers. Am J Med Genet B Neuropsychiatr Genet. 2012; 159B:141–151. PMID:
22232023.

155. Philibert RA, Beach SR, Brody GH. Demethylation of the aryl hydrocarbon receptor repressor as a biomarker for nascent smokers. Epigenetics. 2012; 7:1331–1338. PMID:
23070629.

156. Besingi W, Johansson A. Smoke-related DNA methylation changes in the etiology of human disease. Hum Mol Genet. 2014; 23:2290–2297. PMID:
24334605.

157. Fortes MR, Satake N, Corbet DH, Corbet NJ, Burns BM, Moore SS, et al. Sperm protamine deficiency correlates with sperm DNA damage in Bos indicus bulls. Andrology. 2014; 2:370–378. PMID:
24634207.
158. Hammadeh ME, Hamad MF, Montenarh M, Fischer-Hammadeh C. Protamine contents and P1/P2 ratio in human spermatozoa from smokers and non-smokers. Hum Reprod. 2010; 25:2708–2720. PMID:
20823111.

159. Marczylo EL, Amoako AA, Konje JC, Gant TW, Marczylo TH. Smoking induces differential miRNA expression in human spermatozoa: a potential transgenerational epigenetic concern? Epigenetics. 2012; 7:432–439. PMID:
22441141.

160. Yu B, Ding Q, Zheng T, Jiang L, Li Q, Sun X, et al. Smoking attenuated the association between IκBα rs696 polymorphism and defective spermatogenesis in humans. Andrologia. 2015; 47:987–994. PMID:
25352423.
161. Aston KI, Punj V, Liu L, Carrell DT. Genome-wide sperm deoxyribonucleic acid methylation is altered in some men with abnormal chromatin packaging or poor in vitro fertilization embryogenesis. Fertil Steril. 2012; 97:285–292. PMID:
22154369.
162. Oyeyipo IP, Raji Y, Emikpe BO, Bolarinwa AF. Effects of nicotine on sperm characteristics and fertility profile in adult male rats: a possible role of cessation. J Reprod Infertil. 2011; 12:201–207. PMID:
23926503.
163. Lotti F, Corona G, Vitale P, Maseroli E, Rossi M, Fino MG, et al. Current smoking is associated with lower seminal vesicles and ejaculate volume, despite higher testosterone levels, in male subjects of infertile couples. Hum Reprod. 2015; 30:590–602. PMID:
25567620.

164. Camacho EM, Huhtaniemi IT, O'Neill TW, Finn JD, Pye SR, Lee DM, et al. Age-associated changes in hypothalamic-pituitary-testicular function in middle-aged and older men are modified by weight change and lifestyle factors: longitudinal results from the European Male Ageing Study. Eur J Endocrinol. 2013; 168:445–455. PMID:
23425925.

165. Harte CB, Meston CM. Association between smoking cessation and sexual health in men. BJU Int. 2012; 109:888–896. PMID:
21883852.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download