Abstract
Purpose
There is little data evaluating the changes of severity of bladder outlet obstruction after 80 W-potassium-titanyl-phosphate (KTP) photoselective laser vaporization prostatectomy (PVP) by pressure-flow study. We evaluated the efficacy of PVP to relieve the obstruction in benign prostate hyperplasia (BPH) compared with transurethral resection of the prostate (TURP).
Materials and Methods
This is a prospective, non-randomized single center study. The inclusion criteria were as follows: Men suffering from lower urinary tract symptoms (LUTS) secondary to BPH, age ≥50 years, International Prostatic Symptom Score (IPSS) ≥13, maximum flow rate (Qmax) ≤15 ml/s, and ability to give fully informed consent. Patients with neurogenic cause or detrusor underactivity were excluded. The IPSS, bother score, Qmax, postvoid residual volume (PVR), detrusor pressure at maximum flow rate (PdetQmax), bladder outlet obstruction index (BOOI), and prostate volume were measured before and 6 months after surgery and compared between PVP and TURP.
Results
Sixty-seven patients (53 in PVP, 14 in TURP) were evaluable. In both groups, the IPSS, bother score, Qmax, and PVR had significantly improved (p<0.05), and there were no differences between the changes in those parameters. PVP could effectively reduce the PdetQmax, prostate volume, and BOOI from baseline (from 68.7±23.3 to 40.6±11.2 cmH2O, 49.5±16.3 to 31.3±12.1 ml, 49.8±25.6 to 9.8±20.7), similar to TURP. There were no differences in postoperative PdetQmax, prostate volume, or BOOI between the two groups. The percentage of patients with BOOI ≥40 was decreased from 64% to 4% in the PVP group and from 86% to 14% in the TURP group.
Transurethral resection of the prostate (TURP) has been considered to be the gold standard for the treatment of lower urinary tract symptoms (LUTS) secondary to benign prostate hyperplasia (BPH) (LUTS/BPH). However, because of its relatively high morbidity, long hospital stay, and catheter time, various minimally invasive alternatives have been introduced. Among the alternative surgical options, photoselective laser vaporization of the prostate (PVP) using a potassium-titanyl-phosphate (KTP) laser has shown promising clinical outcomes in terms of efficacy and safety.1-3 A high power KTP laser of 80 watts is able to evaporate tissue instantly and create a large cavity like TURP.4 The favorable efficacy of PVP seems to be due to the complete and effective removal of obstructing tissue and the reduction of the bladder outlet obstruction. However, there is little data evaluating the changes in the severity of bladder outlet obstruction after PVP by pressure-flow study (PFS), and there is no published data comparing the PFS results of PVP with TURP. In this nonrandomized study, we investigated the efficacy of PVP using a 80 watt KTP laser to reduce the volume of the prostate and decrease the severity of obstruction with reference to a TURP-treated control group and reviewed the relevant literature.
In July 2004, we started with a prospective, single center study to evaluate the surgical outcomes of PVP. The inclusion criteria were as follows: Men suffering from LUTS secondary to BPH, age ≥50 years, International Prostatic Symptom Score (IPSS) ≥13, maximum flow rate (Qmax) ≤15 ml/s, prostate volume ≥30 ml and ≤100 ml on transrectal ultrasounds (TRUS), and ability to give fully informed consent. Patients with voiding dysfunction with a suspected neurogenic cause, detrusor underactivity, urethral structure, acute urinary tract infection, chronic urinary retention, and known or suspected prostate cancer were excluded. Patients who did not agree with the protocol of this study were also excluded. To compare the surgical outcomes of PVP, we also enrolled patients who underwent TURP for the same study duration with the same inclusion and exclusion criteria. Approval was obtained from the institutional ethics committee before beginning the study. This study is registered on the ClinicalTrials.gov website with registration identification number - NCT009 08427. The URL is http://www.clinicaltrials.gov.
All patients underwent a urological evaluation that included medical history taking, pelvic examination including digital rectal examinations, neurourologic examinations, urinalysis, urine culture, serum prostate specific antigen (PSA), TRUS to estimate the prostate volume, and urodynamic studies including PFS. Urodynamic studies were performed according to the recommendations of the International Continence Society.5 The urodynamic parameters such as Qmax and detrusor pressure at Qmax (PdetQmax) were obtained. With these parameters, the bladder outlet obstruction index (BOOI) was estimated by the equation: [BOOI]=[PdetQmax] 2×[Qmax].6 Because the ablated volume of the prostate cannot be measured directly after PVP, we estimated the removed volume of tissue by the preoperative and postoperative TRUS.
All operative procedures were performed by a single surgeon (LSW) who had experience of more than 700 cases of TURP. The PVP was performed under monitoring with intravenous sedatives and TURP was performed under spinal anesthesia. The PVP was performed using an 80 W KTP laser using a GreenLight system (GreenLight PV™; Laserscope®, San Jose, CA, USA). The laser was delivered through a 600 µm side-deflecting fiber. A standard 23 Fr continuous flow resectoscope with a laser bridge was used for the procedure and sterile 0.9% saline solution was used for irrigation. A single fiber was used for each procedure. TURP was performed according to a standard technique using a 26 Fr continuous flow resectoscope, as it is described in general textbooks. The resection was carried out by a standard tungsten wire loop with a cutting current of 120 W and a coagulating current of 80 W. PVP was routinely performed in the day-surgery center and TURP was performed under hospitalization. The urethral catheter was removed on the first postoperative day in the PVP group and on the day when the urine became sufficiently clear in the TURP group. In all of the patients, 14-day postoperative antibiotic prophylaxis was prescribed.
After 6 months of follow up, all of the patients were evaluated by the IPSS, bother score, Qmax, and post-void residual volume (PVR). TRUS and PFS were also repeated. The IPSS, bother score, Qmax, PVR, PdetQmax, BOOI, Schafer obstruction grade, and prostate volume were compared before and 6 months after operation in the PVP and TURP groups. The complications associated with the operations were also investigated.
Statistical analyses were performed using the paired t-test for normally distributed data and using the Wilcoxon signed-ranks test for skewed data to compare pre- to post-treatment changes in the following: IPSS, bother score, Qmax, PVR, PdetQmax, BOOI, Schafer grade, and prostate volume. The Student's t-test was used to compare the results of the two groups at presentation and the differences between them when the data was normally distributed, and the Mann-Whitney test was used to analyze skewed data. p values of <0.05 were considered statistically significant.
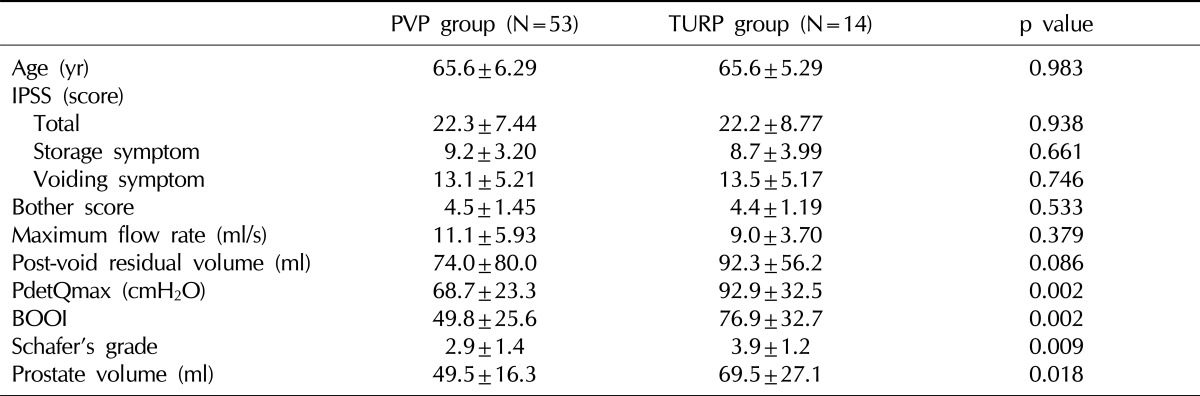
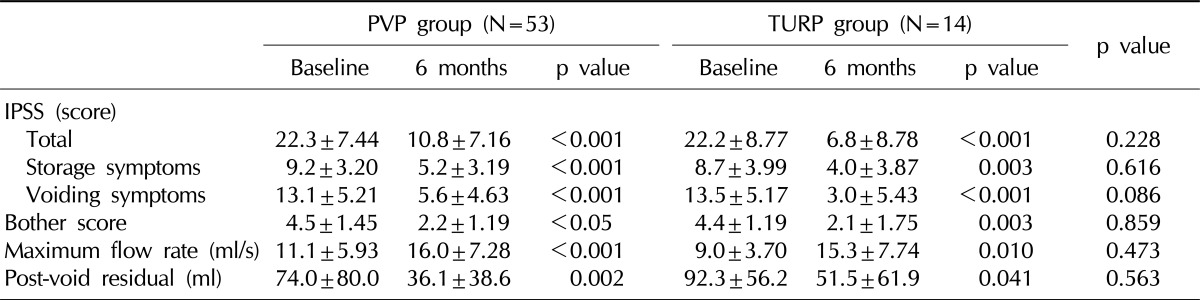
Of the 86 patients (66 in PVP, 20 in TURP) who were enrolled, 53 patients in the PVP group and 14 in the TURP group were evaluable at least 6 months postoperatively. Table 1 shows the baseline characteristics of the patients who underwent PVP and TURP. Preoperative age, IPSS including voiding and storage subscore, bother score, Qmax, and PVR did not differ between the two groups. However, the PdetQmax, BOOI, Schafer grade, and prostate volume were higher in the TURP group than the PVP group (Table 1). The IPSS, bother score, Qmax, and PVR were significantly improved after PVP, and the changes were comparable to TURP in our series (Table 2). After PVP, the prostate volume was effectively decreased from 50.3 to 31.3 ml and the BOOI (from 49.8 to 9.8) and Schafer grade (from 2.9 to 1.2) were markedly reduced. The PdetQmax was much decreased (from to 68.7 to 40.6 cmH2O) as well. the TURP groups also showed similar changes (Fig. 1). At 6 months of follow up, the postoperative prostate volume (31.3 vs. 34.1 ml), PdetQmax (40.6 vs. 51.5 cmH2O), and BOOI (9.8 vs. 18.6) and Schafer grade (1.2 vs. 1.5) did not significantly differ between the two groups (p=0.465, p=0.060, p=0.767, p=0.236, respectively). In the PVP group, the percentage of patients who had BOOI ≥40 was 64% before the operation and decreased to just 4% at 6 months of follow up. In the TURP group, the percentage of patients with a BOOI <40 was 86% before surgery and decreased to 14% at 6 months of follow up.
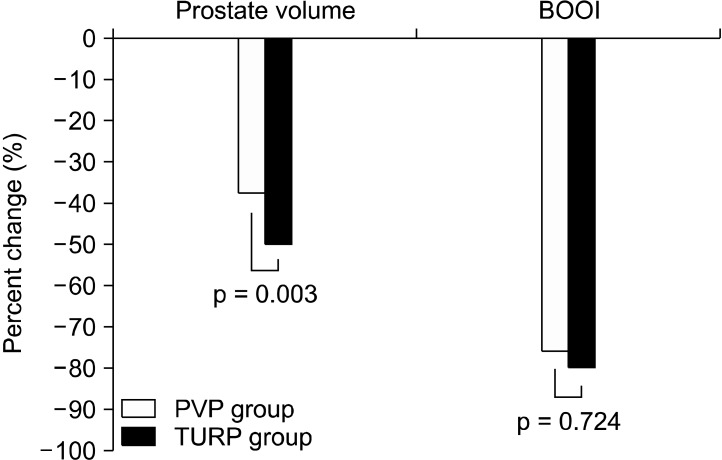
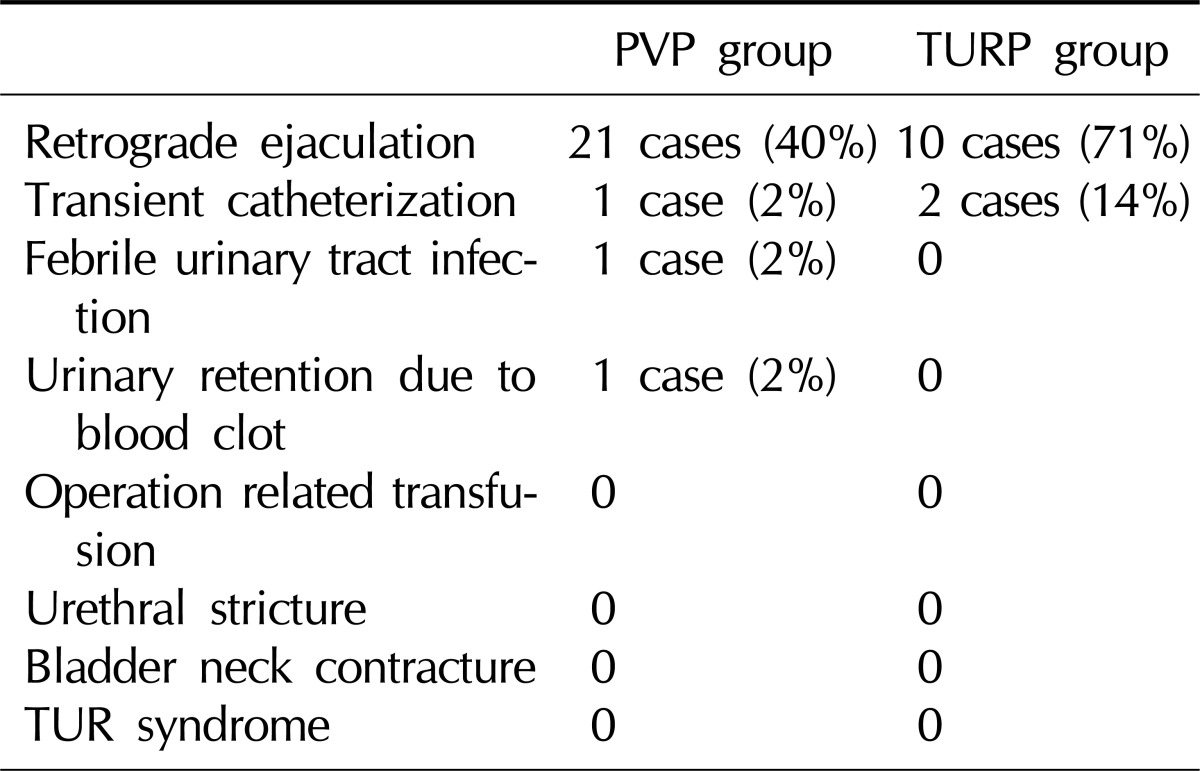
Fig. 2 shows the percent changes of prostate volume and BOOI. Although the percent change of the prostate volume was higher in the TURP group than the PVP group, the percent change of BOOI did not differ between the groups. Table 3 demonstrates surgical complications. Retrograde ejaculation and transient catheterization was much less common in the PVP group. There was no operation-related transfusion, urethral stricture, bladder neck contracture, or TUR syndrome in either group.
The present study shows that PVP using a high power KTP laser can effectively reduce the prostate volume and relieve obstruction, and it has beneficial effects on the IPSS, bother score, Qmax, and PVR. It is important to remove the prostate tissue effectively to relieve the obstruction and improve the LUTS in the surgical treatment of BPH. TURP has been accepted as the gold standard treatment for BPH. TURP can effectively remove prostate tissue immediately and lead to the improvement of voiding after surgery.7 The direct and anatomic resection of prostate tissue during TURP can result in not only the immediate improvement of voiding parameters but also good long-term outcomes.
A KTP laser of 532 nm wavelength provides an optical penetration depth of less than 0.8 mm in prostate tissue and leads to confinement of high density energy to a superficial layer of prostatic tissue, resulting in effective and precise ablation.8 Kuntzman et al9 showed that PVP could create a TUR-like defect in an animal model. In their study, large channels were produced with unscarred prostate tissue 8 weeks after PVP in canine prostates. Several clinical studies have suggested that PVP could reduce prostate volume effectively. Kumar10 investigated the reduction of prostate volume after PVP in BPH and prostate cancer patients (8 patients in BPH, 10 in prostate cancer). They showed that the mean prostate volume was decreased from 53.2 ml to 26.2 ml and suggested that PVP can effectively vaporize obstructive prostatic tissue, leading to a significant decrease in total prostate volume (51% decrease). Sandhu et al11 reported that even in patients with a large prostate (prostate volume ≥60 ml, mean 101 ml), PVP can effectively improve LUTS and voiding parameters. Surgical duration was 123±70 minutes and no transfusion was required. They showed that the IPSS decreased from 18.4 to 6.7 at 12 months, and the Qmax increased from 7.9 ml/s to 18.9 ml/s. They concluded that high-power KTP PVP was safe and efficacious even for large-volume prostates, with low morbidity, acceptable surgical duration, and good postoperative results.
In order to confirm the reduction of the obstruction after prostate surgery, PFS is essential. However, there are only a few non-comparative studies that evaluated the change of obstruction after PVP by using PFS. Recently, Hamann et al12 investigated the impact of PVP on urodynamic results in a prospective study. Video-urodynamics were carried out after 3 and 12 months to determine the changes in bladder function. Despite a lack of postoperative data on the prostate volume, they showed that the mean PdetQmax was decreased from 75.0 to 33.7 and 36.6 cmH2O at 3 and 12 months of follow up. The Schafer obstruction grade was also reduced from 3.6 to 0.9 and 1.1 at 3 and 12 months postoperatively. Pedersen et al13 also recently reported the 2-year follow-up results of PFS. In 77 patients who underwent PVP, the median BOOI was decreased from 53 to 9 at 24 months. These data suggest that KTP laser PVP effectively reduced the obstruction. Our current study shows similar results and strengthens the evidence that PVP can relieve bladder outlet obstruction effectively. In our study, the mean PdetQmax was decreased from 68.7±23.3 to 40.6±11.2 cmH2O, the BOOI was reduced from 49.8±25.6 to 9.8±20.7, and the Schafer grade from 2.9±1.4 to 1.2±0.8. The percentage of patients with BOOI ≥40 was markedly decreased from 64% to 4% after PVP. In the current study, we also compared the prostate volume and urodynamic results with the TURP. The effectiveness of PVP for removing the prostate tissue and reducing the obstruction were comparable with TURP.
This study has several limitations because it was performed under a nonrandomized design. First, the preoperative prostate volume and obstruction severity was higher in the TURP group than the PVP group. In addition, it was difficult to compare the numeric changes directly between the two groups. However, we were able to show that the postoperative prostate volume was similar in both groups. We conclude that these data are still valuable because the endpoint, that is, to improve the urine flow, is more important than the numeric change in prostate volume. In this study, the postoperative PdetQmax, BOOI, and Schafer grade were also similar in the two groups. The percent change of BOOI did not differ significantly between the two groups in spite of the difference in the prostate volume. Therefore, the effect appeared to be similar between PVP and TURP. Second, the number of patients in the TURP group was much smaller than that in the PVP group. In this study, the patients who agreed with the protocol were enrolled after given full information about the surgery. The most common reason thatpatients underwent PVP instead of TURP was that more patients wanted PVP because of its greater safety and earlier recovery. Although the number of patients in the TURP group was small, the data about TURP was valuable as a reference for evaluating the outcomes of PVP in this study.
This trial demonstrated that PVP is as effective as TURP, producing similar improvements in subjective (symptom & bother) and objective (Qmax & PVR) voiding parameters in men with BPH. This study also shows that PVP using a high power KTP laser could reduce the size of the prostate effectively and relieve bladder outlet obstruction similarly to TURP at 6-month follow up.
ACKNOWLEDGEMENTS
This study was supported by the Samsung Medical Center Clinical Research Development Program grant #CRS-104-02-4.
References
1. Bachmann A, Schürch L, Ruszat R, Wyler SF, Seifert HH, Müller A, et al. Photoselective vaporization (PVP) versus transurethral resection of the prostate (TURP): a prospective bi-centre study of perioperative morbidity and early functional outcome. Eur Urol. 2005; 48:965–971. PMID: 16126327.

2. Malek RS, Kuntzman RS, Barrett DM. Photoselective potassium-titanyl-phosphate laser vaporization of the benign obstructive prostate: observations on long-term outcomes. J Urol. 2005; 174:1344–1348. PMID: 16145416.

3. Sarica K, Alkan E, Lüleci H, Taşci AI. Photoselective vaporization of the enlarged prostate with KTP laser: long-term results in 240 patients. J Endourol. 2005; 19:1199–1202. PMID: 16359215.

4. Tan AH, Gilling PJ. Lasers in the treatment of benign prostatic hyperplasia: an update. Curr Opin Urol. 2005; 15:55–58. PMID: 15586032.

5. Schäfer W, Abrams P, Liao L, Mattiasson A, Pesce F, Spangberg A, et al. International Continence Society. Good urodynamic practices: uroflowmetry, filling cystometry, and pressure-flow studies. Neurourol Urodyn. 2002; 21:261–274. PMID: 11948720.

6. Abrams P. Bladder outlet obstruction index, bladder contractility index and bladder voiding efficiency: three simple indices to define bladder voiding function. BJU Int. 1999; 84:14–15. PMID: 10444116.

7. Hakenberg OW, Helke C, Manseck A, Wirth MP. Is there a relationship between the amount of tissue removed at transurethral resection of the prostate and clinical improvement in benign prostatic hyperplasia. Eur Urol. 2001; 39:412–417. PMID: 11306879.

8. Te AE, Malloy TR, Stein BS, Ulchaker JC, Nseyo UO, Hai MA, et al. Photoselective vaporization of the prostate for the treatment of benign prostatic hyperplasia: 12-month results from the first United States multicenter prospective trial. J Urol. 2004; 172:1404–1408. PMID: 15371855.

9. Kuntzman RS, Malek RS, Barrett DM, Bostwick DG. Potassium-titanyl-phosphate laser vaporization of the prostate: a comparative functional and pathologic study in canines. Urology. 1996; 48:575–583. PMID: 8886063.

10. Kumar SM. Photoselective vaporization of the prostate: a volume reduction analysis in patients with lower urinary tract symptoms secondary to benign prostatic hyperplasia and carcinoma of the prostate. J Urol. 2005; 173:511–513. PMID: 15643231.

11. Sandhu JS, Ng C, Vanderbrink BA, Egan C, Kaplan SA, Te AE. High-power potassium-titanyl-phosphate photoselective laser vaporization of prostate for treatment of benign prostatic hyperplasia in men with large prostates. Urology. 2004; 64:1155–1159. PMID: 15596189.

12. Hamann MF, Naumann CM, Seif C, van der Horst C, Jünemann KP, Braun PM. Functional outcome following photoselective vaporisation of the prostate (PVP): urodynamic findings within 12 months follow-up. Eur Urol. 2008; 54:902–907. PMID: 18502565.

13. Pedersen JM, Romundstad PR, Mjønes JG, Arum CJ. 2-year followup pressure flow studies of prostate photoselective vaporization using local anesthesia with sedation. J Urol. 2009; 181:1794–1799. PMID: 19233401.

Fig. 1
Changes in prostate volume, PdetQmax, and BOOI in PVP and TURP group from baseline to 6 months follow up. White bars represent baseline and black bars 6 months follow up. PVP: photoselective laser vaporization prostatectomy, TURP: transurethral resection of the prostate, PdetQmax: detrusor pressure at maximum flow rate, BOOI: bladder outlet obstruction Index. *p<0.05.
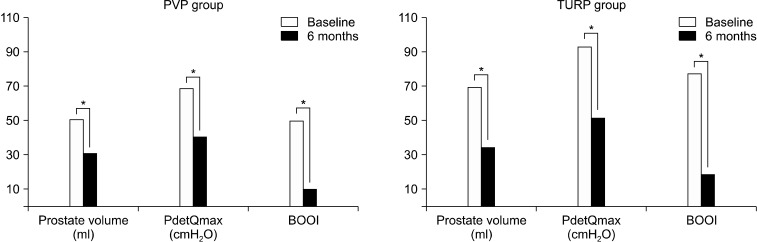
Fig. 2
Change in obstructive parameters - PdetQmax, BOOI prevs. post-treatment. The values were adjusted using baseline values as covariates. The white bars represent the PVP group and black bars, the TURP group. PVP: photoselective laser vaporization prostatectomy, TURP: transurethral resection of the prostate, BOOI: bladder outlet obstruction index, PdetQmax: detrusor pressure at maximum flow rate, p: group comparisons of improvement rates after treatment.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download