Abstract
Purpose
We analyzed factors associated with early recovery of continence after laparoscopic radical prostatectomy.
Materials and Methods
Among 467 patients treated with laparoscopic radical prostatectomy for localized prostate cancer between 2007 and 2012, 249 patients who underwent a preoperative urodynamic study were enrolled. The patients' age, prostate volume, preoperative serum prostate-specific antigen (PSA), Gleason score, pathologic stage, and preoperative urodynamic parameters were recorded. The preoperative membranous and prostatic urethral length on magnetic resonance image, nerve sparing technique, and type of surgical procedure (extrafascial and intrafascial) were analyzed. Patients were considered to have early recovery of continence when they needed no pad in 3 months or less after surgery.
Results
Ninety-two patients were in the early recovery group and 157 were in the late recovery group. The membranous urethral lengths were 12.06±2.56 and 11.81±2.87 mm, and prostatic urethral lengths were 36.39±6.15 and 37.45±7.55 mm in each group, respectively. The membranous-posterior urethral length ratios were 0.25±0.06 and 0.24±0.06, and prostatic-posterior urethral length ratios were 0.75±0.06 and 0.76±0.06, respectively. In and of themselves, the membranous and prostatic urethral lengths were not associated with recovery duration however, the membranous-total and prostatic-total urethral length ratios were related (p=0.024 and 0.024, respectively). None of the urodynamic parameters correlated with continence recovery time. In the multivariate analysis, the type of surgical procedure (odds ratio [OR], 7.032; 95% confidence interval [CI], 2.660 to 18.590; p<0.001) and membranous urethral length (OR, 0.845; 95% CI, 0.766 to 0.931; p=0.001) were significantly related to early recovery of continence.
Laparoscopic radical prostatectomy is currently a common surgical option for localized prostate cancer. Improvements in laparoscopic equipment and surgical techniques have led to lower morbidity and postoperative complication rates.1 However, several complications affect postoperative quality of life; in particular, incontinence is one of the complications with the greatest impact.
The reported rates of urinary incontinence after radical prostatectomy range from 2.5% to 87.0%, and differ considerably according to its definition, follow-up duration, and surgical technique.2-4 However, recent studies reported faster recovery of continence after radical prostatectomy, with up to 95% of patients reported as continent 1 year postoperatively.5 These results are similar to those obtained from laparoscopic radical prostatectomy a meta-analysis showed that continence rates 1 year after laparoscopic radical prostatectomy range from 60% to 97%.2
As the cause of incontinence after radical prostatectomy remains unclear, many studies have been performed to clarify the factors that affect continence recovery duration after surgery.6-9 For this purpose, we considered various factors that might be related to continence including surgical technique, urodynamic parameters, and urethral length.
Among those factors, we analyzed the effect of preoperative bladder function, urethral length, and surgical procedure on continence recovery duration after laparoscopic radical prostatectomy.
In total, 467 patients underwent laparoscopic radical prostatectomy for localized prostate cancer between January 2007 and March 2012. Of these patients, 249 cases who underwent a preoperative urodynamic study were reviewed. An extraperitoneal approach was used in all of the patients and no urethral enhancement techniques were used.
Each patient was interviewed regarding his incontinence status in our outpatient clinic every month. They were asked how many pads they used per day for incontinence. The patients were considered to have achieved recovery of continence when they needed no pad. Patients whose continence recovery duration was in 3 months or less were classified into the 'early recovery' group, whereas the remaining patients were classified into the 'late recovery' group.
Age, prostate volume, preoperative serum prostate-specific antigen (PSA), Gleason score, and pathologic stage were recorded for each patient. The membranous and prostatic urethral lengths were measured during preoperative magnetic resonance image (MRI), and the ratio of the membranous and prostatic urethral length to the posterior urethral length was calculated. Preoperative urodynamic parameters including maximal cystometric capacity (MCC), compliance, and maximal detrusor pressure were recorded. Methods of neurovascular bundle sparing were recorded as none, unilateral, and bilateral. The effect of the surgical procedure type was also analyzed. This study has been conducted under approval of Pusan National University Hospital clinical trial (PNUH: IRB-E-2013009).
All urodynamic evaluations were performed using a Dantec urodynamic testing system (Medtronic Dantec, Tonsbakken, Denmark). Cystometry was performed using an 8 F double lumen catheter with 37℃ normal saline solution at a filling rate of 50 ml/min, with abdominal pressure monitoring. Intra-abdominal pressure was measured using a pressure sensor attached to a water-filled balloon catheter that was passed into the patient's rectum. Detrusor pressure was estimated by subtracting the intra-abdominal pressure from the intravesical pressure. Using cystometry, MCC was defined as the bladder volume at which a patient had a strong desire to void. Maximal detrusor pressure was defined as the detrusor pressure at MCC. Compliance was calculated as volume change/pressure change during bladder filling.
MRI was performed on a 1.5 Tesla MRI system (Magnetom Symphony; Siemens, Erlangen, Germany). T2 coronal images were used. The membranous urethral length was measured as the distance from the prostatic apex to the entry of the urethra into the penile bulb. The prostatic urethral length was measured as the distance from the prostatic apex to the bladder neck. The posterior urethral length was the sum of the membranous and prostatic urethral lengths. The membranous-posterior and prostatic-posterior urethral length ratios were calculated as the membranous urethral length/posterior urethral length and prostatic urethral length/posterior urethral length, respectively.
Although the classical description of the neurovascular bundles is that of two bundles of tissue that are located near the posterolateral surface of the prostate,10 accumulating evidence indicates that this complex exhibits a certain amount of variability. Previously, we incised the endopelvic fascia lateral to the arcus tendinosus with sparing of both neurovascular bundles. In some patients, the cavernosal nerves form lattices or curtains that extend from the posterolateral to the anterolateral surface of the prostate, rather than distinct neurovascular bundles.11,12 To preserve these nerves, some surgeons use a special technique for sparing the 'veil of Aphrodite'.
In the present study, laparoscopic sparing of the veil of Aphrodite was performed using cold scissors. A bilateral incision of the periprostatic fascia was made medial to the puboprostatic ligament and directed to the base of the prostate. All lateral periprostatic fascia, endopelvic fascia, and puboprostatic fascia were maintained intact. This maneuver is important to skeletonize the urethra and to ensure the existence of the prostatic apical margin. The puboprostatic ligament and arcus tendinosus can be preserved using this approach. We compared the postoperative urinary continence recovery ability associated with the previous and current procedures.
T-tests were used to examine the relationship between each parameter, with the exception of the pathologic stage, neurovascular bundle sparing, and surgical procedure. Chi-squared tests were used to examine the differences in the pathologic stage, neurovascular bundle sparing, and surgical procedure between the early and late recovery groups. The age-adjusted partial correlation coefficients were used to calculate the correlation between the continence recovery duration and the other factors. Multivariate analysis was performed using logistic regression by including the parameters that were significant in the partial correlation analysis. A p<0.05 was considered significant. All of the analyses were performed using IBM SPSS Statistics version 19.0 (SPSS Inc., Chicago, IL, USA).
Among the 249 patients analyzed, 92 patients were classified into the early recovery group and 157 were classified into the late recovery group.
In each group, the mean ages of the patients were 66.05±6.23 (49~78) years and 66.40±6.24 (52~80) years, respectively. The prostate volumes were 34.74±13.92 (13.00~79.10) g and 36.09±14.78 (16.00~101.00) g, respectively. The serum PSA values were 12.79±15.12 (0.84~83.66) ng/ml and 13.43±13.99 (1.42~89.94) ng/ml, respectively. The Gleason scores were 6.76±0.95 (6~10) and 6.74±0.89 (5~10), respectively. In the early recovery group, pathologic stages T1, T2, and T3 were 3, 75, and 14, respectively. In the late recovery group, pathologic stages T1, T2, and T3 were 7, 114, and 36, respectively. The age, prostate volume, PSA, Gleason score, and pathologic stage of the two groups were not significantly different (p=0.997, p=0.877, p=0.728, p=0.711, and p=0.654, respectively).
In the early and late recovery groups, the mean membranous urethral lengths were 12.06±2.56 (5.63~19.72) mm and 11.81±2.87 (6.21~20.45) mm, respectively, and the mean prostatic urethral lengths were 36.39±6.15 (25.26~51.54) mm and 37.45±7.55 (20.14~66.00) mm, respectively. The mean posterior urethral lengths were 50.50±6.91 (33.00~75.00) mm and 49.26±7.43 (30.82~77.74) mm, respectively. The membranous-posterior urethral length ratios were 0.25±0.06 (0.11~0.44) and 0.24±0.06 (0.12~0.41), respectively. The prostatic-posterior urethral length ratios were 0.75±0.06 (0.56~0.89) and 0.76±0.06 (0.59~0.88), respectively. While the membranous, prostatic, and posterior urethral lengths were not correlated with continence recovery duration (p=0.206, p=0.177, and p=0.823, respectively), the membranous-posterior and prostatic-posterior urethral length ratios were associated with continence recovery duration (p=0.024 and p=0.024, respectively).
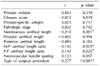
The preoperative urodynamic study in the early and late recovery groups revealed that the mean maximal cystometric capacities were 401.83±128.48 (161~688) ml and 376.41±126.73 (106~673) ml, respectively. The mean compliances were 63.23±63.98 (1.68~407.00) ml/cmH2O and 51.14±45.19 (2.50~334.50) ml/cmH2O, respectively. The mean maximal detrusor pressures were 65.38±19.68 (39~142) cmH2O and 60.66±25.98 (18~172) cmH2O, respectively. None of these urodynamic parameters was associated with continence recovery duration (p=0.629, p=0.307, and p=0.138, respectively) (Table 1).
No sparing technique, and unilateral and bilateral neurovascular bundle sparing surgery were performed in 25, 27, and 40 patients in the early recovery group, and in 70, 27, and 60 patients in the late recovery group, respectively. The neurovascular bundle sparing techniques were not related to the continence recovery duration (p=0.051). In the early recovery group, the previous extrafascial surgical procedure was applied to 73 patients, and the current intrafascial procedure was applied to 19 patients. In the late recovery group, the previous extrafascial procedure was applied to 151 patients and the current intrafascial procedure was applied to 6 patients. The type of surgical procedure affected continence recovery duration (p<0.001) (Table 2).
In partial correlation analysis adjusted by age, the type of surgical procedure, membranous urethral length, and membranous-posterior urethral length ratio correlated negatively with continence recovery duration (r=-0.277, r=-0.213, and r=-0.142, respectively) prostatic-posterior urethral length ratio correlated positively (r=0.142). The other factors were not related to the continence recovery duration (Table 3).
In the multivariate analysis, which included the type of surgical procedure, membranous urethral length, membranous-posterior and prostatic-posterior urethral length ratios, the type of surgical procedure (odds ratio [OR], 7.032; 95% confidence interval [CI], 2.660 to 18.590; p<0.001), and the membranous urethral length (OR, 0.845; 95% CI, 0.766 to 0.931; p=0.001) were significantly related to early recovery of continence (Table 4).
The purpose of this study was to analyze the effects of urethral length, urodynamic parameters, and modified surgical procedures on continence recovery duration after laparoscopic radical prostatectomy.
The patients were divided into two groups - the early and late recovery groups - according to the continence recovery duration. Although we defined continence recovery strictly as 'needing no pad', all of the patients recovered continence in less than 1 year after the surgery. In recent studies, the incontinence rate 1 year after surgery was reported to be 5%, or even as low as 1~2%.13,14 Thus, the 'late recovery 'group was conveniently named for comparison with the 'early recovery' group, which did not mean that continence recovery was morbidly delayed.
Although the neuroanatomy of continence has been incompletely characterized, some studies have reported that neurovascular bundle resection resulted in delayed continence recovery after radical prostatectomy.11,12,15 Those studies were based on the concept that the distal urethral sphincter is innervated by the autonomic (by the pelvic nerve) and somatic (by the pudendal nerve) nervous systems.15
In this study, the outcomes did not differ significantly between the two groups according to the neurovascular bundle sparing technique. However, the multivariate analysis showed that the type of surgical procedure was the most important factor, and compared to the extrafascial surgical procedure, the intrafascial surgical procedure reduced the continence recovery duration. Use of the current intrafascial surgical procedure to preserve the puboprostatic ligament and arcus tendinosus were shown to be related to early continence recovery. In addition, we suggest that the intrafascial surgical procedure can preserve more neurovascular bundles, which were not easily spared by the extrafascial surgical procedure. This suggests that good preservation of the structures surrounding the prostate is critical to reducing the duration of postprostatectomy incontinence.
It has been thought that the urethra is deeply involved in incontinence because of the existence of the urethral sphincters. Coakley et al8 reported that the duration of recovery of continence decreased as the membranous urethral length measured on MRI increased. Another study reported that the prostatic urethral length measured by transrectal ultrasonography exhibited a positive relationship with continence recovery duration.13 Some authors have proposed a modified technique for full functional-length sphincter preservation that increased early continence recovery.14 Others have reported that early continence recovery was related to a long membranous urethra.8,16 Conversely, Borin et al15 reported that aggressive resection of the urethra during robot-assisted laparoscopic prostatectomy did not affect continence and allowed a reduction of the surgical margin-positive rate.
In this study, the continence recovery duration decreased with the increase in the membranous urethral length. Although the critical urethral length that influences postprostatectomy incontinence has not been established, we suggest that preservation of the membranous urethra during prostatectomy is considered important for sphincter preservation related to continence.
The bladder is one of the most important organs affecting incontinence; thus, the effect of preoperative bladder function was analyzed. Kleinhans et al16 estimated the urodynamic changes associated with radical retropubic prostatectomy. Those authors reported that postoperative incontinence could not be predicted by parameters representing preoperative bladder function, whereas it was influenced by sphincteric deficiency as expressed by reduced pressures in the sphincteric mechanism.
However, very few studies have analyzed the relationship between preoperative urodynamic parameters and continence recovery. The preoperative urodynamic study performed here revealed that MCC, compliance, and maximal detrusor pressure were not related to early recovery. This result suggests that the bladder has a lesser effect on continence recovery because the detrusor muscles are not injured during surgery. In contrast, another study that addressed urodynamic changes before and after prostatectomy reported that bladder denervation is one of the factors affecting stress incontinence after surgery.17
A limitation of this study is that urethral sphincteric pressure was not analyzed, although it has been suggested to be an important urodynamic parameter associated with incontinence. Several studies have investigated the effect of urethral sphincteric pressure on incontinence.
Another limitation is that the patient number undergoing the current intrafascial surgical procedure was small. Although significant relationships were observed, reports from further surgical experience are needed to strengthen the findings and conclusions.
Nevertheless, it is meaningful that this study analyzed the relationship between continence recovery duration after laparoscopic radical prostatectomy and preoperative factors that are rarely analyzed.
In this study, the result of the multivariate analysis leads us to conclude that the current intrafascial surgical procedure is the most important factor affecting early recovery of continence after laparoscopic radical prostatectomy. In addition, a high membranous urethral length is related to a shortened duration for continence recovery after laparoscopic radical prostatectomy.
We can predict the results of laparoscopic radical prostatectomy and reduce the duration of incontinence based on these conclusions. Further studies are needed to confirm the ability of the modified current surgical procedure to reduce the continence recovery duration after laparoscopic radical prostatectomy.
Figures and Tables
Table 2
Patient distribution of the neurovascular bundle sparing technique and the type of surgical procedure between the early and late recovery group

References
1. So BK, Choi JD, Lee SY, Kim HS, Park SY, Seo SI. Experience of 100 laparoscopic radical prostatectomies performed by a single surgeon: an analysis of surgical and functional outcomes. Korean J Urol. 2011; 52:517–523.

2. Rassweiler J, Schulze M, Teber D, Seemann O, Frede T. Laparoscopic radical prostatectomy: functional and oncological outcomes. Curr Opin Urol. 2004; 14:75–82.

3. Steiner MS, Morton RA, Walsh PC. Impact of anatomical radical prostatectomy on urinary continence. J Urol. 1991; 145:512–514.

4. Hammerer P, Huland H. Urodynamic evaluation of changes in urinary control after radical retropubic prostatectomy. J Urol. 1997; 157:233–236.

5. Lepor H, Kaci L, Xue X. Continence following radical retropubic prostatectomy using self-reporting instruments. J Urol. 2004; 171:1212–1215.

6. Gacci M, Carini M, Simonato A, Imbimbo C, Gontero P, Briganti A, et al. Factors predicting continence recovery 1 month after radical prostatectomy: results of a multicenter survey. Int J Urol. 2011; 18:700–708.
7. Majoros A, Bach D, Keszthelyi A, Hamvas A, Romics I. Urinary incontinence and voiding dysfunction after radical retropubic prostatectomy (prospective urodynamic study). Neurourol Urodyn. 2006; 25:2–7.

8. Coakley FV, Eberhardt S, Kattan MW, Wei DC, Scardino PT, Hricak H. Urinary continence after radical retropubic prostatectomy: relationship with membranous urethral length on preoperative endorectal magnetic resonance imaging. J Urol. 2002; 168:1032–1035.

9. Hwang JJ, Kim BY, Uchio EM. Improving urinary continence after radical prostatectomy: review of surgical modifications. Korean J Urol. 2009; 50:935–941.

10. Narayan P, Konety B, Aslam K, Aboseif S, Blumenfeld W, Tanagho E. Neuroanatomy of the external urethral sphincter: implications for urinary continence preservation during radical prostate surgery. J Urol. 1995; 153:337–341.

11. Eastham JA, Kattan MW, Rogers E, Goad JR, Ohori M, Boone TB, et al. Risk factors for urinary incontinence after radical prostatectomy. J Urol. 1996; 156:1707–1713.

12. Wei JT, Dunn RL, Marcovich R, Montie JE, Sanda MG. Prospective assessment of patient reported urinary continence after radical prostatectomy. J Urol. 2000; 164:744–748.

13. Oefelein MG. Prospective predictors of urinary continence after anatomical radical retropubic prostatectomy: a multivariate analysis. World J Urol. 2004; 22:267–271.

14. Schlomm T, Heinzer H, Steuber T, Salomon G, Engel O, Michl U, et al. Full functional-length urethral sphincter preservation during radical prostatectomy. Eur Urol. 2011; 60:320–329.

15. Borin JF, Skarecky DW, Narula N, Ahlering TE. Impact of urethral stump length on continence and positive surgical margins in robot-assisted laparoscopic prostatectomy. Urology. 2007; 70:173–177.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download