Abstract
Methods
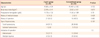
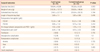
We retrospectively analyzed medical records of patients undergoing hysterectomy between March 2011 and February 2012. Patients were stratified into two groups by surgical approach. Clinical features and surgical outcomes were compared.
Results
Of a total of 68 laparoscopic hysterectomy, 35 (51.5%) were two-port laparoscopy, 33 (48.5%) were conventional laparoscopy. The weight of uterus were heavier in the conventional laparoscopic hysterectomy group (338.06 ± 148.44 g) than in the two-port laparoscopic (318.38 ± 137.73 g) group but there were no significant differences (P=0.572). Estimate blood loss was reported in the two-port and conventional laparoscopic group with blood loss of 314.0 ± 227.18 mL, 293.64 ± 282.35 mL (P=0.744). Actual surgical time was 194.94 ± 46.08 minutes in the two-port, 195.36 ± 54.28 minutes in the conventional (P=0.973). Patients in the two-port group had similar length of hospital stay of 5.69 ± 1.1 days as compared to 5.85 ± 0.8 days in the conventional group (P=0.476) but there were no significant differences. Immediate postoperative pain by using a visual analogue scale was 4.49 ± 1.56 point in the two-port group, 4.55 ± 2.03 point in the conventional laparoscopic group (P=0.892).
Conclusion
Two-port group is a feasible method with comparable operative outcomes including operative time, blood loss, weight of uterus, postoperative pain, and hospital stay when compared with the conventional laparoscopic hysterectomy. Therefore two-port laparoscopic hysterectomy may replace the role of conventional laparoscopic hysterectomy.
Figures and Tables
 | Fig. 1Picture of Glove Port (Nelis), multichannel port. (A) Front aspect. (B) Glove Port was inserted on umbilical area. (C) Longitudinal aspect. |
References
1. Johnson N, Barlow D, Lethaby A, Tavender E, Curr E, Garry R. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev. 2006. (2):CD003677.
2. Kluivers KB, Hendriks JC, Mol BW, Bongers MY, Bremer GL, de Vet HC, et al. Quality of life and surgical outcome after total laparoscopic hysterectomy versus total abdominal hysterectomy for benign disease: a randomized, controlled trial. J Minim Invasive Gynecol. 2007. 14:145–152.
3. Yi SW, Park HM, Lee SS, Park SM, Lee HM, Sohn WS. Two-port total laparoscopic hysterectomy with a multichannel port. J Laparoendosc Adv Surg Tech A. 2009. 19:223–228.
4. Pelosi MA, Pelosi MA 3rd. Laparoscopic hysterectomy with bilateral salpingo-oophorectomy using a single umbilical puncture. N J Med. 1991. 88:721–726.
5. Jung YW, Lee M, Yim GW, Lee SH, Paek JH, Kwon HY, et al. A randomized prospective study of single-port and four-port approaches for hysterectomy in terms of postoperative pain. Surg Endosc. 2011. 25:2462–2469.
6. Leung KF, Lee KW, Cheung TY, Leung LC, Lau KW. Laparoscopic cholecystectomy: two-port technique. Endoscopy. 1996. 28:505–507.
7. Poon CM, Chan KW, Lee DW, Chan KC, Ko CW, Cheung HY, et al. Two-port versus four-port laparoscopic cholecystectomy. Surg Endosc. 2003. 17:1624–1627.
8. Ghezzi F, Cromi A, Colombo G, Uccella S, Bergamini V, Serati M, et al. Minimizing ancillary ports size in gynecologic laparoscopy: a randomized trial. J Minim Invasive Gynecol. 2005. 12:480–485.
9. Paek J, Nam EJ, Lee M, Yim GW, Kim S, Kim YT, et al. Two-port access versus conventional staging laparoscopy for endometrial cancer. Int J Gynecol Cancer. 2012. 22:515–520.
10. Jeon YE, Paek J, Nam EJ, Kim YT, Kim SW. Two-port access Laparoscopic radical hysterectomy: first clinical report. J Womens Med. 2010. 3:18–22.
11. Yoon BS, Park H, Seong SJ, Park CT, Jun HS, Kim IH. Single-port versus conventional laparoscopic salpingectomy in tubal pregnancy: a comparison of surgical outcomes. Eur J Obstet Gynecol Reprod Biol. 2011. 159:190–193.
12. Jung YW, Kim YT, Lee DW, Hwang YI, Nam EJ, Kim JH, et al. The feasibility of scarless single-port transumbilical total laparoscopic hysterectomy: initial clinical experience. Surg Endosc. 2010. 24:1686–1692.
13. Yim GW, Jung YW, Paek J, Lee SH, Kwon HY, Nam EJ, et al. Transumbilical single-port access versus conventional total laparoscopic hysterectomy: surgical outcomes. Am J Obstet Gynecol. 2010. 203:26.e1–26.e6.
14. Kim TJ, Lee YY, Cha HH, Kim CJ, Choi CH, Lee JW, et al. Single-port-access laparoscopic-assisted vaginal hysterectomy versus conventional laparoscopic-assisted vaginal hysterectomy: a comparison of perioperative outcomes. Surg Endosc. 2010. 24:2248–2252.
15. Lee WJ. Single port laparoscopic surgery. J Korean Med Assoc. 2010. 53:793–806.
16. Alexander JI, Hull MG. Abdominal pain after laparoscopy: the value of a gas drain. Br J Obstet Gynaecol. 1987. 94:267–269.
17. Korell M, Schmaus F, Strowitzki T, Schneeweiss SG, Hepp H. Pain intensity following laparoscopy. Surg Laparosc Endosc. 1996. 6:375–379.
18. Sharp JR, Pierson WP, Brady CE 3rd. Comparison of CO2- and N2O-induced discomfort during peritoneoscopy under local anesthesia. Gastroenterology. 1982. 82:453–456.
19. Vitale GC, Collet D, Larson GM, Cheadle WG, Miller FB, Perissat J. Interruption of professional and home activity after laparoscopic cholecystectomy among French and American patients. Am J Surg. 1991. 161:396–398.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download