Abstract
Purpose
To understand the potential contribution of systemic endothelial dysfunction to diabetic erectile dysfunction, and the time course of erectile dysfunction in a streptozotocin (STZ)-induced diabetic rat model.
Materials and Methods
Among 84, 12-week-old Sprague-Dawley rats, 48 rats received intraperitoneal STZ and were classified into six groups of diabetes by the period of observation (n=8). The remaining 36 rats were also grouped, similar to the diabetic groups, and served as normal controls. After 4, 6, 8, 10, 12, and 14 weeks of diabetes (serum glucose >250 mg%), all rats underwent cavernous nerve electrostimulation (3 V, 0.2 ms, 30 sec) with varying frequency (2.5~20 Hz). At the end of the study, 8 ml of blood was taken to measure the plasma markers of endothelial function and glycosylated hemoglobin.
Results
Compared to the control, significant reduction of erectile response was not observed until eight weeks after diabetes induction. The diabetic rats had elevation of all plasma markers except for l-selectin. However, the correlation analysis revealed that no systemic marker of endothelial dysfunction was associated with change in erectile function. Only the level of hemoglobin A1c (HbA1c) showed a modest but significant correlation with the peak intracavernosal pressure, corrected by mean arterial pressure (ρ=-0.183), and the area under the curve of the cavernosometry (ρ=-0.207).
Erectile dysfunction (ED) often affects diabetic patients. According to a recent study, the crude prevalence of ED was over 50% among men with diabetes.1 The etiology of ED in diabetic patients is presumed to be multifactorial, but appears predominantly to be caused by a failure of nitric oxide (NO)-mediated cavernosal smooth muscle relaxation due to an autonomic neuropathy and endothelial dysfunction.2
There is growing evidence to support the relationship between systemic endothelial dysfunction and ED in diabetic patients.3,4 Compared to diabetic patients with normal potency, diabetic patients with ED have different results on tests of systemic endothelial function, such as response to L-arginine stimulation, circulating concentration of plasma thrombomodulin and cell adhesion molecules.3 A significant reduction in endothelium-mediated vascular responses was associated with impaired erectile function in the diabetic group, when compared with matched non-diabetic controls from human and animal studies.4,5 By contrast, Browne et al6 reported no difference in the forearm blood flow response to acetylcholine, a surrogate marker of endothelial function, between impotent and potent diabetic men. While the explanation for these discrepant results is not clear, the differing sensitivity of the various tests of endothelial dysfunction and diabetes' variation in severity, which is dependent on diabetes' duration and glycemic control, might contribute to the inconsistent results. Serial evaluation of erectile function and evaluation of its association with endothelial function during the course of diabetes in rats might provide insight into this unresolved issue.
Streptozotocin (STZ)-induced diabetic rats have been widely used to elucidate the mechanisms involved in the pathophysiology of diabetic ED. Most studies using diabetic rats have measured erectile responses to cavernous nerve stimulation 6~12 weeks after induction of diabetes with various doses of intraperitoneal STZ.7-10 However, the absence of a standardized protocol for induction of diabetes and the wide range of time points used for the evaluation of erectile responses might provide inconsistent data leading to an incomplete understanding of the natural course of ED in STZ-induced diabetic rats, and making it difficult to interpret and compare experimental results. Only a few studies have addressed this concern.11,12
Therefore, in this study, we investigated changes in erectile function and endothelial function during the course of STZ-induced diabetes in rats to improve our understanding of the association of systemic endothelial dysfunction with diabetic ED.
Eighty-four 8-week-old male Sprague-Dawley rats were classified randomly into a diabetic (n=48) or control (n=36) group. The rats were kept under a 12 hours light/dark cycle and fed rat pellets ad libitum. The rats received either STZ (50 mg/kg, intraperitoneal injection) or the same volume of vehicle (0.1 M citrate buffer, pH 4.5). At the time of injection, the animals weighed 180~220 g. Blood glucose levels were checked in all animals 48 hours after the injection using an Accu-Chek Compact Meter (Roche Diagnostics, Indianapolis, IN, USA) and diabetes was confirmed when the rats had significant hyperglycemia (>250 mg/dl). By that time, approximately 60% of rats developed diabetes. The remaining non-hyperglycemic rats received a second injection (30 mg/kg) and they became diabetic within three days. Body weight and blood glucose levels were monitored every other week. All procedures were approved by the Institutional Animal Care and Use Committee of Seoul National University Hospital (IACuc No 10-0236).
Erectile function was evaluated in anesthetized diabetic rats and age-matched control rats at 4, 6, 8, 10, 12, and 14 weeks after induction of diabetes. The functional studies were performed with eight diabetic and six control rats at each point in time. On the day of the study, the rats were fasted overnight and then anesthetized with sodium pentobarbital (50 mg/kg, intraperitoneal injection). After completing the functional studies, a total of 8 ml whole blood was taken from the aorta. An aliquot was mixed with Na2-EDTA (final concentration 1 mg/ml) for the percent hemoglobin A1c (HbA1c) determination by immunoassay (Roche Diagnostics). The other portion of the sample was added to a test tube, where it was mixed with 1/10 of its volume of 0.11 M sodium citrate. The plasma was removed after centrifugation, in a floor-standing centrifuge, for 20 minutes at 1,700 g and 4℃ and was stored at -70℃ until assayed.
Erectile responses were elicited by electrical stimulation of the cavernous nerve as described previously.13 Stimulation parameters were 3 V at varying frequencies of 2.5~20 Hz with square wave duration of 0.2 ms for 30 sec. Both mean arterial pressure (MAP) and intracavernosal pressure (ICP) were continuously monitored during the electrical stimulation. Comparisons were made for the percent ICP/MAP and the area under the curve (AUC) corresponding to the duration of electrical stimulation.
Enzyme-linked immunosorbent assays (ELISA) were used to assess plasma concentrations of soluble intracellular adhesion molecule, e-selectin, and l-selectin (R & D Systems, Abingdon, UK). The plasma von Willebrand factor (vWF) was measured by ELISA (Diagnostica Stago, Asniéres Cedex, France). The high sensitivity C-reactive protein (hs-CRP) level was assessed by immunoturbidimetry using a Tina-quant, C-reactive protein high-sensitivity kit and a Hitachi analyzer (Roche, Laval, Quebec, Canada). Endothelin-1 (ET-1) was measured by enzyme immunoassay (Assay Designs, Ann Arbor, MI, USA). All assays were performed in duplicate and in a blinded fashion.
Data are presented as the mean±standard deviation. The significance of differences between the diabetic group and the control group was evaluated using the Mann-Whitney test. Correlations between erectile function and plasma endothelial markers were estimated by Spearman correlation analysis. Statistical significance was considered to be when p<0.05.
Fig. 1 shows the changes in body weight and blood glucose levels of the two groups. The body weight of the control rats gradually increased 2.5 fold from approximately 200 g at 14 weeks. By contrast, the body weight of the diabetic rats remained unchanged during the experimental period and was significantly less than that of the age-matched control rats. Once the rats became diabetic, the serum glucose levels were maintained in the range of 300~410 mg/dl throughout the study.
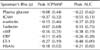
Erectile responses, expressed as percent ICP/MAP and AUC at each point in time, are shown in Table 1. Compared to the age-matched controls, there was no evidence for deterioration of the erectile function until six weeks after the induction of diabetes. Although eight weeks of diabetes was associated with the beginning of the alteration of the erectile responses, the degree of functional impairment was different based on the parameters measured. Compared to the age-matched control group, the 8-week diabetic rats began to show a significant decrease in the AUC observed at the higher frequencies of nerve stimulation (10, 20 Hz). After this time, significant differences in the AUC were observed between the diabetic group and the control group at all frequencies. By contrast, a significant reduction in the percent ICP/MAP was not observed until 12 weeks of diabetes. The differences, in both parameters, gradually increased during the course of diabetes in both the diabetic and control groups.
Six plasma markers and HbA1c were measured during the course of diabetes. There were significant differences in the tested markers between the two groups. The plasma e-selectin and vWF showed the earliest significant changes starting from four weeks of diabetes induction. The differences peaked at six and eight weeks, and declined thereafter. The intracellular adhesion molecule (ICAM) and ET-1 began to show a significant elevation beginning at eight weeks of diabetes. The plasma levels of both markers increased further during the remaining period of study. Elevated plasma hs-CRP was observed from four weeks of diabetes, and its level remained elevated throughout the study. On the other hand, the plasma level of l-selectin did not show a significant difference compared to the controls during the study. The plasma levels of HbA1c began to show significant elevations six weeks after diabetes induction; the level was further elevated, up to 10.3%, by 14 weeks of diabetes.
Table 2 shows the results of the correlation analysis of the variables of erectile function compared to various plasma markers. Except for the HbA1c, there was no significant correlation noted between the other plasma markers of endothelial injury and the variables of erectile function. A modest, but significant correlation was observed between the HbA1c and the erectile parameters (ρ=-0.18 for ICP/MAP; -0.21 for AUC).
In the current study, we described the change of reflex erectile function and several blood markers of endothelial dysfunction in rats with STZ-induced diabetes. As previously reported, the rats showed evidence of declining erectile function following the STZ injection.11,12 Compared to the age-matched controls, the diabetic rats showed a significant decrease in the ICP/MAP and AUC at the eight and twelve week assessments after the STZ injection, respectively. While the elevation of several markers of endothelial dysfunction preceded the decline of erectile function, there was no marker that showed a better correlation with erectile function than the HbA1c, which showed only a modest correlation. This is the first study to describe the biweekly changes in erectile function, in diabetic rats, in detail, and to correlate the changes with various plasma markers of endothelial dysfunction with erectile function.
One important finding of our study was that the determination of erectile function impairment depends on the tested parameters and conditions. The AUC of the diabetic rats showed significant erectile impairment as early as eight weeks; however, the ICP/MAP, which has been the most frequently used parameter in cavernosometry, showed evidence of deterioration at twelve weeks after the STZ injection. In addition, the erectile response to higher frequencies of stimulation appeared to decrease earlier than that to lower frequencies. These results suggest that a period of two to three months is needed to accurately measure the effects of STZ on ED in rats. In addition, a range of electrical stimulation during the cavernosometry is needed for appropriate assessments. The fact that changes in the AUC preceded the changes in the ICP/MAP implies that the sole use of ICP/MAP might not be adequate for the detection of changes in erectile function, and other indices of erectile function such as the AUC should be added to such evaluations. The ICP/MAP is the adjustment of peak ICP for systemic blood pressure; this index may just reflect the capability to provide a rigid erection in humans. However, other components of an erection, such as the amount of tumescence or the capability of maintaining the tumescence are important for erectile function. The AUC is the total sum of the elevated ICP during the test and might reflect the tumescence time for humans. The necessity for other indices in addition to the ICP/MAP has been suggested by others. Following the treatment with chronic sildenafil, a significant beneficial effect appeared only in the detumescence time rather than ICP/MAP.14 The reflex erection of the rat in itself does not sufficiently mirror the human response, but detailed analysis of erectile parameters, in the diabetic rat model, might provide additional insight into the human response.
Our results are not consistent with those from Melman et al,15 which have reported significant changes in ICP/MAP in as early as 1 month after STZ injection. The difference in tested species (Sprague-Dawley vs. Fischer-344) and stimulation parameters may partly explain the difference. Moreover, a difference in blood glucose control as reflected by the difference in the mean blood glucose level could be the reason. Their diabetic rats showed a higher mean blood glucose (always >400 mg/dl) levels than those from our diabetic group, which ranged 300~410 mg/dl during the period of study.
Diabetes might be associated with low-grade inflammation and subsequent endothelial dysfunction, which is characterized by decreased systemic bioactivity of NO. Since NO is also the principal molecule responsible for penile erections, it is presumed that systemic endothelial dysfunction plays an important role in diabetic ED. However, there is limited information on the temporal relationship between endothelial function and diabetic ED. Therefore, we serially measured several markers associated with endothelial function and inflammation in the rat model of diabetes. Systemic endothelial function in animals has been evaluated either by measuring vascular smooth muscle responses to various stimuli or by determining blood levels of selected compounds presumed to reflect endothelial function. Since the former method takes much more time per animal and is not suitable for generating meaningful statistical data, during a limited period of time, we chose serial assessment of several blood markers of endothelial dysfunction as potential surrogates of endothelial function. Except for l-selectin, we noted significant elevation in the plasma markers associated with endothelial activation (vWF, e-selectin, ICAM, ET-1) or inflammation (hs-CRP) in the diabetic rats, similar to the results demonstrated in human diabetic patients.16-18 However, the variable kinetics of each plasma marker made it difficult to draw any meaningful conclusion regarding the role of systemic endothelial dysfunction in the development of diabetic ED. Among four plasma markers of endothelial activation tested, elevation of the vWF and e-selectin levels was noted as early as four weeks, whereas ICAM and ET-1 showed delayed elevation, noted after eight weeks of diabetes. Furthermore, while the former markers showed a temporary elevation, the latter markers maintained their level during the remaining period of the study. These results suggest the presence of significant endothelial dysfunction in diabetic rats. However, the plasma vWF and e-selectin may be sensitive markers of endothelial dysfunction, but their transient nature is difficult to explain. In addition, the ICAM and ET-1 levels were not as sensitive to early changes in the endothelial function. The plasma level of the hs-CRP, which reflects a low-grade inflammation, remained elevated throughout the study. This finding was consistent with previous diabetic studies, and supports the presence of systemic inflammation in diabetes.19,20 The reason l-selectin showed no change is unclear; other studies have reported inconsistent results with regard to l-selectin levels in diabetic patients.21,22 Interestingly, no single plasma marker showed a meaningful correlation with erectile function. The null relationship between changes in systemic endothelial function and ED, and the inconsistent results between markers of systemic endothelial function suggest that systemic endothelial dysfunction did not seem to play a significant role in the development of ED during the early phase of diabetes. These findings also cast doubt on the role of these markers as a potential target for therapy and follow-up.
Although other explanations for diabetic ED were not evaluated in this study, multiple local etiologies have been suggested in other rat models of diabetic ED. The decreased expression of neuronal and/or endothelial nitric oxide synthase (NOS),23,24 decreased NOS activity,23 and accumulation of advanced glycation end products25 has been shown to be associated with impairment of erections. Glycation of endothelial NOS (O-linked GlcNAc modification), which leads to decreased enzyme activity, has been found in diabetic rats.26 Compared to the abovementioned local mechanisms, the significance of systemic endothelial dysfunction does not appear to be a significant factor.
Unlike other plasma markers, the amount of glycosylated hemoglobin showed a meaningful negative correlation with erectile function in diabetic rats. Hyperglycemia per se was shown to quench NO and inactivate NOS by increasing the formation of free radicals. The role of superoxide in hyperglycemic conditions is well known. It directly reacts with NO and its serum level is correlated with glycemic control. Glycosylated hemoglobin impaires endothelium-derived relaxation of the corpus cavernosum in a dose-dependent manner and superoxide dismutase completely reverses this impairment.27 Consistent with preclinical studies, a negative correlation between the levels of glycosylated hemoglobin and erectile function has been demonstrated in patients with type 2 diabetes.28 Our results confirm the importance of uncontrolled hyperglycemia in diabetic ED.
The major limitation of our study could be the absence of data on vaso-relaxation responses as a surrogate for endothelial function. Along with measurement of the blood levels of certain molecules, tests of endothelium-dependent vasomotion provide a functional test of the endothelium. The endothelium has a multitude of functions; different tests are needed to measure different aspects of endothelial function. Some studies have indicated a correlation among these functions, while others have not.29-31 Therefore, in the future, the data on vasomotion must be more specifically associated with erectile function to determine the association of endothelial dysfunction with diabetic ED.
Our observational data in a rat diabetic model showed eight weeks were needed to observe impairment of erections in STZ-injected diabetic rats. There was some evidence of systemic endothelial dysfunction in the diabetic rats, but no association with erectile function was found. These results suggest no significant role of systemic endothelial dysfunction in the development of early phase diabetic ED. However, the important role of uncontrolled hyperglycemia in diabetic ED was once again confirmed.
Figures and Tables
Fig. 1
The effect of diabetes on body weight and serum glucose concentrations. (A) The rats were weighed at regular intervals for 14 weeks. (B) Blood glucose was measured every 2 weeks. Significant elevation of blood glucose was noted within 2 weeks of streptozotocin injection. ▪: nondiabetic control animals, ▴: streptozotocin-induced diabetic rats. *Statistically significant difference from control group at each point in time (p<0.05).

Fig. 2
Serial comparison of plasma markers between control and diabetic rats. The levels were measured after the tested rats were euthanized and blood was collected. (A) Intracellular adhesion molecule (ICAM), (B) e-selectin, (C) l-selectin, (D) von Willebrand factor, (E) high sensitivity C-reactive protein (hsCRP), (F) endothelin-1 and (G) hemoglobin A1c (HbA1c). *Statistically significant difference from control group at each point in time (p<0.05).

References
1. Selvin E, Burnett AL, Platz EA. Prevalence and risk factors for erectile dysfunction in the US. Am J Med. 2007. 120:151–157.

2. Saenz de Tejada I, Goldstein I, Azadzoi K, Krane RJ, Cohen RA. Impaired neurogenic and endothelium-mediated relaxation of penile smooth muscle from diabetic men with impotence. N Engl J Med. 1989. 320:1025–1030.

3. De Angelis L, Marfella MA, Siniscalchi M, Marino L, Nappo F, Giugliano F, et al. Erectile and endothelial dysfunction in Type II diabetes: a possible link. Diabetologia. 2001. 44:1155–1160.

4. Pegge NC, Twomey AM, Vaughton K, Gravenor MB, Ramsey MW, Price DE. The role of endothelial dysfunction in the pathophysiology of erectile dysfunction in diabetes and in determining response to treatment. Diabet Med. 2006. 23:873–878.

5. Ahn GJ, Yu JY, Choi SM, Kang KK, Ahn BO, Kwon JW, et al. Chronic administration of phosphodiesterase 5 inhibitor improves erectile and endothelial function in a rat model of diabetes. Int J Androl. 2005. 28:260–266.

6. Browne DL, Meeking DR, Allard S, Munday LJ, Shaw KM, Cummings MH. Diabetic erectile dysfunction-an indicator of generalised endothelial function per se? Int J Clin Pract. 2006. 60:1323–1326.
7. Nangle MR, Cotter MA, Cameron NE. IkappaB kinase 2 inhibition corrects defective nitrergic erectile mechanisms in diabetic mouse corpus cavernosum. Urology. 2006. 68:214–218.
8. Usta MF, Kendirci M, Gur S, Foxwell NA, Bivalacqua TJ, Cellek S, et al. The breakdown of preformed advanced glycation end products reverses erectile dysfunction in streptozotocin-induced diabetic rats: preventive versus curative treatment. J Sex Med. 2006. 3:242–250.

9. Chen Y, Yang R, Yao L, Sun Z, Wang R, Dai Y. Differential expression of neurotrophins in penises of streptozotocin-induced diabetic rats. J Androl. 2007. 28:306–312.

10. Christ GJ, Hsieh Y, Zhao W, Schenk G, Venkateswarlu K, Wang HZ, et al. Effects of streptozotocin-induced diabetes on bladder and erectile (dys)function in the same rat in vivo. BJU Int. 2006. 97:1076–1082.
11. Italiano G, Marin A, Pescatori ES, Calabrò A, Artibani W, Pagano F, et al. Effect of streptozotocin-induced diabetes on electrically evoked erection in the rat. Int J Impot Res. 1993. 5:27–35.
12. Ari G, Vardi Y, Finberg JP. Nitric oxide and penile erection in streptozotocin-diabetic rats. Clin Sci (Lond). 1999. 96:365–371.

13. Park K, Ryu KS, Li WJ, Kim SW, Paick JS. Chronic treatment with a type 5 phosphodiesterase inhibitor suppresses apoptosis of corporal smooth muscle by potentiating Akt signalling in a rat model of diabetic erectile dysfunction. Eur Urol. 2008. 53:1282–1288.

14. Musicki B, Champion HC, Becker RE, Liu T, Kramer MF, Burnett AL. Erection capability is potentiated by long-term sildenafil treatment: role of blood flow-induced endothelial nitric-oxide synthase phosphorylation. Mol Pharmacol. 2005. 68:226–232.

15. Melman A, Zotova E, Kim M, Arezzo J, Davies K, DiSanto M, et al. Longitudinal studies of time-dependent changes in both bladder and erectile function after streptozotocin-induced diabetes in Fischer 344 male rats. BJU Int. 2009. 104:1292–1300.

16. Seligman BG, Biolo A, Polanczyk CA, Gross JL, Clausell N. Increased plasma levels of endothelin 1 and von Willebrand factor in patients with type 2 diabetes and dyslipidemia. Diabetes Care. 2000. 23:1395–1400.

17. Clausen P, Jacobsen P, Rossing K, Jensen JS, Parving HH, Feldt-Rasmussen B. Plasma concentrations of VCAM-1 and ICAM-1 are elevated in patients with Type 1 diabetes mellitus with microalbuminuria and overt nephropathy. Diabet Med. 2000. 17:644–649.

18. Meigs JB, Hu FB, Rifai N, Manson JE. Biomarkers of endothelial dysfunction and risk of type 2 diabetes mellitus. JAMA. 2004. 291:1978–1986.

19. Malik S, Wong ND, Franklin S, Pio J, Fairchild C, Chen R. Cardiovascular disease in U.S. patients with metabolic syndrome, diabetes, and elevated C-reactive protein. Diabetes Care. 2005. 28:690–693.

20. Thorand B, Löwel H, Schneider A, Kolb H, Meisinger C, Fröhlich M, et al. C-reactive protein as a predictor for incident diabetes mellitus among middle-aged men: results from the MONICA Augsburg cohort study, 1984-1998. Arch Intern Med. 2003. 163:93–99.
21. Kretowski A, Gillespie KM, Bingley PJ, Kinalska I. Soluble L-selectin levels in type I diabetes mellitus: a surrogate marker for disease activity? Immunology. 2000. 99:320–325.
22. Dursun H, Cinaz P, Bideci A, Guven A, Aybay C, Elbeg S. Serum levels of sL-selectin and tumour necrosis factor-alpha in children with type 1 diabetes mellitus. Acta Diabetol. 2007. 44:1–5.
23. Bivalacqua TJ, Champion HC, Usta MF, Cellek S, Chitaley K, Webb RC, et al. RhoA/Rho-kinase suppresses endothelial nitric oxide synthase in the penis: a mechanism for diabetes-associated erectile dysfunction. Proc Natl Acad Sci U S A. 2004. 101:9121–9126.

24. Cellek S, Rodrigo J, Lobos E, Fernández P, Serrano J, Moncada S. Selective nitrergic neurodegeneration in diabetes mellitus - a nitric oxide-dependent phenomenon. Br J Pharmacol. 1999. 128:1804–1812.
25. Seftel AD, Vaziri ND, Ni Z, Razmjouei K, Fogarty J, Hampel N, et al. Advanced glycation end products in human penis: elevation in diabetic tissue, site of deposition, and possible effect through iNOS or eNOS. Urology. 1997. 50:1016–1026.

26. Musicki B, Kramer MF, Becker RE, Burnett AL. Inactivation of phosphorylated endothelial nitric oxide synthase (Ser-1177) by O-GlcNAc in diabetes-associated erectile dysfunction. Proc Natl Acad Sci U S A. 2005. 102:11870–11875.
27. Cartledge JJ, Eardley I, Morrison JF. Impairment of corpus cavernosal smooth muscle relaxation by glycosylated human haemoglobin. BJU Int. 2000. 85:735–741.

28. Rhoden EL, Ribeiro EP, Riedner CE, Teloken C, Souto CA. Glycosylated haemoglobin levels and the severity of erectile function in diabetic men. BJU Int. 2005. 95:615–617.

29. Głowińska-Olszewska B, Tołwińska J, Urban M. Relationship between endothelial dysfunction, carotid artery intima media thickness and circulating markers of vascular inflammation in obese hypertensive children and adolescents. J Pediatr Endocrinol Metab. 2007. 20:1125–1136.

30. Lupattelli G, Lombardini R, Schillaci G, Ciuffetti G, Marchesi S, Siepi D, et al. Flow-mediated vasoactivity and circulating adhesion molecules in hypertriglyceridemia: association with small, dense LDL cholesterol particles. Am Heart J. 2000. 140:521–526.

31. van Haelst PL, van Doormaal JJ, Asselbergs FW, van Roon AM, Veeger NJ, Henneman MM, et al. Correlates of endothelial function and their relationship with inflammation in patients with familial hypercholesterolaemia. Clin Sci (Lond). 2003. 104:627–632.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download