Abstract
Purpose
This study was conducted to find the relative risk of semen abnormality with respect to smoking history and obesity.
Materials and Methods
Subfertile or infertile men were enrolled in this study from July 2010 to June 2011. All participants provided their cigarette use information, self-reported weight, height, semen analysis, physical examination, and sexually transmitted disease status. None of the enrolled patients had any specific pathological reason for infertility. Semen abnormality was defined as a condition in which one or more parameters did not satisfy the World Health Organization's criteria.
Results
A total of 1,073 male patients were considered for this study. After the application of the inclusion criteria, 193 patients were finally analyzed. These patients were divided into two groups according to semen abnormality: the normal semen group (n=72) and the abnormal semen group (n=121). Baseline characteristics, except age and smoking history, were not significantly different between the two groups. Smoking history and age were risk factors for the semen abnormality of idiopathic infertile male patients.
Go to : 
Cigarette smoking is a recognized health hazard and a major cause of various malignant diseases. In the case of women of reproductive age, cigarette smoking has a dose-related effect that can delay the time to conception [1]. In the case of male infertility, cigarette smoking has been reported to have a negative impact on sperm parameters [2]. Semen quality measures were significantly associated with the pregnancy rate, with the percentage of morphologically normal sperm, and with the total number of sperm showing a particularly strong association [3]. Smokers inhale a host of toxins, such as nicotine, carbon monoxide, cadmium, and other mutagenic compounds [4]. Smoking cigarettes may be associated with infertility in men and may damage the chromatin structure and produce endogenous DNA strand breaks in human sperm [5]. Cigarette smoking has been associated with adverse effects on semen quality, such as those on semen density, motility, and morphology [6,7]. Previous studies have suggested that semen quality may be greatly impacted by smoking [6,7,8,9].
In recent decades, the prevalence of obesity has doubled in the Western and the westernizing countries. In South Korea, according to the Korean National Health and Nutrition Examination Survey IV (KNHANES IV), obesity has increased gradually. There have been several studies on the relationship between obesity and male infertility. In a sperm function test, the hyaluronan binding of sperm and a high body mass index (BMI) had a negative effect on sperm quality and function [10]. Moreover, overweight men have a markedly changed sex hormone profile in serum, as well as a degradation of semen quality [11].
The aim of this study was to find the risk factors for semen abnormality. Further, we aimed to document semen abnormality depending on the smoking frequency and BMI.
Go to : 
A retrospective medical record study was conducted. Men visiting the hospital between July 2010 and June 2011 for subfertility or infertility were enrolled in this study. The Cheil General Hospital & Women's Healthcare Center Institutional Review Board approved the study. All participants provided their cigarette use information, self-reported weight and height to calculate their BMI, semen analysis and physical examination results, and history of sexually transmitted diseases. Semen samples were collected by masturbation following more than three days of abstinence. After liquefaction, a seminal analysis was performed according to the standard World Health Organization (WHO) criteria, a sperm concentration of >15× 106/mL, >4% morphologically normal cells, >40% motile sperm (categories 'a,' 'b,' and 'c'), and >58% alive sperm [12], and the sperm morphology was evaluated using Kruger's morphology criteria. If any single parameter did not satisfy these WHO criteria, we defined the case as an abnormality. The status of sexually transmitted diseases was evaluated via a polymerase chain reaction examination. Patients with infection, varicocele upon physical examination, or azoospermia, or those who submitted an incomplete questionnaire were excluded. None of the enrolled patients had any specific pathological reason for infertility. The questionnaire helped define the smoking amount per day and the smoking duration for the participants. Individuals were divided into two groups: the normal semen group and the abnormal semen group.
Patient characteristics are reported as mean±standard deviation unless otherwise indicated. A statistical analysis was performed with a paired t-test for normally distributed data and a Mann-Whitney U test for skewed data in order to evaluate the baseline characteristics. The correlation between two factors was analyzed by Pearson's or Spearman's rank correlation. The predictive risk factors were identified using binary logistic regression, odds ratio, and 95% confidence interval. A value of p<0.05 was considered statistically significant. For the statistical analysis, PASW Statistics version 18.0 (IBM Co., Armonk, NY, USA) was used.
Go to : 
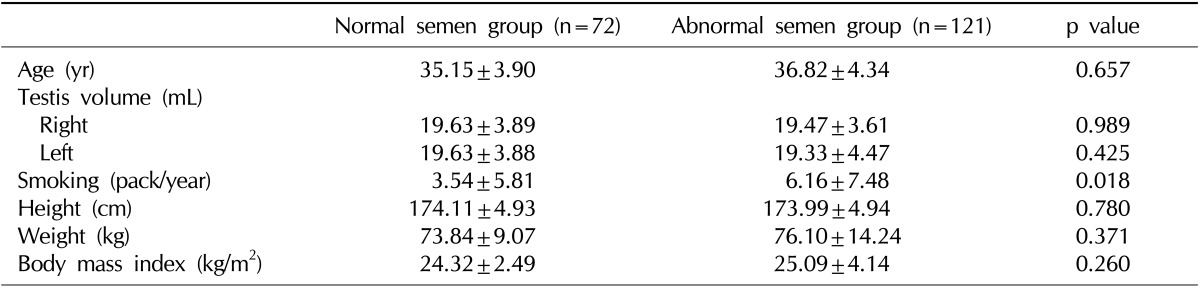
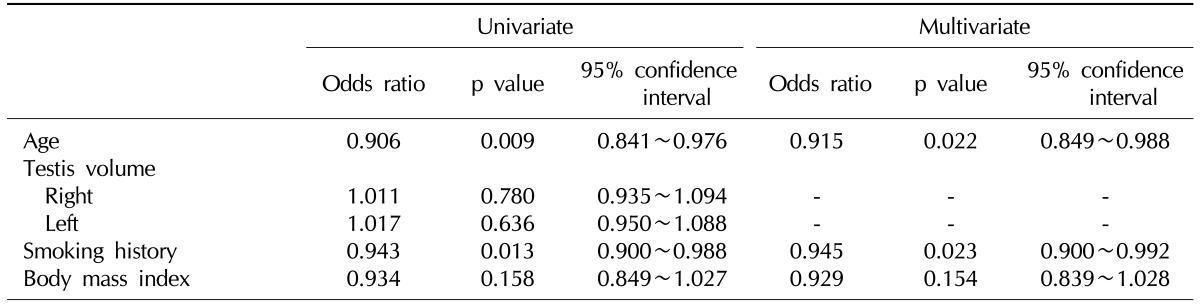
A total of 1,073 male patients were enrolled in this study. After the application of the inclusion criteria, 193 medical records of idiopathic infertile male patients were analyzed. Patients were divided into two groups according to semen abnormality: the normal semen group (n=72) and the abnormal semen group (n=121). Baseline characteristics, including testicular sizes and BMI, were not significantly different between the two groups, except smoking history (Table 1). Smoking and BMI did not statistically affect the semen parameters in the correlation test. Semen volume, sperm count, motility, viability, and morphology of all the subjects did not correlate with the smoking history or BMI. Table 2 shows the results of the analyses for the semen abnormality risk factors. Age and smoking history were found to be the risk factors for semen abnormality. Further, it was found that BMI did not significantly affect semen abnormality.
Go to : 
Various environmental materials may affect spermatogenesis, including toxins and medications. Numerous and widespread environmental chemicals may interfere with sexual hormone signaling in vitro and in vivo[13]. Cigarette smoke is known to be a somatic cell mutagen and a carcinogen. Toxic substances such as nicotine, carbon monoxide, benzo(a)pyrene, mutagenic pyrolysis-derived compounds, and cadmium can be absorbed during the inhalation of cigarette smoke. Toxic metabolites of cigarette smoke may impair spermatogenesis, resulting in the production of defective spermatozoa. Further, cigarette smoking is correlated with increased levels of seminal oxidative stress [14]. It appears that smoking is more likely to be associated with decreased semen quality in studies of healthy men. Among normal healthy men, smokers had about 24% lower sperm concentration than non-smokers. However, in a study of infertile male patients, smoking was not as closely associated with decreased semen quality [15].
Smoking is associated with sperm morphology, motility, and concentration. The average percentage reduction in the mean sperm concentration of smokers as compared to non-smokers was 13%. However, another study showed a different result. In healthy males, semen quality is more affected by smoking, and couples experiencing female factor infertility may be more affected by smoking than couples with only an infertile male. Among infertile male patients with poor semen quality, quitting smoking may improve the semen quality [15].
In this study, cigarette smoking was shown to be related to semen abnormality in idiopathic infertile male patients. However, there was no statistically significant correlation between smoking history and semen parameters. Moreover, age was a risk factor for semen abnormality. The sperm concentration of those smoking more than 20 cigarettes per day was lower than that of non-smokers [16]. Some studies have shown no significant difference in sperm concentration due to cigarette smoking. In fertile men and subfertile asthenozoospermic patients, there was no significant difference in the semen parameters [17]. In the case of semen morphology, some reports have shown that semen morphology correlated with smoking, while others have not. Although semen morphology was shown to be an important parameter related to pregnancy [3], the definition of abnormal sperm morphology was not consistent. In this study, all enrolled subjects had idiopathic infertility; this result does not agree to that of a previous study that compared fertile and infertile male patients.
A prior longitudinal study regarding the correlation of semen parameters and the pregnancy rate showed that morphologically normal sperm and sperm concentration affected the pregnancy rate [3]. In the present study, smokers represented only 6.0% of the study population, which did not effectively contribute to the overall analysis.
In South Korea, according to KNHANES IV data, the number of adult patients with severe obesity increased by about 1.5 times from 2.4% in 1998 to 3.9% in 2007~2009. Obesity affects gonadotropin-releasing hormone, which may impair Leydig and Sertoli cell functioning [18]. The conversion of androgens into estrogens in the adipose tissue may augment leptin production and depress pituitary gland function [19,20]. Moreover, being overweight was dose-dependently related to hormonal changes such as changes in the levels of testosterone and the sex hormone-binding globulin [11]. Overweight men had a slightly lower sperm concentration and total sperm count than normal-weight men [11,21]. However, in this study, BMI did not affect the abnormality of semen parameters.
In this study, there were a few limitations. In several previous studies, many confounders, which may affect semen parameters, were considered. However, in this retrospective study, other confounders were not considered. In addition, the hormonal status may differ according to body weight; we did not check the hormonal status of the patients. To overcome these limitations, we plan to conduct a well-designed prospective study in the near future.
Go to : 
In idiopathic infertile male patients, smoking and age may be the risk factors for semen abnormality. However, smoking and BMI did not correlate with semen parameters. Obesity did not affect the semen abnormality. Smoking adversely affects the semen quality and may play a negative role in conception. A more prospective and well-designed study is needed for establishing an accurate relationship between smoking and semen quality.
Go to : 
References
2. Marinelli D, Gaspari L, Pedotti P, Taioli E. Mini-review of studies on the effect of smoking and drinking habits on semen parameters. Int J Hyg Environ Health. 2004; 207:185–192. PMID: 15330386.

3. Zinaman MJ, Brown CC, Selevan SG, Clegg ED. Semen quality and human fertility: a prospective study with healthy couples. J Androl. 2000; 21:145–153. PMID: 10670528.
4. Zavos PM, Correa JR, Antypas S, Zarmakoupis-Zavos PN, Zarmakoupis CN. Effects of seminal plasma from cigarette smokers on sperm viability and longevity. Fertil Steril. 1998; 69:425–429. PMID: 9531871.
5. Zenzes MT. Smoking and reproduction: gene damage to human gametes and embryos. Hum Reprod Update. 2000; 6:122–131. PMID: 10782570.

6. Merino G, Lira SC, Martínez-Chéquer JC. Effects of cigarette smoking on semen characteristics of a population in Mexico. Arch Androl. 1998; 41:11–15. PMID: 9642454.

7. Zhang JP, Meng QY, Wang Q, Zhang LJ, Mao YL, Sun ZX. Effect of smoking on semen quality of infertile men in Shandong, China. Asian J Androl. 2000; 2:143–146. PMID: 11232793.
8. Al-Bader A, Omu AE, Dashti H. Chronic cadmium toxicity to sperm of heavy cigarette smokers: immunomodulation by zinc. Arch Androl. 1999; 43:135–140. PMID: 10543576.

9. Wang SL, Wang XR, Chia SE, Shen HM, Song L, Xing HX, et al. A study on occupational exposure to petrochemicals and smoking on seminal quality. J Androl. 2001; 22:73–78. PMID: 11191090.
10. Wegner CC, Clifford AL, Jilbert PM, Henry MA, Gentry WL. Abnormally high body mass index and tobacco use are associated with poor sperm quality as revealed by reduced sperm binding to hyaluronan-coated slides. Fertil Steril. 2010; 93:332–334. PMID: 19733846.
11. Aggerholm AS, Thulstrup AM, Toft G, Ramlau-Hansen CH, Bonde JP. Is overweight a risk factor for reduced semen quality and altered serum sex hormone profile? Fertil Steril. 2008; 90:619–626. PMID: 18068160.

12. Cooper TG, Noonan E, von Eckardstein S, Auger J, Baker HW, Behre HM, et al. World Health Organization reference values for human semen characteristics. Hum Reprod Update. 2010; 16:231–245. PMID: 19934213.

13. Toppari J. Environmental endocrine disrupters and disorders of sexual differentiation. Semin Reprod Med. 2002; 20:305–312. PMID: 12428210.

14. Saleh RA, Agarwal A, Sharma RK, Nelson DR, Thomas AJ Jr. Effect of cigarette smoking on levels of seminal oxidative stress in infertile men: a prospective study. Fertil Steril. 2002; 78:491–499. PMID: 12215323.

15. Vine MF. Smoking and male reproduction: a review. Int J Androl. 1996; 19:323–337. PMID: 9051418.

16. Ramlau-Hansen CH, Thulstrup AM, Aggerholm AS, Jensen MS, Toft G, Bonde JP. Is smoking a risk factor for decreased semen quality? A cross-sectional analysis. Hum Reprod. 2007; 22:188–196. PMID: 16966350.

17. de Jong AM, Menkveld R, Lens JW, Nienhuis SE, Rhemrev JP. Effect of alcohol intake and cigarette smoking on sperm parameters and pregnancy. Andrologia. 2014; 46:112–117. PMID: 23230969.

18. Vermeulen A. Environment, human reproduction, menopause, and andropause. Environ Health Perspect. 1993; 101(Suppl 2):91–100. PMID: 8243411.

19. Messinis IE, Milingos SD. Leptin in human reproduction. Hum Reprod Update. 1999; 5:52–63. PMID: 10333369.

20. Strain GW, Zumoff B, Kream J, Strain JJ, Deucher R, Rosenfeld RS, et al. Mild Hypogonadotropic hypogonadism in obese men. Metabolism. 1982; 31:871–875. PMID: 6811834.

21. Jensen TK, Andersson AM, Jørgensen N, Andersen AG, Carlsen E, Petersen JH, et al. Body mass index in relation to semen quality and reproductive hormones among 1,558 Danish men. Fertil Steril. 2004; 82:863–870. PMID: 15482761.
Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download