Abstract
Sexual dysfunction is a common condition in patients taking antipsychotics, and is the most bothersome symptom and adverse drug effect, resulting in a negative effect on treatment compliance. It is known that hyperprolactinemia is a major cause of sexual dysfunction. Based on the blockade of dopamine D2 receptors, haloperidol, risperidone, and amisulpride are classed as prolactin-elevating antipsychotics, while olanzapine, clozapine, quetiapine, ziprasidone, and aripiprazole are classed as prolactin-sparing drugs. Risperidone and the other typical antipsychotics are associated with a high rate of sexual dysfunction as compared to olanzapine, clozapine, quetiapine, and aripiprazole. With regard to treatment in patients suffering from sexual dysfunction, sildenafil was associated with significantly more erections sufficient for penetration as compared to a placebo. Subsequent studies are needed in order to provide physicians with a better understanding of this problem, thereby leading toward efficacious and safe solutions.
Sexual dysfunction is a common condition in patients taking antipsychotic medication, with a reported prevalence of 45~80% in males and 30~80% in females. It is the most bothersome symptom and adverse drug effect in men and women with schizophrenia, resulting in a negative effect on treatment compliance.1-3
This report will review the current understanding of antipsychotic-induced sexual dysfunction and its management.
The mechanisms by which antipsychotic drugs may cause sexual dysfunction are as follows: histamine receptor antagonism, dopamine receptor antagonism, dopamine D2 receptor antagonism, cholinergic receptor antagonism, and alpha-adrenergic alpha receptor antagonism.4,5
Concretely, being bound to histaminergic receptors may impair arousal by directly increasing sedation. Dopaminergic receptor antagonism may decrease the libido by inhibiting motivation and reward. Blockade of dopamine D2 receptors in the tuberoinfundibular pathway by antipsychotics may decrease the libido, impair arousal, and impair orgasm indirectly, by leading to elevated prolactin levels. Cholinergic receptor antagonism may induce erectile dysfunction by reducing peripheral vasodilation. Alpha-adrenergic alpha receptor antagonism can reduce peripheral vasodilation, resulting in erectile dysfunction in men and decreased lubrication in women. Additionally, abnormal ejaculation is correlated with the anti-adrenergic effects of treatment.
It is well known that hyperprolactinemia is a major cause of sexual dysfunction in men and women taking antipsychotics by the aforementioned mechanisms.6,7 Depending on the blockade of dopamine D2 receptors, haloperidol, risperidone, and amisulpride are classed as prolactin-elevating antipsychotics, while olanzapine, clozapine, quetiapine, ziprasidone, and aripiprazole are classed as prolactin-sparing drugs.4
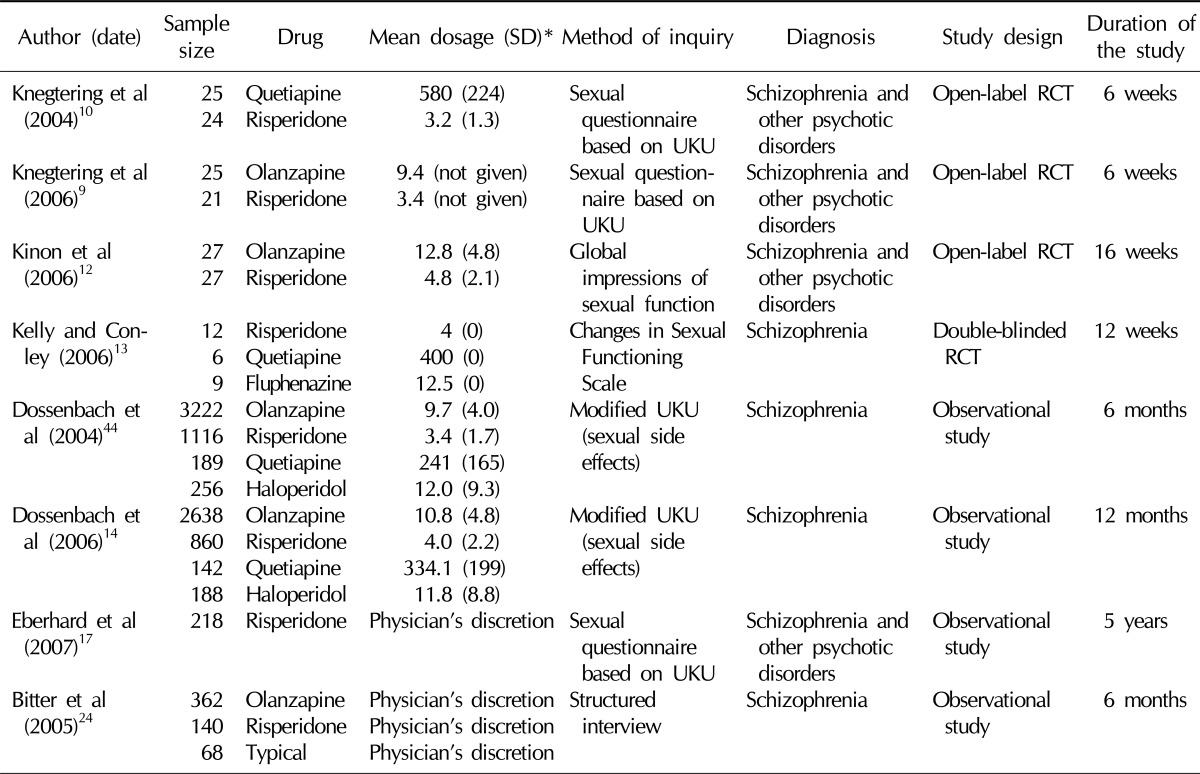
The large majority of studies concerning antipsychotic-induced sexual dysfunction are small cross sectional studies or small scale observational studies.8 According to a recent review article, four randomized clinical trials and four large-scale long-term observational studies from three cohorts have reported primary outcomes concerning antipsychotic-induced sexual dysfunction.9-13 Foremost, we will review these reports as well as other related cross-sectional case control studies and small-scale short-term observational studies (Table 1).
It is known that haloperidol, which is a typical antipsychotic, raises serum prolactin levels to 20~40 ng/ml in therapeutic doses.5
From evidence of a large prospective cohort study, 71.1% of men and women taking haloperidol over 12 months complained of sexual dysfunction depending on the modified version of the Udvalg for Kliniske Undersøgelser (Danish for rysfunction Clinical Examinations'; UKU Side Effect Rating Scale) which is composed of 5 items: libido, amenorrhea, gynecomastia, erectile dysfunction/sexual dysfunction, and galactorrhea (Table 1).14 The prevalence rate of decreased libido is 60.0%, erectile dysfunction/sexual dysfunction is 52.3%, and amenorrhea is 53.8%. The odds ratio, compared to patients treated with olanzapine, for decreased libido, erectile dysfunction/sexual dysfunction, and amenorrhea are 3.25 (2.14~4.92), 3.04 (1.94~4.74), and 4.06 (2.20~7.51), respectively.
In a cross sectional study (n=131), 30.8% of male patients complained of decreased libido, 30.8% complained of erectile dysfunction, and 27.7% complained of ejaculatory disorder. In female patients, 23.8% complained of decreased libido, 9.4% complained of arousal disorder, and 8.1% complained of vaginal dryness.15
Risperidone is a representative atypical antipsychotic drug with a high probability of prolactin elevation. According to clinical trials and cross sectional studies, risperidone elevates the serum prolactin in a dose dependent manner and up to a level of 30~60 ng/ml when used at therapeutic doses.9,16 A prospective 5 year observational study evaluating 128 men and 90 women reported that risperidone induces a higher prolactin elevation than other atypical antipsychotics (Table 1).17
Evidence from a large prospective observational study showed that 67.8% of men and women receiving risperidone for over 1 year experienced sexual dysfunction.14 Reduced libido is the most commonly reported disturbance (described by 60.0% of patients), while 46.0% of patients report erectile dysfunction/sexual dysfunction and 42.1% of patients report amenorrhea. The rate of sexual dysfunction is significantly high as compared with patients receiving olanzapine (odds ratio: 2.02; 95% confidence interval: 1.63~2.49).
According to a cross-sectional study studying males and females separately (n=131), 37.8% of males reported decreased libido, 32.1% reported erectile dysfunction, and 32.6% reported ejaculatory disorder. In female patients, 40.5% reported decreased libido, 19.0% reported arousal disorder, and 15% reported vaginal dryness.15
A small scale study reported gynecomastia, galactorrhea, and priapism in male patients. Further, female patients were reported to experience amenorrhea and galactorrhea.6
A cross-sectional study including 60 schizophrenic male patients who showed atypical neuroleptic clozapine was associated with low prolactin serum level as compared to classical antipsychotics (mean=12.6 ng/ml, standard deviation [SD]=11.2 vs. mean 18.2 ng/ml, SD=16.2).18 Also, another cross sectional study (n=18 schizophrenic male patients) showed clozapine was associated with a low prolactin serum level as compared to risperidone (mean=27 ng/ml, SD=14 vs. mean=27 ng/ml, SD=14).19 It is generally believed that clozapine produces a low incidence of hyperprolactinemia-related adverse sexual events including decreased libido and impaired arousal relative to classical antipsychotics.18
A retrospective study investigated by review of medical records reported a significantly lower proportion of patients with sexual dysfunctions in the clozapine group as compared to the haloperidol and risperidone groups.20 However, sexual dysfunction related to anti-adrenergic and anticholinergic effects (erectile and ejaculatory problems as well as priapism) does occur with clozapine.6,21
Olanzapine temporarily increases the prolactin level. Moreover, in most cases, the elevated prolactin level returns to a normal level. In a double blind clinical trial, prolactin elevation caused by olanzapine normalized after six weeks as compared to the control group in both male and female patients.22
According to a 28-week double-blind clinical trial conducted with 339 patients and aimed at the efficacy of olanzapine, olanzapine produces a low incidence of adverse sexual events in men as compared to risperidone-treated men. Further, delayed ejaculation was significantly lower (2.8% vs. 11.5% of male patients, respectively; p<0.05).23
An open-label, prospective 4-month study in hyperprolactinemic patients with schizophrenia explored whether prolactin levels decrease after switching from antipsychotic therapy to olanzapine therapy. This study reported that patients who switched to olanzapine experienced significant reductions in mean serum prolactin levels in both males and females; furthermore, galactorrhea, gynecomastia, and sexual functioning were significantly improved in both genders (Table 1).12
A 6-month observational study examining sexual functioning among first-time treated schizophrenia patients showed that the loss of libido was significantly less common in the olanzapine group (17.8% at 6 months) as compared to the risperidone (35.5% at 6 months) and haloperidole groups (38.7% at 6 months).24
In a randomized open-label comparison of the impact of olanzapine versus risperidone on sexual functioning, less sexual dysfunction occurred in the group treated with olanzapine (n=20) than the risperidone group (n=19), with a major significant difference in erectile dysfunction (erectile dysfunction: 0% in the olanzapine group vs. 31.6% in the risperidone group).9
In a large population study, quetiapine was not associated with the increase in prolactin levels when a therapeutic dose was used.6,25-28
In an open-label study, including patients with schizophrenia or a related psychotic illness who were randomized to quetiapine (200~1200 mg/day) or risperidone (1~6 mg/day) for 6 weeks, sexual dysfunction was lower in patients treated with quetiapine (n=25) compared to those treated with risperidone (n=26). Specifically, there was a significant difference in decreased libido and impaired arousal.10
There has been just one double-blind clinical trial to evaluate sexual dysfunction as a primary outcome measure.27 People with treatment-resistant schizophrenia participated in a randomized double-blind 12-week trial of risperidone (4 mg/day), quetiapine (400 mg/day), or fluphenazine (12.5 mg/day). Overall, only quetiapine was associated with the normalization of prolactin levels and had the greatest benefits among these drugs regarding sexual functioning; in particular, there was a significant difference in orgasmic function.13 Thus, it appears that quetiapine is associated with a lower sexual dysfunction rate than risperidone and haloperidol.
According to double-blind clinical trial studies, aripiprazole did not increase the prolactin level or normalize prolactin levels in patients with elevated baseline levels caused by typical antipsychotics.29-37
In an open-label randomized clinical trial, patients for whom a change of antipsychotic medication was indicated due to a lack of tolerability and/or symptom control, switched to aripiprazole and were treated for 26 weeks, showing a significant reduction in overall sexual dysfunction as measured on the total score of the Arizona Sexual Experience Scale (composed of following five domains: sex drive, arousal, vaginal lubrication or penile erection, and ability to reach orgasm).38 Also, in another open label study, switching to aripiprazole was associated with a significant improvement in sexual desire, erectile dysfunction, and ejaculatory disorder.39
Dopamine agonist (bromocriptine, cabergoline) and dopamine releasing agent (amantadine) were tried in a patient suffering from sexual dysfunction secondary to antipsychotics, however most of the studies are open label, uncontrolled studies, or case reports.
According to a Cochrane Database Systematic Review, only two well-designed randomized controlled trials can be relied on for determining the effects for treatment of sexual dysfunction due to antipsychotic therapy.40
In the first of these two studies, a randomized, double-blind, placebo controlled, flexible-dose, two-way crossover trial was carried out. Thirty-two married male outpatients with schizophrenia or delusional disorder and antipsychotic-induced erectile dysfunction were recruited for the trial. The patients reported significant improvement while taking sildenafil in the number of adequate erections (number of erections hard enough for penetration: 6.52 vs. 3.32; p<0.001), satisfaction with sexual intercourse, and ability to undergo erections for over 2 weeks. The odds ratios for adequate erections and for satisfactory sexual intercourse with sildenafil were 4.07 and 3.77, respectively. There were no major side effects or adverse drug interactions, specifically nasal congestion (12.5% vs. 0%) or headaches (9.4% vs. 3.1%).41
Another double-blind, placebo-controlled crossover study was undertaken in 10 neuroleptic-treated male schizophrenic outpatients in order to assess the effect of co-administration of 15 mg/day of selegiline (selective monoamine oxidase inhibitor, inducing dopamine secretion) for 3 weeks on their sexual dysfunction. Selegiline was not found to be effective in improving any domain of sexual functioning despite a significant decrease in prolactin levels.42
On the basis of the scarce data available, Costa et al43 attempted to design a preliminary stepwise algorithm for the clinical management of antipsychotic-induced sexual dysfunction, as follows: 1. Gradually reduce dosage of the antipsychotic 2. If there is no symptoms improvement, switch to other antipsycotics with better sexual profile; 3. If the symptoms still persist, prescribe drug association already mentioned in the article.
While the literature clarifying the influence of antipsychotic on sexual funtion is limited, these studies suggest that the relative impact of antipsychotics on sexual dysfunction can be summarized as risperidone, and typical antipsychotics are associated with a high rate of sexual dysfunction as compared to olanzapine, clozapine, quetiapine, and aripiprazole. Thus, it is possible for psychiatrists to minimize the risk of sexual dysfunction through the appropriate choice of antipsychotics.
With regard to treatment in patients suffering from sexual dysfunction, sildenafil was associated with significantly more erections sufficient for penetration as compared to a placebo. Subsequent studies are needed in order to provide physicians with a better understanding of this problem, thereby leading toward efficacious and safe solutions.
References
1. Finn SE, Bailey JM, Schultz RT, Faber R. Subjective utility ratings of neuroleptics in treating schizophrenia. Psychol Med. 1990; 20:843–848. PMID: 1980954.

2. Lambert M, Conus P, Eide P, Mass R, Karow A, Moritz S, et al. Impact of present and past antipsychotic side effects on attitude toward typical antipsychotic treatment and adherence. Eur Psychiatry. 2004; 19:415–422. PMID: 15504648.

3. Olfson M, Uttaro T, Carson WH, Tafesse E. Male sexual dysfunction and quality of life in schizophrenia. J Clin Psychiatry. 2005; 66:331–338. PMID: 15766299.

4. Haddad PM, Wieck A. Antipsychotic-induced hyperprolactinaemia: mechanisms, clinical features and management. Drugs. 2004; 64:2291–2314. PMID: 15456328.
5. Knegtering H, van der Moolen AE, Castelein S, Kluiter H, van den Bosch RJ. What are the effects of antipsychotics on sexual dysfunctions and endocrine functioning? Psychoneuroendocrinology. 2003; 28(Suppl 2):109–123. PMID: 12650685.

6. Kelly DL, Conley RR. Sexuality and schizophrenia: a review. Schizophr Bull. 2004; 30:767–779. PMID: 15954189.

7. Smith SM, O'Keane V, Murray R. Sexual dysfunction in patients taking conventional antipsychotic medication. Br J Psychiatry. 2002; 181:49–55. PMID: 12091263.

8. Serretti A, Chiesa A. A meta-analysis of sexual dysfunction in psychiatric patients taking antipsychotics. Int Clin Psychopharmacol. 2011; 26:130–140. PMID: 21191308.

9. Knegtering H, Boks M, Blijd C, Castelein S, van den Bosch RJ, Wiersma D. A randomized open-label comparison of the impact of olanzapine versus risperidone on sexual functioning. J Sex Marital Ther. 2006; 32:315–326. PMID: 16709552.

10. Knegtering R, Castelein S, Bous H, Van Der Linde J, Bruggeman R, Kluiter H, et al. A randomized open-label study of the impact of quetiapine versus risperidone on sexual functioning. J Clin Psychopharmacol. 2004; 24:56–61. PMID: 14709948.

11. Knegtering H, van den Bosch R, Castelein S, Bruggeman R, Sytema S, van Os J. Are sexual side effects of prolactin-raising antipsychotics reducible to serum prolactin? Psychoneuroendocrinology. 2008; 33:711–717. PMID: 18395353.

12. Kinon BJ, Ahl J, Liu-Seifert H, Maguire GA. Improvement in hyperprolactinemia and reproductive comorbidities in patients with schizophrenia switched from conventional antipsychotics or risperidone to olanzapine. Psychoneuroendocrinology. 2006; 31:577–588. PMID: 16488084.

13. Kelly DL, Conley RR. A randomized double-blind 12-week study of quetiapine, risperidone or fluphenazine on sexual functioning in people with schizophrenia. Psychoneuroendocrinology. 2006; 31:340–346. PMID: 16198059.

14. Dossenbach M, Dyachkova Y, Pirildar S, Anders M, Khalil A, Araszkiewicz A, et al. Effects of atypical and typical antipsychotic treatments on sexual function in patients with schizophrenia: 12-month results from the Intercontinental Schizophrenia Outpatient Health Outcomes (IC-SOHO) study. Eur Psychiatry. 2006; 21:251–258. PMID: 16530390.

15. Bobes J, Garc A-Portilla MP, Rejas J, Hern Ndez G, Garcia-Garcia M, Rico-Villademoros F, et al. Frequency of sexual dysfunction and other reproductive side-effects in patients with schizophrenia treated with risperidone, olanzapine, quetiapine, or haloperidol: the results of the EIRE study. J Sex Marital Ther. 2003; 29:125–147. PMID: 12623765.

16. Spollen JJ 3rd, Wooten RG, Cargile C, Bartztokis G. Prolactin levels and erectile function in patients treated with risperidone. J Clin Psychopharmacol. 2004; 24:161–166. PMID: 15206663.

17. Eberhard J, Lindström E, Holstad M, Levander S. Prolactin level during 5 years of risperidone treatment in patients with psychotic disorders. Acta Psychiatr Scand. 2007; 115:268–276. PMID: 17355517.
18. Aizenberg D, Modai I, Landa A, Gil-Ad I, Weizman A. Comparison of sexual dysfunction in male schizophrenic patients maintained on treatment with classical antipsychotics versus clozapine. J Clin Psychiatry. 2001; 62:541–544. PMID: 11488365.

19. Turrone P, Kapur S, Seeman MV, Flint AJ. Elevation of prolactin levels by atypical antipsychotics. Am J Psychiatry. 2002; 159:133–135. PMID: 11772702.

20. Mullen B, Brar JS, Vagnucci AH, Ganguli R. Frequency of sexual dysfunctions in patients with schizophrenia on haloperidol, clozapine or risperidone. Schizophr Res. 2001; 48:155–158. PMID: 11345946.

21. Cutler AJ. Sexual dysfunction and antipsychotic treatment. Psychoneuroendocrinology. 2003; 28(Suppl 1):69–82. PMID: 12504073.

22. Crawford AM, Beasley CM Jr, Tollefson GD. The acute and long-term effect of olanzapine compared with placebo and haloperidol on serum prolactin concentrations. Schizophr Res. 1997; 26:41–54. PMID: 9376336.

23. Tran PV, Hamilton SH, Kuntz AJ, Potvin JH, Andersen SW, Beasley C Jr, et al. Double-blind comparison of olanzapine versus risperidone in the treatment of schizophrenia and other psychotic disorders. J Clin Psychopharmacol. 1997; 17:407–418. PMID: 9315992.

24. Bitter I, Basson BR, Dossenbach MR. Antipsychotic treatment and sexual functioning in first-time neuroleptic-treated schizophrenic patients. Int Clin Psychopharmacol. 2005; 20:19–21. PMID: 15602111.

25. Borison RL, Arvanitis LA, Miller BG. U.S. Seroquel Study Group. ICI 204,636, an atypical antipsychotic: efficacy and safety in a multicenter, placebo-controlled trial in patients with schizophrenia. J Clin Psychopharmacol. 1996; 16:158–169. PMID: 8690831.
26. Arvanitis LA, Miller BG. The Seroquel Trial 13 Study Group. Multiple fixed doses of "Seroquel" (quetiapine) in patients with acute exacerbation of schizophrenia: a comparison with haloperidol and placebo. Biol Psychiatry. 1997; 42:233–246. PMID: 9270900.

27. Small JG, Hirsch SR, Arvanitis LA, Miller BG, Link CG. Seroquel Study Group. Quetiapine in patients with schizophrenia. A high- and low-dose double-blind comparison with placebo. Arch Gen Psychiatry. 1997; 54:549–557. PMID: 9193196.
28. King DJ, Link CG, Kowalcyk B. A comparison of bd and tid dose regimens of quetiapine (Seroquel) in the treatment of schizophrenia. Psychopharmacology (Berl). 1998; 137:139–146. PMID: 9630000.

29. Dossenbach M, Hodge A, Anders M, Molnár B, Peciukaitiene D, Krupka-Matuszczyk I, et al. Prevalence of sexual dysfunction in patients with schizophrenia: international variation and underestimation. Int J Neuropsychopharmacol. 2005; 8:195–201. PMID: 15631645.

30. Casey DE, Carson WH, Saha AR, Liebeskind A, Ali MW, Jody D, et al. Aripiprazole Study Group. Switching patients to aripiprazole from other antipsychotic agents: a multicenter randomized study. Psychopharmacology (Berl). 2003; 166:391–399. PMID: 12610718.

31. Kasper S, Lerman MN, McQuade RD, Saha A, Carson WH, Ali M, et al. Efficacy and safety of aripiprazole vs. haloperidol for long-term maintenance treatment following acute relapse of schizophrenia. Int J Neuropsychopharmacol. 2003; 6:325–337. PMID: 14609439.

32. Lee BH, Kim YK, Park SH. Using aripiprazole to resolve antipsychotic-induced symptomatic hyperprolactinemia: a pilot study. Prog Neuropsychopharmacol Biol Psychiatry. 2006; 30:714–717. PMID: 16571367.

33. Marder SR, McQuade RD, Stock E, Kaplita S, Marcus R, Safferman AZ, et al. Aripiprazole in the treatment of schizophrenia: safety and tolerability in short-term, placebo-controlled trials. Schizophr Res. 2003; 61:123–136. PMID: 12729864.

34. McQuade RD, Stock E, Marcus R, Jody D, Gharbia NA, Vanveggel S, et al. A comparison of weight change during treatment with olanzapine or aripiprazole: results from a randomized, double-blind study. J Clin Psychiatry. 2004; 65(Suppl 18):47–56. PMID: 15600384.
35. Pigott TA, Carson WH, Saha AR, Torbeyns AF, Stock EG, Ingenito GG. Aripiprazole Study Group. Aripiprazole for the prevention of relapse in stabilized patients with chronic schizophrenia: a placebo-controlled 26-week study. J Clin Psychiatry. 2003; 64:1048–1056. PMID: 14628980.
36. Potkin SG, Saha AR, Kujawa MJ, Carson WH, Ali M, Stock E, et al. Aripiprazole, an antipsychotic with a novel mechanism of action, and risperidone vs placebo in patients with schizophrenia and schizoaffective disorder. Arch Gen Psychiatry. 2003; 60:681–690. PMID: 12860772.

37. Baggaley M. Sexual dysfunction in schizophrenia: focus on recent evidence. Hum Psychopharmacol. 2008; 23:201–209. PMID: 18338766.

38. Hanssens L, L'Italien G, Loze JY, Marcus RN, Pans M, Kerselaers W. The effect of antipsychotic medication on sexual function and serum prolactin levels in community-treated schizophrenic patients: results from the Schizophrenia Trial of Aripiprazole (STAR) study (NCT00237913). BMC Psychiatry. 2008; 8:95. PMID: 19102734.

39. Mir A, Shivakumar K, Williamson RJ, McAllister V, O'Keane V, Aitchison KJ. Change in sexual dysfunction with aripiprazole: a switching or add-on study. J Psychopharmacol. 2008; 22:244–253. PMID: 18308789.

40. Berner MM, Hagen M, Kriston L. Management of sexual dysfunction due to antipsychotic drug therapy. Cochrane Database Syst Rev. 2007; (1):CD003546. PMID: 17253492.

41. Gopalakrishnan R, Jacob KS, Kuruvilla A, Vasantharaj B, John JK. Sildenafil in the treatment of antipsychotic-induced erectile dysfunction: a randomized, double-blind, placebo-controlled, flexible-dose, two-way crossover trial. Am J Psychiatry. 2006; 163:494–499. PMID: 16513872.

42. Kodesh A, Weizman A, Aizenberg D, Hermesh H, Gelkopf M, Zemishlany Z. Selegiline in the treatment of sexual dysfunction in schizophrenic patients maintained on neuroleptics: a pilot study. Clin Neuropharmacol. 2003; 26:193–195. PMID: 12897639.

43. Costa AM, Lima MS, Mari Jde J. A systematic review on clinical management of antipsychotic-induced sexual dysfunction in schizophrenia. Sao Paulo Med J. 2006; 124:291–297. PMID: 17262163.

44. Dossenbach M, Erol A, el Mahfoud Kessaci M, Shaheen MO, Sunbol MM, Boland J, et al. IC-SOHO Study Group. Effectiveness of antipsychotic treatments for schizophrenia: interim 6-month analysis from a prospective observational study (IC-SOHO) comparing olanzapine, quetiapine, risperidone, and haloperidol. J Clin Psychiatry. 2004; 65:312–321. PMID: 15096069.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download